| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| Other Sizes |
|
| 靶点 |
Wnt/β-catenin; c-Met (IC50 = 0.13 nM)
|
|---|---|
| 体外研究 (In Vitro) |
体外活性:INCB28060 表现出皮摩尔酶效,并且对 c-MET 具有高度特异性,其选择性比一大组人类激酶高 10,000 倍以上。 INCB28060 抑制癌细胞中的人 c-MET 磷酸化和 c-MET 介导的信号传导。 INCB28060 抑制 c-MET 依赖性细胞增殖和存活,并防止锚定非依赖性癌细胞生长和细胞迁移。激酶测定:测定缓冲液含有 50 mM Tris-HCl、10 mM MgCl2、100 mM NaCl、0.1 mg/ml BSA、5mM DTT,pH 7.8。对于 HTS,将溶解在 DMSO 中的 0.8 μL 5 mM INCB28060 点在 384 孔板上。 DMSO 滴定表明溶剂的最大耐受浓度为 4%。为了测量 IC50,INCB28060 板通过 3 倍和 11 点连续稀释来制备。将 0.8 μL INCB28060 的 DMSO 溶液从 INCB28060 板转移至测定板。 DMSO 的终浓度为 2%。在测定缓冲液中制备 8 nM 非磷酸化 c-Met 或 0.5 nM 磷酸化 c-Met 溶液。将溶解在 DMSO 中的肽底物生物素-EQEDEPEGDYFEWLE-酰胺的 1 mM 储备液在含有 400 μM ATP(未磷酸化 c-Met)或 160 uM ATP(磷酸化 c-Met)的测定缓冲液中稀释至 1 μM。将 20 μL 体积的酶溶液(或酶空白的测定缓冲液)添加到每个板的相应孔中,然后添加 20 μL/孔的底物溶液以启动反应。将板避光并在 25°C 下孵育 90 分钟。通过添加 20 μL 含有 45 mM EDTA、50 mM Tris-HCl、50 mM NaCl、0.4 mg/ml BSA、200 nM SA-APC 和 3 nM EUPy20 的溶液来终止反应。将板在室温下孵育 15-30 分钟,并在 Perkin Elmer Fusion α-FP 仪器上测量 HTRF(均质时间分辨荧光)。使用的 HTRF 程序设置如下:初级激励滤波器 330/30,初级窗口:200 uSec,初级延迟:50 uSec,闪烁次数:15,良好读取时间:2000。 细胞测定:H441 细胞接种在 RPMI- 1640培养基含有10% FBS并生长至完全融合。通过使用 P200 移液器吸头刮擦细胞来引入间隙。然后用 50 ng/mL 重组人 HGF 刺激细胞,以在存在不同浓度的 INCB28060 的情况下诱导细胞跨间隙迁移。过夜孵育后,拍摄代表性照片并进行细胞迁移抑制的半定性评估。
|
| 体内研究 (In Vivo) |
INCB28060在c-MET依赖的小鼠肿瘤模型中显示出很强的抗肿瘤活性[1]
为了评估INCB28060的体内活性,我们使用了S114细胞衍生的小鼠肿瘤模型。由于S114细胞同时表达人c-MET和HGF,因此这些细胞的肿瘤生长依赖于c-MET信号。为了确定控制c-MET磷酸化所需的INCB28060的最小剂量,我们对小鼠口服增加剂量的INCB28060,并在30分钟后测量肿瘤中的磷酸化c-MET水平。如图4A所示,0.03 mg/kg INCB28060是测试的最低剂量,可抑制约50%的c-MET磷酸化。剂量递增以剂量依赖的方式影响磷酸化c-MET,单次剂量为0.3mg/kg或更高可导致90%以上的抑制。为了进一步表征INCB28060随时间的影响,选择了3mg/kg的单次剂量。在7小时的测量时间点内,磷酸化c-MET的抑制率超过90%(图4B),这与同一时间段内磷酸化-c-MET的化合物暴露量超过蛋白质调整IC90(约71 nmol/L)是一致的(图4B)。因此,INCB28060的活性是剂量依赖性的,并且由于体内同一时间段的有效药物暴露水平而随时间持续。用MKN-45人癌症细胞衍生的小鼠肿瘤模型观察到类似的结果,该模型由c-MET激活驱动,作为c-MET扩增的结果(数据未显示)。 INCB28060在c-MET依赖性小鼠肿瘤模型中显示出很强的抗肿瘤活性,即使口服0.03 mg/kg INCB28060也会引起约50%的c-MET磷酸化抑制。在荷瘤小鼠中观察到肿瘤生长的剂量依赖性抑制。 |
| 酶活实验 |
