| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| Other Sizes |
|
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Both vitamin D2 & vitamin D3 are absorbed from the small intestine, although vitamin D3 may be absorbed more efficiently. The exact portion of the gut that is most effective in vitamin D absorption reflects the vehicle in which the vitamin is dissolved. Most of the vitamin appears first within chylomicrons in lymph. The presence of bile is required for absorption of ergocalciferol and the extent of GI absorption may be decreased in patients with hepatic, biliary, or GI disease (e.g., Crohn's disease, Whipple's disease, sprue). A longitudinal, randomized, double blind, placebo controlled study was conducted for 6 months to monitor ultraviolet B light exposure in human milk-fed infants both with and without supplemental vitamin D2, and to measure longitudinally the bone mineral content, growth, and serum concentrations of calcium, phosphorus, 25-hydroxyvitamin D3, 25-hydroxyvitamin D2, 1,25-dihydroxyvitamin D, and parathyroid hormone. Sequential sampling was performed of 46 human milk-fed white infants; 24 received 400 IU/day of vitamin D2, and 22 received placebo. An additional 12 patients were followed who received standard infant formula. 83% of patients completed a full 6 months of the study. Ultraviolet B light exposure and measurements of growth did not differ between groups. At 6 months, the human milk groups did not differ significantly in bone mineral content or serum concentrations of parathyroid hormone or 1,25-dihydroxyvitamin D, although total 25-hydroxyvitamin D values were significantly less in the unsupplemented human milk group (23.53 + or - 9.94 vs 36.96 + or - 11.86 ng/ml; p< 0.01). However, 25-hydroxyvitamin D3 serum concentrations were significantly higher in the unsupplemented human milk-fed group compared with the supplemented group (21.77 + or - 9.73 vs 11.74 + or - 10.27 ng/ml, p< 0.01) by 6 months of age. It was concluded that unsupplemented, human milk-fed infants had no evidence of vitamin D deficiency during the first 6 months of life. A comparison was made of the ability of ergocalciferol and cholecalciferol to elevate plasma concentrations of vitamin D and 25-hydroxyvitamin D in cats. Cholecalciferol, given as an oral bolus in oil, resulted in a rapid elevation of plasma concentration of cholecalciferol followed by a rapid decline. In contrast, 25-hydroxyvitamin D concentration in plasma increased until day 3 after administration and remained elevated for a further 5 days. When 337 microg of both cholecalciferol and ergocalciferol in oil were given as an oral bolus to 10 cats, the peak plasma concentrations of cholecalciferol and ergocalciferol occurred at 8 or 12 h after administration. Peak concentrations of cholecalciferol were over twice those of ergocalciferol (570 +/- 80 vs. 264 +/- 42 nmol/l). The area under the curve 0-169 h for cholecalciferol was also more than twice that for ergocalciferol. When ergocalciferol and cholecalciferol were administered in a parenteral oil-based emulsion, higher concentrations of 25-hydroxyvitamin D3 than 25-hydroxyvitamin D2 were maintained in plasma. When both vitamins were included in the diet in the nutritional range, plasma concentrations of 25-hydroxyvitamin D2 were 0.68 of those of 25-hydroxyvitamin D3. Discrimination against ergocalciferol by cats appears to result from differences in affinity of the binding protein for the metabolites of the two forms of vitamin D. These results indicate that cats discriminate against ergocalciferol, and use it with an efficiency of 0.7 of that of cholecalciferol to maintain plasma 25-hydroxyvitamin D concentration. Osteoporosis diminishes the quality of life in adults with cystic fibrosis (CF). Vitamin D deficiency resulting from malabsorption may be a factor in the etiology of low bone mineral density (BMD) in patients with CF. OBJECTIVE: Absorption of oral ergocalciferol (vitamin D2) and the consequent response of 25-hydroxyvitamin D in 10 adults with CF and exocrine pancreatic insufficiency was compared with that of 10 healthy control subjects. DESIGN: In this pharmacokinetic study, CF patients and control subjects were pair-matched on