| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| Other Sizes |
|
| 靶点 |
ACAT1 (IC50 = 24 μM); ACAT2 (IC50 = 9.2 μM)
|
|---|---|
| 体外研究 (In Vitro) |
当给予阿伐麦布(0、0.25、5、10、20、40和80μM;1、2和3天)时,前列腺癌(PCa)细胞增殖较少[2]。 β-连环蛋白、波形蛋白、N-钙粘蛋白、Snail 和 MMP9 的表达(所有这些都与上皮间质转化 (EMT) 密切相关)被Avasimibe(10 和 20 μM;48 小时)降低 [2] 。在前列腺癌中,avasimibe(10 和 20 μM)通过 E2F-1 信号通路诱导细胞周期停滞。在 PCa 细胞中,avasimibe 导致 G1 期细胞周期停滞 [2]。阿伐麦布(10 和 20 μM)可抑制 PCa 细胞转移 [2]。
|
| 体内研究 (In Vivo) |
在七周内,avasimibe(每隔一天腹腔注射 30 mg/kg)可抑制体内 PCa 细胞的发育和转移。Avasimibe毒性极小,具有良好的生物相容性[2]。
Avasimibe体内抑制前列腺癌细胞生长和转移[2] 通过皮下移植PC-3细胞建立异种移植模型,我们的研究发现,与对照组相比,avasimibe使肿瘤体积减小(图4a, b)。异种移植肿瘤的H&E染色和Ki67免疫荧光染色进一步证实了avasimibe对PCa细胞生长的抑制作用(图4c)。免疫荧光染色也观察到avasimibe组E2F-1表达上调(图4c)。[2] 研究人员通过尾静脉注射表达gfp的PC-3 LV-NC细胞建立肺转移模型,评估表达gfp的PC-3 LV-NC细胞的荧光强度,评价其迁移能力。avasimibe组肺转移瘤的荧光强度弱于对照组(图4d, e)。肺组织H&E染色显示,avasimibe治疗可抑制肺转移瘤的数量(图4f)。[2] |
| 细胞实验 |
细胞活力测定[2]
细胞类型: PCa 细胞(PC-3 和 DU 145) 测试浓度: 0、0.25、5、10、 20、40 和 80 µM 孵育时间:1、2 和 3 天 实验结果:剂量依赖性抑制 PC-3 和 DU 145 细胞活力。 蛋白质印迹分析[2] 细胞类型: PCa 细胞(PC-3 和 DU 145) 测试浓度: 10 和20 µM 孵育持续时间: 48 小时 实验结果:降低 EMT 相关蛋白(β-连环蛋白、波形蛋白、N-钙粘蛋白、Snail、MMP9 和 E-钙粘蛋白)。 细胞周期分析[2] 细胞类型: PCa 细胞(PC-3 和 DU 145) 测试浓度: 10 和20 µM 孵育时间: 48 小时 实验结果:诱导 G1 期周期停滞并改变 PCa 细胞中 G1 期相关蛋白水平。 MTT试验[1] 简单地说,将PCa细胞在96孔板中(3000个细胞/孔;200µl培养基)处理1天,并用avasimibe(0、0.25、5、10、20、40和80µM)处理1、2和3天。细胞与20µl MTT (5 mg/ml/孔)在37℃下孵育4小时。丢弃上清后,将MTT甲醛晶体溶解于200µl/孔DMSO中,用微孔板仪测定490 nm处OD值。 克隆生存试验[1] 将PCa细胞置于六孔板上(每孔1500个细胞)。1天后,将正常培养基替换为avasimibe工作液。细胞培养10到15天,直到它们长成菌落。丢弃培养基,用4%多聚甲醛(PFA)固定细胞1 h, 0.1%结晶紫染色半小时。使用Image-Pro Plus计算菌落。 创面愈合试验[1] Avasimibe处理的PCa细胞在六孔板中生长,直到细胞达到95%的合流。然后,用1毫升无菌蓝色微管尖端刮擦细胞单层。将细胞用PBS洗涤2次后,在添加2% FBS和不同浓度avasimibe的培养基中培养12 h。然后在0和12 h用倒置荧光显微镜在预先标记的白光下拍摄细胞。用Photoshop测量划痕边缘之间的水平距离。迁移速率= 1−(12 h划痕距离/0 h初始距离)。 跨井迁移试验[1] 通过Transwell室系统评估细胞迁移。在六孔板上用avasimibe预处理细胞48 h,然后在200µl培养基(无血清)中加入avasimibe处理的PCa细胞(1.2 × 105 PC3或8 × 104 DU 145细胞),在下孔室中放置600µl正常培养基。孵育1天后,用4% PFA固定半小时,0.1%结晶紫染色1小时。在5个随机场倒置相差显微镜下拍照和评价。 流式细胞术用于细胞周期分析[1] 转染1 d后,细胞用avasimibe工作液处理1 d。收集经阿瓦西米处理的PCa细胞,用PBS洗涤三次。共收获1× 106个细胞进行细胞周期染色,然后取1× DNA染色液500µl和通透化液5µl置于黑暗中试管中染色30 min。按照前面的方法对样品的1× 104个细胞进行流式细胞术评估。使用FlowJo软件分析数据。 流式细胞术检测细胞凋亡[1] 细胞凋亡实验步骤如前所述。用100µl结合缓冲液(1×)重悬PCa细胞,用FITC-annexin V(5µl)和碘化丙啶(PI, 5µl)在25°C黑暗条件下染色10 min。然后加入1×结合缓冲液,使其总体积达到500µl,用流式细胞术对样品进行评价。细胞凋亡百分比=晚期细胞凋亡百分比+早期细胞凋亡百分比。 流式细胞术检测活性氧(ROS) [1] 流式细胞术检测细胞内ROS水平。Avasimibe处理的PCa细胞用2 ',7 ' -二氯二氢荧光素二乙酸酯(DCFH-DA,10µM)在25℃下染色20 min,避光,然后用PBS洗涤。流式细胞术检测ROS水平。 |
| 动物实验 |
Animal/Disease Models: SPF male mice (BALB/c-nude, 4 weeks old) bearing PCa cells[2]
Doses: 30 mg/kg Route of Administration: Intraperitoneally injected for 7 weeks Experimental Results: decreased tumor volume compared with that of the control group. Inhibited PCa growth and migration in vivo. Xenograft model and pulmonary metastasis model [2] SPF male mice (BALB/c-nude, 4 weeks old) were acclimated to the environment of the animal facility for seven days.[2] Tumour-bearing mice were constructed by inoculating 2 × 106 PC-3 cells into the flanks of mice (n = 7). Seven days later, avasimibe(30 mg/kg, dissolved in DMSO and diluted in PBS containing 1% Tween-80) and solvent were intraperitoneally injected on alternate days for 7 weeks (the stock solution had a concentration of 25 mg/ml). The mice were anaesthetized by intraperitoneal injection of pentobarbital (50 mg/kg) before euthanasia. Tumour volume was measured with a Vernier scale every other day for 7 weeks, and tumour volume was calculated as follows: tumour volume (mm3) = tumour length × width2/2. We separated the tumour tissues, and then, the tumour tissues were fixed in 4 % PFA and verified by H&E and immunofluorescence staining.