测定缓冲液的成分如下:pH 7.8、50 mM Tris-HCl、10 mM MgCl2、100 mM NaCl、0.1 mg/ml BSA 和 5 mM DTT。在 HTS 的 384 孔板上点样的是溶解在 DMSO 中的 0.8 μL 5 mM INCB28060。根据DMSO滴定,4%的溶剂浓度是可以耐受的最高浓度。 INCB28060 板通过三个和十一个点的连续稀释来制备,以测量 IC50。从 INCB28060 板中转移 0.8 μL INCB28060 的 DMSO 溶液。 DMSO 的终浓度为 2%。在测定缓冲液中,制备 0.5 nM 磷酸化 c-Met 或 8 nM 非磷酸化 c-Met 溶液。在含有 400 μM ATP(未磷酸化 c-Met)或 160 uM ATP(磷酸化 c-Met)的测定缓冲液中,将溶解在 DMSO 中的肽底物生物素-EQEDEPEGDYFEWLE-酰胺的 1 mM 储备液稀释至 1 μM。要开始反应,向每个板的相应孔中添加 20 μL 体积的酶溶液(或酶空白的测定缓冲液)后,每孔添加 20 μL 底物溶液。将板在 25°C 避光条件下孵育 90 分钟。为了终止反应,引入 20 μL 包含 45 mM EDTA、50 mM Tris-HCl、50 mM NaCl、0.4 mg/ml BSA、200 nM SA-APC 和 3 nM EUPy20 的混合物。将板在室温下孵育 15-30 分钟后,Perkin Elmer Fusion α-FP 仪器测量均质时间分辨荧光 (HTRF)。使用以下 HTRF 程序设置:330/30 主激励滤波器,主窗口 200 uSec,主延迟 50 uSec,总共 15 次闪烁。读板时间:2000
|
| 细胞实验 |
在含有 10% FBS 的 RPMI-1640 培养基中,接种 H441 细胞并生长至完全汇合。使用 P200 移液器吸头刮擦细胞以形成间隙。接下来,在存在不同浓度的 INCB28060 的情况下,用 50 ng/mL 重组人 HGF 刺激细胞以诱导跨越间隙的迁移。经过过夜的孵育期后,对细胞迁移的抑制进行半定性评估并拍摄代表性照片。
细胞活力测定[1] 针对单个细胞系预先确定了存活率测定中使用的最佳细胞密度。为了测定化合物的效力,将细胞以适当的密度接种到96孔微孔板中,培养基中含有1%至2%的FBS,并补充了INCB28060的系列稀释液,最终体积为每孔100μL。孵育72小时后,向每个孔中加入24μL CellTiter 96 AQueous One溶液,并在37°C的孵化器中孵育2小时。使用微孔板读数器在490nm下在线性范围内测量光密度,在650nm下进行波长校正。使用GraphPad Prism软件计算IC50值。 软琼脂集落形成试验[1] 在不同浓度的50 ng/mL重组人HGF和INCB28060存在或不存在的情况下,在6孔板中以足够的密度制备U-87MG或H441细胞,该板与0.5 mL顶层琼脂混合,顶层琼脂在适当的培养基中含有0.3%琼脂糖,并补充有1%或10%FBS。将细胞均匀地放置在1mL在培养基中含有0.6%琼脂糖的固化基层琼脂上。将培养板在37°C的湿度为5%CO2的培养箱中培养。每周用含有适当浓度人HGF和INCB28060的顶层琼脂给细胞喂食一次。2至3周后拍摄代表性照片时,评估菌落的数量和大小。 细胞迁移试验[1] 将H441细胞接种在含有10%FBS的RPMI-1640培养基中,并生长至完全融合。通过用P200移液管尖端刮擦细胞来引入间隙。然后,在不同浓度的INCB28060存在下,用50 ng/mL重组人HGF刺激细胞,诱导其穿过间隙迁移。孵育过夜后,拍摄代表性照片,并对细胞迁移的抑制进行半定性评估。 细胞凋亡测定[1] 将细胞接种在96孔板中,在含有0.5%FBS的培养基中生长过夜。然后用不同浓度的INCB28060处理细胞24小时。根据制造商的说明,使用基于DNA片段的细胞死亡检测ELISAplus试剂盒测量细胞凋亡。为了测量PARP切割,细胞在10cm培养皿中生长,并如上所述用INCB28060进行类似处理。然后制备蛋白质提取物,并使用兔抗切割PARP(Asp214)抗体进行蛋白质印迹分析。 |
| 动物实验 |
Eight-week-old female Balb/c nu/nu mice (Charles River) are inoculated subcutaneously with 4 × 106 tumor cells (S114 model) or with 5 × 106 tumor cells (U-87MG glioblastoma model).