age, sex, and race. Each subject consumed 2500 microg oral vitamin D2 with a meal. The CF group also took pancreatic enzymes that provided > or = 80000 U lipase. Blood samples were obtained at baseline and at 5, 10, 24, 30, and 36 h after vitamin D2 consumption to measure serum vitamin D2 and 25-hydroxyvitamin D concentrations. RESULTS: Vitamin D2 concentrations in all subjects were near zero at baseline. CF patients absorbed less than one-half the amount of oral vitamin D2 that was absorbed by control subjects (P < 0.001). Absorption by the CF patients varied greatly; 2 patients absorbed virtually no vitamin D2. The rise in 25-hydroxyvitamin D in response to vitamin D2 absorption was significantly lower over time in the CF group than in the control group (P = 0.0012). CONCLUSIONS: Vitamin D2 absorption was significantly lower in CF patients than in control subjects. These results may help explain the etiology of vitamin D deficiency in CF patients, which may contribute to their low BMD. Metabolism / Metabolites Vitamin D ... is hydroxylated at the 25 position in liver to produce 25-hydroxy-vitamin D3 which is the major metabolite circulating in the plasma. The metabolite is further hydroxylated in the kidney to 1,25-dihydroxy-vitamin D3, the most active metabolite in initiating intestinal transport of calcium & phosphate & mobilization of mineral from bone. A polar, biologically active metabolite of vitamin D2, 25-hydroxyergocalciferol, which is about 1.5 times more active in curing rickets in rats, has been isolated from pig plasma. Dihydrotachysterol is a vitamin D analog that may be regaurded as a reduction product of vitamin D2 ... Dihydrotachysterol is about 1/450 as active as vitamin D in the antirachitic assay, but at high doses it is much more effective than vitamin D in mobilizing bone mineral. Biological Half-Life 19 to 48 hours (however, stored in fat deposits in body for prolonged periods). |
|---|---|
| 毒性/毒理 (Toxicokinetics/TK) |
Effects During Pregnancy and Lactation
◉ Summary of Use during Lactation Vitamin D is a normal component of human milk. Daily maternal vitamin D2 or D3 supplementation in the 10 to 50 mcg (400 to 2,000 IU) range produces milk concentrations that are inadequate to deliver the daily requirement to an exclusively breastfed infant, and inadequate to correct pre-existing infant vitamin D deficiency through breastfeeding alone. Breastfeeding mothers who take vitamin D supplements in this range should give their infants a daily vitamin D supplement of at least 10 mcg (400 IU) to meet pediatric nutritional guidelines. Daily maternal vitamin D dosages at or above 100 mcg (4,000 IU) achieve milk levels can potentially meet the 10 mcg daily infant goal intake, depending on the mother's underlying vitamin D status and daily infant milk intake. Obese mothers may have higher requirements. ◉ Effects in Breastfed Infants Maternal daily doses of 400 to 6,400 IU (10 to 160 mcg) have not been associated with any short-term biochemical abnormalities in breastfed infants. An 11-day-old, exclusively breastfed, term, female neonate experienced asymptomatic, mild hypercalcemia (total serum calcium 11.4 mg/dL). The mother was taking maintenance vitamin D2 100,000 IU daily to maintain normal calcium and phosphorus status after a pre-pregnancy thyroid-parathyroidectomy, plus a prenatal vitamin containing 400 IU daily vitamin D (form not specified) during pregnancy and lactation. Vitamin D2 and 25-OH-vitamin D2 levels in cord blood and in milk at 14 days of age were both markedly elevated. Serum vitamin D levels were not measured in the infant. The combination of high daily breastmilk vitamin D2 intake plus a high infant serum level present at birth likely contributed to the abnormal calcium value. In a study in northern India, short-term maternal use of oral 60,000 IU vitamin D3 once daily for 10 days beginning after birth was not associated with any differences in serum calcium or phosphorus levels, or of urinary calcium/creatinine ratios, in their exclusively breastfed infants at 14 weeks and 6 months of age compared to infants of mothers given placebo. Infants of mothers given vitamin D had a lower frequency of biochemical rickets compared to placebo (0 vs 17%), but no difference in the frequency of radiological rickets (3.6% vs 3.4%). One hundred fifty-two mothers in northern India, most of whom were vitamin D deficient, were randomized to receive 120,000 IU (3000 mcg) of vitamin D one time within 7 days postpartum followed by the same dose at 6, 10, and 14 weeks postpartum to coincide with scheduled infant immunization, or placebo. Infants of mothers in the placebo group received 400 IU (10 mcg) of daily vitamin D while those in the treatment group received placebo. At 14 weeks, infant growth parameters and serum biochemical indicators of bone mineral and liver homeostasis were similar between the two groups. At 9 months, dental growth and diarrheal or respiratory illness frequency were also not different. One hundred fourteen vitamin D deficient mothers in northern India were randomized to receive vitamin D3 60,000 IU (1,500 mcg) or placebo as a single dose starting between 24 and 48 hours after delivery, and then repeated at 6, 10, and 14 weeks postpartum. Over 90% of participants were exclusively breastfeeding. At 6 months of age, 6 infants in the control group and no infants in the treatment group developed biochemical rickets, while 2 infants and 1 infant, respectively, developed radiological rickets. Infants of mothers in the treatment group reportedly had normal serum calcium and phosphorus concentrations at 6 months of age, although specific results were not given, and this outcome was not reported for the control group. One hundred ninety mothers in Qatar were randomized to receive either 600 IU or 6000 IU vitamin D beginning within 4 weeks postpartum. Infants of the mothers in the low-dose group were given 400 IU daily while those in the high-dose group received daily placebo. At the scheduled 4- and 7-month postpartum study visits, infant growth parameters, serum calcium and parathyroid hormone levels, and parent reported infant health status, were not different between the two groups. Two hundred twenty healthy, non-obese, breastfeeding mothers in Rajasthan, India were randomized to receive 120,000 IU or 12,000 IU of vitamin D3 once a month for 12 months beginning in the first postpartum month. Infants in both groups had normal serum calcium, phosphate, and alkaline phosphate levels at baseline and at 12 months. There was no significant differences in growth parameters, bone mineral content or density between the two groups at 12 months. One thousand three hundred pregnant women in Dhaka, Bangladesh were randomized to receive an oral tablet of 4,200 IU, 16,800 IU, 28,000 IU of vitamin D3, or placebo once weekly beginning prenatally between 17- and 24-weeks gestational age. The placebo group and some in the 28,000 IU group continued to receive their assigned treatment for 26 weeks postpartum while the others stopped treatment after delivery. Baseline maternal vitamin D status was similar across all participants with 65% being biochemically vitamin D deficient. The median duration of exclusive breastfeeding was 12 to 14 weeks and was similar between each of the groups. Infant vitamin D supplementation was uncommon (<10%). One thousand one hundred sixty-four infants were available for analysis. There were no differences between the groups in infant growth at 1 year postpartum. There were also no differences in infant mortality, hospitalizations, respiratory tract infections, serum calcium status, or early childhood bone mineral density and grip strength. Infant hypercalcemia and hypercalciuria occurred rarely (≤1%) and did not differ between groups. Radiologically confirmed rickets occurred in 4 infants (0.3%), 3 in the placebo group and 1 in the lowest dose group. However, a difference between the groups could not be determined due to such a low incidence. The frequency of infant biochemical rickets at 6 months of age was significantly higher in the placebo group (7.9%) compared to the high-dose group (1.3%), but not compared to the other groups. One hundred forty-eight exclusively breastfeeding postpartum patients were given either 400 or 6,400 IU daily of vitamin D3 beginning within 4 to 6 weeks of delivery. Average baseline infant serum 25-OH-vitamin D was <50 nmol/L (range undetectable to 113.8 nmol/L). Infants of mothers in the 400 IU daily group were given a 400 IU daily vitamin D supplement, while those in the 6,400 IU daily group were given placebo. There were no differences between the two groups in biochemical markers of calcium status, bone mineral content or density at 1, 4, or 7 months of age. Emerging evidence suggests adequate infant delivery of vitamin D through breastmilk from maternal supplementation during pregnancy and lactation is important for regulation of the developing infant immune system. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. |
