| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg | |||
| Other Sizes |

| 靶点 |
IP Receptor ( EC50 = 1.9 nM ); TP Receptor ( EC50 = 919 nM ); IP Receptor ( Ki = 32.1 nM ); FP Receptor ( Ki = 4680 nM ); DP1 ( EC50 = 0.6±0.1 nM ); EP2 ( EC50 = 6.2±1.2 nM ); DP1 ( EC50 = 4.4 nM ); EP2 ( EC50 = 3.6 nM ); EP4 ( EC50 = 826 nM ); EP3 ( EC50 = 2505 nM ); EP1 ( Ki = 212 nM ); EP1 ( EC50 = 285 nM ); EP3 ( EC50 = 68.9 nM ); EP4 ( EC50 = 181 nM )
- Prostacyclin receptor (IP):Treprostinil acts as a potent agonist with a Ki value of 0.3 nM. [1] - Prostaglandin DP1 receptor (DP1):Treprostinil exhibits high agonist activity with a Ki value of 0.14 nM. [1] - Prostaglandin EP2 receptor (EP2):Treprostinil is a potent agonist with a Ki value of 0.7 nM. [1] |
|---|---|
| 体外研究 (In Vitro) |
曲前列环素对 DP1、EP2 和 IP 受体具有高亲和力(Ki 分别为 4.4、3.6 和 32 nM),对 EP1 和 EP4 受体亲和力低,对 EP3、FP 和 TP 受体亲和力更低。与曲前列环素一样,IP、DP1 和 EP2 受体的激活均可导致人肺动脉血管舒张[1]。曲前列环素抑制培养的内皮集落形成细胞的活力。来自曲前列环素预处理的间充质干细胞的条件培养基刺激内皮集落形成细胞增殖[5]。
- 受体结合与激活: - 曲前列尼尔对IP、DP1和EP2受体具有纳摩尔级亲和力,其中对DP1的亲和力最高(Ki = 0.14 nM)。它通过激活这些受体诱导cAMP生成,从而发挥血管舒张和抗增殖作用。[1] - 间充质干细胞(MSCs)中VEGF-A的诱导: - 曲前列尼尔(10–100 nM)通过激活IP和DP1受体显著增加MSCs中VEGF-A的分泌。该效应可被特异性拮抗剂阻断,证实为受体介导的信号通路。[2] |
| 体内研究 (In Vivo) |
吸入曲前列环素钠是一种前列环素类似物,是最新获得 FDA 批准用于治疗致命孤儿疾病:肺动脉高压 (PAH) 的药物[2]。与安慰剂相比,曲前列环素可保留窦内皮细胞内层并减少移植后早期血小板沉积。安慰剂组肝组织血流明显受损,而曲前列环素则维持与正常水平相似的血流[3]。曲前列环素治疗显着增加裸鼠基质胶中内皮集落形成细胞联合间充质干细胞的血管形成能力。沉默间充质干细胞中的 VEGF-A 基因也会阻断曲前列环素的促血管生成作用[4]。曲前列环素在提高小鼠和人类造血干细胞和祖细胞的细胞内 cAMP 水平方面最有效[5]。与常氧小鼠相比,曲前列环素治疗显着减少了细胞的募集。曲前列环素还可降低右心室收缩压并略微减少血管重塑,但无法逆转右心室肥厚[6]。
- 肺动脉高压(PAH)治疗: - 在PAH动物模型(如慢性低氧诱导的大鼠)中,曲前列尼尔通过吸入或皮下输注给药可降低肺血管阻力并改善右心室功能。其治疗作用归因于IP和DP1受体的双重激活,导致血管舒张和抑制纤维细胞募集。[3][6] - 缺血再灌注损伤保护: - 在大鼠原位肝移植模型中,曲前列尼尔(10–50 ng/kg/min,静脉注射)通过抑制氧化应激和中性粒细胞浸润减轻肝损伤。该效应与内皮型一氧化氮合酶(eNOS)活性增加和促炎细胞因子释放减少相关。[5] - 增强造血祖细胞移植: - 在小鼠模型中,曲前列尼尔(0.1–1 mg/kg,腹腔注射)通过促进造血干细胞向骨髓迁移改善移植植入。这一过程由祖细胞表面CXCR4趋化因子受体表达上调介导。[4] |
| 酶活实验 |
- 前列腺素受体结合实验:
1. 将转染人IP、DP1或EP2受体的HEK293细胞膜制剂与放射性标记配体(如用于IP的[³H]-伊洛前列素)在不同浓度的曲前列尼尔(0.01–100 nM)存在下孵育。
2. 通过过滤分离结合和游离配体,测量放射性以确定Ki值。曲前列尼尔以高效力置换[³H]-伊洛前列素,IP(Ki = 0.3 nM)和DP1(Ki = 0.14 nM)。[1]
|
| 细胞实验 |
将来自人类或小鼠的造血干细胞和祖细胞在 37°C 下在载体存在下或与 10 μM 曲前列环素和 30 μM 毛喉素联合培养一小时和二十四小时。细胞凋亡试剂盒用于在 4°C 下用磷酸盐缓冲盐水洗涤细胞后对细胞进行外化磷脂酰丝氨酸染色 [5]。
- MSCs中VEGF-A分泌实验: 1. 将MSCs在无血清培养基中用曲前列尼尔(10–100 nM)处理24小时。 2. 收集条件培养基,通过ELISA定量VEGF-A水平。曲前列尼尔以浓度依赖方式增加VEGF-A分泌(EC50 ≈ 50 nM)。[2] - 内皮集落形成细胞(ECFC)血管生成实验: 1. 将ECFCs与曲前列尼尔处理的MSCs在Matrigel中共培养。 2. 12小时后评估管形成。曲前列尼尔使ECFC血管生成芽数比对照组增加2–3倍,依赖于MSCs分泌的VEGF-A。[2] |
| 动物实验 |