3, 10, 30 mg/kg INCB28060 is orally dosed, twice each day. Efficacy studies[1] Tumor-bearing mice were dosed orally, twice each day with 1, 3, 10, or 30 mg/kg of free base INCB28060 reconstituted in 5% DMAC in 0.5% methylcellulose for up to 2 weeks. Body weights were monitored throughout the study as a gross measure of toxicity/morbidity. Tumor growth inhibition, expressed in percent, was calculated using the formula: (1 − [(volume (treated)/volume (vehicle)]) × 100. Pharmacodynamic analysis[1] For pharmacodynamic analysis, S114 tumor–bearing mice were monitored for tumor growth and then randomized into groups of 3 with average tumor sizes of approximately 300 to 500 mm3. For time course studies, mice were given a single oral dose of 3 mg/kg INCB28060 reconstituted in 5% DMAC in 0.5% methylcellulose and tumors were harvested at the indicated time points. For dose escalation studies, mice were given a single oral dose of INCB28060 at 0.03, 0.1, 0.3, 1, 3, or 10 mg/kg reconstituted in 5% DMAC in 0.5% methylcellulose and tumors were harvested 30 minutes after dosing. All tumors were processed for the determination of phospho-c-Met levels using the Human Phospho-HGFR/c-Met kit. The plasma concentration of INCB28060 was determined by LC/MS/MS analysis following retro-orbital or cardiac puncture blood collection. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
The oral bioavailability of capmatinib is estimated to be >70%. Following oral administration, maximum plasma concentrations are achieved within 1 to 2 hours (Tmax). Co-administration with a high-fat meal increased capmatinib AUC by 46% with no change in Cmax (as compared to fasted conditions), and co-administration with a low-fat meal had no clinically meaningful effects on exposure. Following oral administration of radiolabeled capmatinib, approximately 78% of the radioactivity is recovered in feces, of which ~42% is unchanged parent drug, and 22% is recovered in the urine, of which a negligible amount remains unchanged parent drug. The apparent volume of distribution at steady-state is 164 L. The mean apparent clearance of capmatinib at steady-state is 24 L/h. Metabolism / Metabolites Capmatinib undergoes metabolism primarily via CYP3A4 and aldehyde oxidase. Specific biotransformation pathways and metabolic products have yet to be elucidated. Biological Half-Life The elimination half-life is 6.5 hours. |
| 毒性/毒理 (Toxicokinetics/TK) |
Hepatotoxicity
In the prelicensure clinical trials of capmatinib in patients with solid tumors harboring MET mutations, liver test abnormalities were frequent although usually self-limited and mild. Some degree of ALT elevations arose in 39% of capmatinib treated patients and were above 5 times the upper limit of normal (ULN) in 7%. In these trials that enrolled 373 patients, capmatinib was discontinued early due to increased AST or ALT in only 1% of patients. The liver test abnormalities had a median onset of 2 months after initiation of therapy. While serum aminotransferase elevations were occasionally quite high (5 to 20 times upper limit of normal), there were no accompanying elevations in serum bilirubin and no patient developed clinically apparent liver injury with jaundice. The product label for capmatinib recommends monitoring for routine liver tests before, at 2 week intervals during the first 3 months of therapy, and monthly thereafter as clinically indicated. Likelihood score: E* (unproven but suspected rare cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation No information is available on the clinical use of capmatinib during breastfeeding. Because capmatinib is 96% bound to plasma proteins, the amount in milk is likely to be low. The manufacturer recommends that breastfeeding be discontinued during capmatinib therapy and for 1 week after the last dose. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding Plasma protein binding is approximately 96% and is independent of drug serum concentration. |