[2] Pulmonary metastasis models were constructed by injecting 2 × 106 PC-3 (LV-NC GFP-expressing) cells into the tail vein of mice (n = 5). Avasimibe (30 mg/kg) and solvent were administered as described above for 7 weeks. The fluorescence intensity of lung metastasis tumours was measured using a Fusion FX7 Spectra Imaging system. Then, the lungs were surgically exposed and collected for further analysis by H&E. Avasimibe was administered orally as bulk drug in gelatin capsules on a mg/kg body weight basis. Control animals received empty gelatin capsules equal in number to those given to the high-dose group for each study. The 2-week repeated-dose study was the first study conducted with avasimibe in dogs (see below). The doses were selected based on experience with a previous ACAT inhibitor (Wolfgang et al., 1995). However, the study failed to define a dose-limiting toxicity. Therefore, an escalating dose study was conducted in order to establish a maximum tolerated dose. In the study, 2 male dogs were administered 100 mg/kg on Days 1–9, 1000 mg/kg once a day on Days 10–16 and 1000 mg/kg b.i.d. on Days 17–23. The b.i.d. doses were administered 8 h apart. Plasma drug concentrations were determined pre-dose, 1.5, 4, 8, 12, and 24 h post-dose on Days 9 and 16, and pre-dose, 1.5, 4, 8, 9.5, 12, 16, 24, and 32 h post-dose (first dose) on Day 23. Hematological and serum chemistry parameters were measured pre-test and on Days 8, 15, and 22. The animals were not euthanized at the end of the study. Reference: Toxicol Sci. 2001 Feb;59(2):324-34. |
| 毒性/毒理 (Toxicokinetics/TK) |
Avasimibe, a novel inhibitor of acyl coenzyme A:cholesterol acyltransferase (ACAT), is currently being developed as an antiatherosclerotic agent. The preclinical safety and toxicokinetics of the compound were assessed in beagle dogs in an escalating-dose study and in repeated-dose studies of 2-, 13-, and 52-week duration. Oral (capsule) doses up to 1000 mg/kg b.i.d. were assessed in the escalating dose study and once-a-day doses up to 300 mg/kg, 1000 mg/kg, and 1000 mg/kg were assessed in the 2-, 13-, and 52-week studies, respectively. Avasimibe was found to be a substrate and inducer of hepatic CYP 3A, producing pronounced decreases in plasma drug concentrations subsequent to Day 1. Plasma drug concentrations plateaued markedly at doses above 100 mg/kg. Significant toxicologic findings were restricted to the higher doses (> or =300 mg/kg) and included emesis, fecal consistency changes, salivation, body weight loss, microscopic and clinical pathologic evidence of hepatic toxicity, and red blood cell (RBC) morphology changes. Mortality occurred at 1000 mg/kg due to hepatic toxicity. Toxicity was more closely associated with the exaggerated pharmacodynamic effects of the compound (e.g., marked serum cholesterol decreases) seen at the high doses of avasimibe used in these studies rather than with measures of systemic exposure (Cmax or AUC). Adrenal effects were noted only in the 52-week study and consisted of minimal to mild cortical cytoplasmic vacuolization and fibrosis at doses > or =300 mg/kg, with no change in adrenal weight. In conclusion, avasimibe is an ACAT inhibitor that has minimal adrenal effects in dogs, with dose-limiting toxicity defined by readily monitored and reversible changes in hepatic function. Toxicol Sci. 2001 Feb;59(2):324-34.