Rats: For the study, male Lewis rats weighing between 200 and 300 g are employed. 24 hours prior to hepatectomy, donor animals are given treprostinil or a placebo, and the corresponding recipient animal receives the same care until the moment of sacrifice. Treatment is invisible to the surgeon. To study what happens right after IRI, recipients are sacrificed 1, 3, 6, 24 and 48 hours after transplantation. Using an Alzet implantable osmotic pump, subcutaneous administration of treprostinil (100 ng/kg/min) or placebo is performed. This dosage is chosen to produce a plasma concentration that is steady-state and falls between 5 and 20 ng/mL[3].
Mice: Mice that have had bone marrow transplantation (BMT) are split up into five groups, each with six to ten mice. In a normobaric chamber, one group of mice is exposed to hypoxia (10% inspired oxygen fraction), while the other group of mice (control BMT) spends 28 days in a normoxic chamber with a normal oxygen environment (21% inspired O2 fraction). While the two other groups of mice receive four weeks of hypoxic exposure and receive Treprostinil infusions at varying dose levels (14 ng/kg and 70 ng/kg per minute), the sham group mice receive saline treatment. Comparatively, infusion rates for humans in PAH therapy range from 10 to 60 ng/kg per minute[6]. - Chronic hypoxic PAH model: 1. Rats are exposed to hypoxia (10% O₂) for 4 weeks to induce PAH. 2. Treprostinil is administered via subcutaneous osmotic pumps (10–50 ng/kg/min) or inhaled aerosol (1–5 μg/kg) daily for 2 weeks. 3. Pulmonary hemodynamics are measured via right heart catheterization, and lung tissues are analyzed for fibrocyte infiltration (CD45⁺/collagen I⁺ cells). [6] - Liver transplantation model: 1. Rats undergo orthotopic liver transplantation with 60-minute warm ischemia. 2. Treprostinil (10–50 ng/kg/min) is infused intravenously starting 30 minutes before reperfusion and continuing for 6 hours postoperatively. 3. Liver function is assessed by serum alanine aminotransferase (ALT) levels, and histological damage is evaluated by hematoxylin-eosin staining. [5] |
| 药代性质 (ADME/PK) |
- Subcutaneous/intravenous administration:
- Treprostinil is rapidly absorbed with a bioavailability of ~90%. Plasma protein binding is ~90%, primarily to albumin. The terminal half-life is 3–4 hours, and elimination occurs via hepatic metabolism (CYP3A4-mediated oxidation) and renal excretion. [3]
- Inhaled administration: - Inhaled Treprostinil achieves peak plasma concentrations within 10–15 minutes, with a bioavailability of ~20–30%. The inhaled route reduces systemic exposure compared to parenteral administration, minimizing off-target effects. [3] |
| 毒性/毒理 (Toxicokinetics/TK) |
Effects During Pregnancy and Lactation