| 参考文献 | |
| 其他信息 |
Pharmacodynamics
Capmatinib inhibits the overactivity of c-Met, a receptor tyrosine kinase encoded by the _MET_ proto-oncogene. Mutations in _MET_ are involved in the proliferation of many cancers, including non-small cell lung cancer (NSCLC). Capmatinib may cause photosensitivity reactions in patients following ultraviolet (UV) exposure - patients undergoing therapy with capmatinib should be advised to use sunscreen and protective clothing to limit exposure to UV radiation. Instances of interstitial lung disease/pneumonitis, which can be fatal, occurred in patients being treated with capmatinib. Patients presenting with signs or symptoms of lung disease (e.g. cough, dyspnea, fever) should have capmatinib immediately withheld, and capmatinib should be permanently discontinued if no other feasible causes of the lung-related symptoms are identified. |
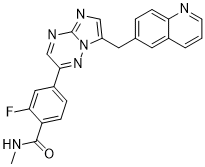
| 分子式 |
C23H17FN6O
|
|
|---|---|---|
| 分子量 |
412.42
|
|
| 精确质量 |
412.144
|
|
| 元素分析 |
C, 66.98; H, 4.15; F, 4.61; N, 20.38; O, 3.88
|
|
| CAS号 |
1029712-80-8
|
|
| 相关CAS号 |
Capmatinib dihydrochloride hydrate;1865733-40-9;Capmatinib dihydrochloride;1197376-85-4;Capmatinib hydrochloride;1029714-89-3
|
|
| PubChem CID |
25145656
|
|
| 外观&性状 |
Yellow solid powder
|
|
| 密度 |
1.4±0.1 g/cm3
|
|
| 折射率 |
1.717
|
|
| LogP |
-0.12
|
|
| tPSA |
88.56
|
|
| 氢键供体(HBD)数目 |
1
|
|
| 氢键受体(HBA)数目 |
6
|
|
| 可旋转键数目(RBC) |
4
|
|
| 重原子数目 |
31
|
|
| 分子复杂度/Complexity |
637
|
|
| 定义原子立体中心数目 |
0
|
|
| SMILES |
FC1=C(C(N([H])C([H])([H])[H])=O)C([H])=C([H])C(=C1[H])C1C([H])=NC2=NC([H])=C(C([H])([H])C3C([H])=C([H])C4=C(C([H])=C([H])C([H])=N4)C=3[H])N2N=1
|
|
| InChi Key |
LIOLIMKSCNQPLV-UHFFFAOYSA-N
|
|
| InChi Code |
InChI=1S/C23H17FN6O/c1-25-22(31)18-6-5-16(11-19(18)24)21-13-28-23-27-12-17(30(23)29-21)10-14-4-7-20-15(9-14)3-2-8-26-20/h2-9,11-13H,10H2,1H3,(H,25,31)
|
|
| 化学名 |
2-fluoro-N-methyl-4-[7-(quinolin-6-ylmethyl)imidazo[1,2-b][1,2,4]triazin-2-yl]benzamide
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.08 mg/mL (5.04 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 20.8 mg/mL澄清DMSO储备液加入400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.08 mg/mL (5.04 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 20.8 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: 5%DMSO+40%PEG300+5%Tween80+50%ddH2O: 6mg/ml 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.4247 mL | 12.1236 mL | 24.2471 mL | |
| 5 mM | 0.4849 mL | 2.4247 mL | 4.8494 mL | |
| 10 mM | 0.2425 mL | 1.2124 mL | 2.4247 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
A Study of Amivantamab and Capmatinib Combination Therapy in Unresectable Metastatic Non-small Cell Lung Cancer
CTID: NCT05488314
Phase: Phase 1/Phase 2 Status: Active, not recruiting
Date: 2024-10-24
INCB28060 inhibits c-MET–dependent cell proliferation and survival. Clin Cancer Res. 2011 Nov 15;17(22):7127-38. |
HGF induces production of TGF-α, AR, and HRG-β1 in cancer cells and INCB28060 effectively blocks the induction. |
Cross-talk between c-MET and EGFR or HER-3 in cancer cells. |