|
| 参考文献 |
[1]. Taichi Ohshiro,et al. Pyripyropene A, an acyl-coenzyme A:cholesterol acyltransferase 2-selective inhibitor, attenuates hypercholesterolemia and atherosclerosis in murine models of hyperlipidemia. Arterioscler Thromb Vasc Biol. 2011 May;31(5):1108-15.
[2]. Kangping Xiong, et al. The cholesterol esterification inhibitor avasimibe suppresses tumour proliferation and metastasis via the E2F-1 signalling pathway in prostate cancer.Cancer Cell Int. 2021 Aug 30;21(1):461. |
| 其他信息 |
Avasimibe is a monoterpenoid.
Avasimibe is an orally bioavailable inhibitor of acyl-Coenzyme A:cholesterol acyltransferase (ACAT) that prevents cholesterol deposition in the arterial wall. Research was discontinued due to difficulties in assaying the effects of avasimibe on preventing plaque formation and due to its ability to increase the activity of Cytochrome P450 3A4, thus increasing the removal of other drugs from the body. Drug Indication Investigated for use/treatment in peripheral vascular disease. Background: New effective drugs for prostate cancer (PCa) treatment are urgently needed. Avasimibe was recently identified as a promising drug for anticancer therapies. The main purpose of this study was to explore the effects and the underlying mechanisms of avasimibe in prostate cancer. Methods: In this study, MTT and clonogenic survival assays were performed to detect cell proliferation after avasimibe treatment. The effect of avasimibe on cell migration was measured by wound healing and transwell migration assays. Cell cycle distribution and apoptosis were detected by flow cytometry. Immunofluorescence staining and western blot analysis were used to detect the expression of cell cycle-related proteins and epithelial-mesenchymal transition (EMT)-related proteins. In vivo, the antitumour effects of avasimibe were evaluated using a xenograft model and pulmonary metastasis model. Results: The study found that avasimibe suppresses tumour growth and triggers G1 phase arrest. Moreover, the expression of the cell cycle-related proteins CDK2/4/6, Cyclin D1 and Cyclin A1 + A2 was significantly increased and p21 expression was decreased after avasimibe treatment. The migration of PCa cells was attenuated after treatment with avasimibe, followed by the downregulation of the expression of the EMT-related proteins N-cadherin, β-catenin, vimentin, Snail and MMP9 and upregulation of E-cadherin expression. Moreover, E2F-1 was elevated after treatment with avasimibe. After knockdown of E2F-1 expression, the inhibition of cell proliferation and migration caused by avasimibe was significantly recovered. The results of the xenograft model showed that avasimibe suppressed tumour growth in vivo. Immunofluorescence staining revealed lower levels of Ki67 and higher levels of E2F-1 in tumour tissues of the avasimibe group than those of the control group. A pulmonary metastasis model also confirmed the inhibition of PCa metastasis by avasimibe. The number of lung metastatic foci in the avasimibe group was significantly decreased compared with that in the control group. Conclusions: Our results suggest that avasimibe can suppress tumour proliferation and metastasis via the E2F-1 signalling pathway. These findings demonstrate the potential of avasimibe as a new effective drug for PCa treatment.