◉ Summary of Use during Lactation One patient taking treprostinil breastfed her infant for one year without any complications. However, until more data are available, treprostinil should only be used with careful monitoring during breastfeeding. ◉ Effects in Breastfed Infants A woman developed pulmonary artery hypertension and was treated with intravenous treprostinil beginning at 32 weeks of gestation and titrated up to 26 ng/kg/min. The dose was nearly doubled postpartum because of worsening symptoms. She breastfed (extent not stated) her infant for one year with no apparent drug-related problems, although there was concern for obesity at 6 months of age. The infant was healthy and developing normally at 2 years of age. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. - Side effects: - Common adverse effects include headache, flushing, and jaw pain, attributed to vasodilation. At higher doses, Treprostinil may cause hypotension, nausea, and diarrhea. [3] - Plasma protein binding: - Treprostinil is highly bound to plasma proteins (~90%), which may increase drug-drug interactions with other highly protein-bound compounds (e.g., warfarin). [3] |
| 参考文献 |
|
| 其他信息 |
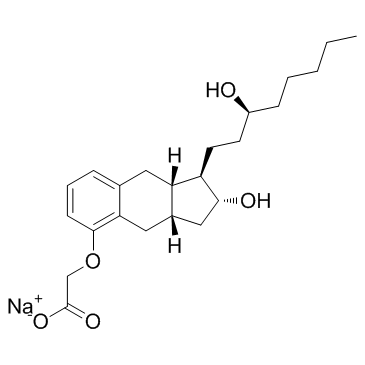
Treprostinil sodium is an organic sodium salt. It contains a treprostinil.
Drug Indication Treatment of adult patients with WHO Functional Class (FC) III or IV and: inoperable chronic thromboembolic pulmonary hypertension (CTEPH), orpersistent or recurrent CTEPH after surgical treatmentto improve exercise capacity. Treatment of pulmonary arterial hypertension Treatment of chronic thromboembolic pulmonary hypertension - Mechanism of action: - Treprostinil exerts its therapeutic effects through dual activation of IP and DP1 receptors, leading to vasodilation, inhibition of platelet aggregation, and suppression of vascular remodeling. Its activation of EP2 receptors may also contribute to anti-inflammatory effects. [1][6] - Clinical use: - Approved for the treatment of pulmonary arterial hypertension (PAH) and chronic thromboembolic pulmonary hypertension (CTEPH). Available in multiple formulations: subcutaneous/intravenous solution, inhaled aerosol, and oral tablets. [3] - FDA-approved indications: - Treprostinil is indicated for improving exercise capacity and delaying clinical worsening in patients with PAH. The inhaled formulation is specifically approved for patients with severe symptoms (WHO functional class III/IV). [3] |
| 分子式 |
C23H33NAO5
|
|---|---|
| 分子量 |
412.4949
|
| 精确质量 |
412.22
|
| 元素分析 |
C, 66.97; H, 8.06; Na, 5.57; O, 19.39
|
| CAS号 |
289480-64-4
|
| 相关CAS号 |
Treprostinil;81846-19-7; Treprostinil diethanolamine; 830354-48-8
|
| PubChem CID |
23663413
|
| 外观&性状 |
White to off-white solid powder
|
| 密度 |