| 其他信息 |
Ergocalciferol appears as odorless white crystals. Used as a dietary supplement and food additive. (EPA, 1998)
5,6-trans-Vitamin D2 is a vitamin D. 5,6-trans-Vitamin D2 has been reported in Humulus lupulus and Homo sapiens with data available. See also: Ergocalciferol (annotation moved to). Mechanism of Action The mechanism of action of calcitriol, the activated form of vitamin D, resembles that of the steroid and thyroid hormones. Thus, calcitriol binds to cytosolic receptors within target cells, and the receptor-hormone complex interacts with the DNA of certain genes to either enhance or inhibit their transcription. Structural analysis of the calcitriol receptor indicates that it belongs to the same supergene family as the steroid receptors. Calcitriol also appears to exert a few effects that occur too rapidly to be explained by genomic actions. /Calcitriol/ The mechanisms responsible for mobilization of bone salts have been only partially defined, and the interaction of multiple factors appears to be involved. Paradoxically, the cells responsible for bone resorption (osteoclasts) are not directly acted upon by calcitriol and do not appear to contain calcitriol receptors. Instead, calcitriol causes an increase in the number of osteoclasts available to resorb bone; this may result from an action upon myeloid hematopoietic precursor cells that are induced to differentiate toward functional osteoclasts. The cells responsible for bone formation (osteoblasts) do contain receptors, and calcitriol causes them to elaborate several proteins, including osteocalcin, a vitamin K-dependent protein that contains gamma-carboxyglutamic acid residues. The exact role of this protein is not known, but other unidentified substances are also elaborated that appear to stimulate the function of osteoclasts. In addition, calcitriol acts synergistically with gamma-interferon to increase the production of interleukin-1, a lymphokine that promotes bone resorption. |
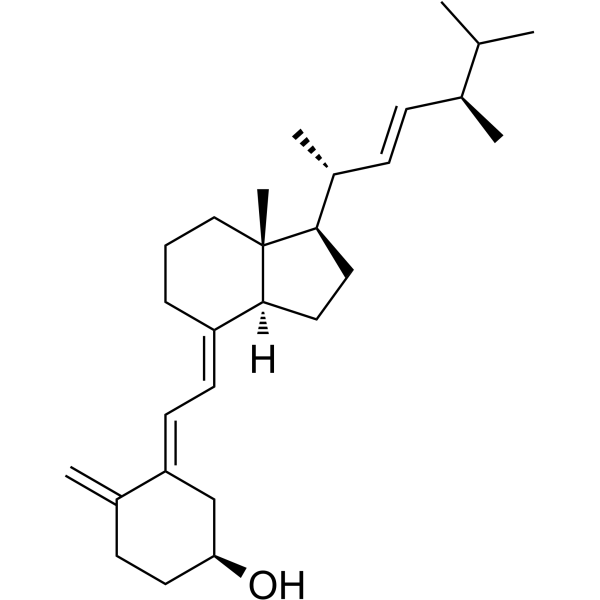
| 分子式 |
C28H44O
|
|---|---|
| 分子量 |
396.64836
|
| 精确质量 |
396.339
|
| CAS号 |
51744-66-2
|
| 相关CAS号 |
Vitamin D2;50-14-6
|
| PubChem CID |
6536972
|
| 外观&性状 |
Prisms from acetone
White crystals Colorless crystals |
| 熔点 |
239 to 244 °F (EPA, 1998)
116.5 °C |
| LogP |
7.641
|
| tPSA |
20.23
|
| 氢键供体(HBD)数目 |
1
|
| 氢键受体(HBA)数目 |
1
|
| 可旋转键数目(RBC) |
5
|
| 重原子数目 |
29
|
| 分子复杂度/Complexity |
678
|
| 定义原子立体中心数目 |
6
|
| SMILES |
[C@@H](C)(/C=C/[C@@H](C(C)C)C)[C@]1(CC[C@@]2([C@]1(C)CCC/C/2=C\C=C1\C(=C)CC[C@H](O)C\1)[H])[H]
|
| InChi Key |
MECHNRXZTMCUDQ-VLOQVYPSSA-N
|
| InChi Code |
InChI=1S/C28H44O/c1-19(2)20(3)9-10-22(5)26-15-16-27-23(8-7-17-28(26,27)6)12-13-24-18-25(29)14-11-21(24)4/h9-10,12-13,19-20,22,25-27,29H,4,7-8,11,14-18H2,1-3,5-6H3/b10-9+,23-12+,24-13+/t20-,22+,25-,26+,27-,28+/m0/s1
|
| 化学名 |
(1S,3E)-3-[(2E)-2-[(1R,3aS,7aR)-1-[(E,2R,5R)-5,6-dimethylhept-3-en-2-yl]-7a-methyl-2,3,3a,5,6,7-hexahydro-1H-inden-4-ylidene]ethylidene]-4-methylidenecyclohexan-1-ol
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: (1). 本产品在运输和储存过程中需避光。 (2). 请将本产品存放在密封且受保护的环境中(例如氮气保护),避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : ~25 mg/mL (~63.03 mM)
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (6.30 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: 2.5 mg/mL (6.30 mM) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 悬浊液; 超声助溶。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (6.30 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.5211 mL | 12.6056 mL | 25.2111 mL | |
| 5 mM | 0.5042 mL | 2.5211 mL | 5.0422 mL | |
| 10 mM | 0.2521 mL | 1.2606 mL | 2.5211 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。