[2] Avasimibe is a novel orally bioavailable ACAT inhibitor , currently under clinical development (phase III trials). It was safe when administered to rats, dogs, and humans. In vitro studies in human macrophages demonstrated that avasimibe reduces foam cell formation not only by enhancing free cholesterol efflux, but also by inhibiting the uptake of modified LDL. The concentration-dependent reduction in cellular cholesteryl ester content in these cells was not accompanied by an increase in intracellular free cholesterol, which is in agreement with a good safety profile for avasimibe. In the liver, avasimibe caused a significant reduction in the secretion of apo B and apo B-containing lipoproteins into plasma. Avasimibe induced cholesterol 7alpha-hydroxylase and increased bile acid synthesis in cultured rat hepatocytes, and its administration to rats did not produce an increase in lithogenicity index of the bile. The hypolipidemic efficacy of the compound was demonstrated in cholesterol-fed as well as in non-cholesterol-fed animals. In these models, plasma cholesterol levels were reduced, mainly due to the decrease in the non-HDL cholesterol fraction. Clinical data are scarce, but in a study performed in 130 men and women with combined hyperlipidemia and hypoalphalipoproteinemia, avasimibe, 50-500 mg/day, significantly reduced plasma total triglyceride and VLDL-cholesterol. Although total cholesterol, LDL-cholesterol, and HDL-cholesterol were unchanged, it must be stressed that animal data suggest that avasimibe may have direct antiatherosclerotic activity in addition to its cholesterol-lowering effect. Avasimibe treatment can also contribute to increase plaque stability, as it reduces the accumulation of lipids in the arterial wall, inhibits macrophage infiltration into the media and reduces matrix metalloproteinase expression and activity. Moreover, avasimibe and statins have been shown to have synergistic effects, and the combination therapy may not only inhibit atherosclerotic lesion progression but also induce lesion regression, independently of changes in plasma cholesterol.Reference: Cardiovasc Drug Rev. 2003 Spring;21(1):33-50. |
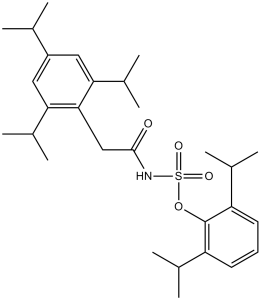
| 分子式 |
C29H43NO4S
|
|
|---|---|---|
| 分子量 |
501.72
|
|
| 精确质量 |
501.291
|
|
| 元素分析 |
C, 69.42; H, 8.64; N, 2.79; O, 12.76; S, 6.39
|
|
| CAS号 |
166518-60-1
|
|
| 相关CAS号 |
166518-61-2 (sodium); 166518-60-1 (free form);
|
|
| PubChem CID |
166558
|
|
| 外观&性状 |
Typically exists as white to off-white solids at room temperature
|
|
| 密度 |
1.1±0.1 g/cm3
|
|
| 熔点 |
178-180° (Lee); mp 169.5-170.4° (Dozeman)
|
|
| 折射率 |
1.529
|
|
| LogP |
9.34
|
|
| tPSA |
80.85
|
|
| 氢键供体(HBD)数目 |
1
|
|
| 氢键受体(HBA)数目 |
4
|
|
| 可旋转键数目(RBC) |
10
|
|
| 重原子数目 |
35
|
|
| 分子复杂度/Complexity |
734
|
|
| 定义原子立体中心数目 |
0
|
|
| SMILES |
S(N([H])C(C([H])([H])C1C(=C([H])C(C([H])(C([H])([H])[H])C([H])([H])[H])=C([H])C=1C([H])(C([H])([H])[H])C([H])([H])[H])C([H])(C([H])([H])[H])C([H])([H])[H])=O)(=O)(=O)OC1C(=C([H])C([H])=C([H])C=1C([H])(C([H])([H])[H])C([H])([H])[H])C([H])(C([H])([H])[H])C([H])([H])[H]
|
|
| InChi Key |
PTQXTEKSNBVPQJ-UHFFFAOYSA-N
|
|
| InChi Code |
InChI=1S/C29H43NO4S/c1-17(2)22-14-25(20(7)8)27(26(15-22)21(9)10)16-28(31)30-35(32,33)34-29-23(18(3)4)12-11-13-24(29)19(5)6/h11-15,17-21H,16H2,1-10H3,(H,30,31)
|
|
| 化学名 |
((2,4,6-Tris(1-methylethyl)phenyl)acetyl)sulfamic acid 2,6-bis(1-methylethyl)phenyl ester
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: 7.5 mg/mL (14.95 mM) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 悬浮液;超声助溶。
例如,若需制备1 mL的工作液,可将100 μL 75.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: 7.5 mg/mL (14.95 mM) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 悬浊液; 超声助溶。 例如,若需制备1 mL的工作液,可将 100 μL 75.0mg/mL澄清的DMSO储备液加入到900μL 20%SBE-β-CD生理盐水中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: 7.5 mg/mL (14.95 mM) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶. 配方 4 中的溶解度: 2% DMSO+corn oil: 5mg/mL 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.9931 mL | 9.9657 mL | 19.9314 mL | |
| 5 mM | 0.3986 mL | 1.9931 mL | 3.9863 mL | |
| 10 mM | 0.1993 mL | 0.9966 mL | 1.9931 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
|
|---|
|
|