587.1ºC at 760 mmHg
|
| 沸点 |
587.1ºC at 760 mmHg
|
| 闪点 |
199.3ºC
|
| 蒸汽压 |
1.25E-14mmHg at 25°C
|
| LogP |
3.583
|
| tPSA |
86.99
|
| 氢键供体(HBD)数目 |
2
|
| 氢键受体(HBA)数目 |
5
|
| 可旋转键数目(RBC) |
10
|
| 重原子数目 |
29
|
| 分子复杂度/Complexity |
502
|
| 定义原子立体中心数目 |
5
|
| SMILES |
[Na+].O([H])C1([H])C([H])([H])[C@]2([H])C([H])([H])C3C(=C([H])C([H])=C([H])C=3C([H])([H])[C@@]2([H])C1([H])C([H])([H])C([H])([H])C([H])(C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])[H])O[H])OC([H])([H])C(=O)[O-]
|
| InChi Key |
IQKAWAUTOKVMLE-ZSESPEEFSA-M
|
| InChi Code |
InChI=1S/C23H34O5.Na/c1-2-3-4-7-17(24)9-10-18-19-11-15-6-5-8-22(28-14-23(26)27)20(15)12-16(19)13-21(18)25;/h5-6,8,16-19,21,24-25H,2-4,7,9-14H2,1H3,(H,26,27);/q;+1/p-1/t16-,17-,18+,19-,21+;/m0./s1
|
| 化学名 |
sodium;2-[[(1R,2R,3aS,9aS)-2-hydroxy-1-[(3S)-3-hydroxyoctyl]-2,3,3a,4,9,9a-hexahydro-1H-cyclopenta[g]naphthalen-5-yl]oxy]acetate
|
| 别名 |
UT-15; LRX 15 sodium; UT 15; LRX15 sodium; UT15; LRX-15 sodium; BW 15AU sodium; U-62840 sodium; Uniprost; Treprostinil; Orenitram; Remodulin; Treprostinil (sodium); 7JZ75N2NT6; TREPROSTINIL SODIUM SALT; CHEBI:50863; sodium;2-[[(1R,2R,3aS,9aS)-2-hydroxy-1-[(3S)-3-hydroxyoctyl]-2,3,3a,4,9,9a-hexahydro-1H-cyclopenta[g]naphthalen-5-yl]oxy]acetate;
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO: 25~82 mg/mL (~198.8 mM)
Water: 82 mg/mL Ethanol: 82 mg/mL |
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (6.06 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (6.06 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (6.06 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 配方 4 中的溶解度: 50 mg/mL (121.22 mM) in PBS (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶. 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.4243 mL | 12.1215 mL | 24.2430 mL | |
| 5 mM | 0.4849 mL | 2.4243 mL | 4.8486 mL | |
| 10 mM | 0.2424 mL | 1.2122 mL | 2.4243 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT03045029 | Active Recruiting |
Drug: Oral treprostinil | Pulmonary Arterial Hypertension | United Therapeutics | July 18, 2017 | N/A |
| NCT05176951 | Active Recruiting |
Drug: Treprostinil Palmitil Drug: Placebo |
Pulmonary Hypertension | Insmed Incorporated | December 22, 2022 | Phase 2 |
| NCT05060315 | Active Recruiting |
Combination Product: Remunity Pump for Remodulin |
Pulmonary Arterial Hypertension | United Therapeutics | July 5, 2023 | N/A |
| NCT03835676 | Recruiting | Drug: Treprostinil | Pulmonary Hypertension | Magdi H. Yacoub | May 1, 2019 | Phase 4 |
| NCT04005469 | Recruiting | Drug: Treprostinil | Ischemia Reperfusion Injury Delayed Graft Function |
Rhode Island Hospital | November 13, 2020 | Phase 1 Phase 2 |
|
|
|
|
|