| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| Other Sizes |
| 靶点 |
Natural triterpenoid saponinl; HMGB1; anti-tumor; anti-diabetic
|
|---|---|
| 体外研究 (In Vitro) |
甘草酸二钾(0-400 μM,4 天)可抑制 IL-4 和 IL-13 产生的细胞中特应性皮炎相关基因(NELL2、CA2、AQP3 和 HAS3 基因水平)的 mRNA 水平 [1]。甘草酸二钾(0-400 μM,4 天)可部分恢复 IL-4/IL-13 诱导的 AD 样皮肤等效小鼠的特应性皮炎样表型(海绵状细胞间隙)[1]。 0-100 μM,24 小时)可减少舒尼替尼诱导的 CCC-HEH-2 细胞自噬和细胞死亡 [5]。
特应性皮炎(AD)是一种慢性炎症性皮肤病,目前尚未完全了解。皮肤屏障功能缺陷和Th2免疫反应失调被认为是AD发病的关键。在本研究中,我们使用角质形成细胞和使用Th2细胞因子IL-4和IL-13的ad样皮肤等效模型。采用角化细胞和AD样皮肤模型研究甘草酸二钾/dipotassium glycyrrhizinate (KG)对AD治疗的影响。KG在受Th2细胞因子刺激的角质形成细胞中降低ad相关基因表达。在ad样皮肤等效模型中,KG减轻ad样表型和基因表达模式,并抑制ad相关细胞因子的释放。这些发现表明KG在AD治疗中具有潜在的有效性,AD样皮肤等效模型可能有助于了解AD的发病机制 甘草酸(GA)/dipotassium glycyrrhizinate (KG)对转染TGR5[2]细胞中TGR5的直接影响 [2] 在我们之前的报道中,我们使用CHO-K1细胞转染外源性TGR5受体基因。然后应用Western blot分析证实实验成功。这些CHO-K1细胞中表达的TGR5具有功能性。[2] 然后,应用这些细胞来估计GA对TGR5受体的直接影响。在表达TGR5的细胞中,GA处理显著增强了以细胞内2-NBDG含量为指标的葡萄糖摄取(图3A)。Triamterene剂量依赖性地阻断了这些细胞中ga诱导的葡萄糖摄取(图3B)。此外,GA在TGR5-CHO-K1细胞中也以剂量依赖性的方式增加了环AMP (cAMP)水平(图3C),并以同样的方式降低了三萜烯(图3D)。然而,在2-NBDG摄取增加(图3A)或cAMP水平升高(图3B)方面,GA并未影响缺乏TGR5表达的CHO-K1细胞。 甘草酸(GA)/dipotassium glycyrrhizinate (KG)通过TGR5促进肠细胞[2]中GLP-1的分泌 [2] 具有TGR5受体的培养肠道NCI-H716细胞常被用于研究GLP-1的释放。在与GA孵育的NCI-H716细胞中也观察到GLP-1分泌明显升高(图4A)或钙内流(图4B)。然而,在沉默NCI-H716细胞中表达的TGR5基因后,GA的这两种作用都被删除了。这与我们之前的报道完全相似,丁烯酸通过激活TGR5促进GLP-1的释放。 |
| 体内研究 (In Vivo) |
甘草酸二钾(150 mg/kg,腹腔注射)可提高心血管 GLP-1 水平并减轻链脲佐菌素(65 mg/kg,腹腔注射)引起的 1 型糖尿病症状 [2]。 (50 mg/kg,腹腔注射,每天一次,持续 4 周)可预防大鼠碘化钾引起的自身免疫炎症模型中前列腺炎的发生[3]。腹腔注射50–200 mg/kg甘草酸二钾。
甘草酸升高链脲佐菌素诱导的 1 型糖尿病大鼠(STZ 治疗的大鼠)血浆 GLP-1 水平,而氨苯蝶啶足以抑制武田 G 蛋白偶联受体 5 (TGR5) 被阻断 [1]。在小鼠中,甘草酸(50 mg/kg,腹腔注射)可显着降低 TgAb、HMGB1、TNF-α、IL-6 和 IL-1β 水平 [3]。
甘草酸对1型糖尿病大鼠血糖变化的影响 [2] 在STZ诱导的糖尿病大鼠中,注射甘草酸(GA)以剂量依赖的方式减轻了高血糖(图1A)。此外,与正常大鼠(141.4±10.2 pmol/l,n=8)相比,STZ诱导的糖尿病大鼠的血浆胰岛素水平(5.35±2.11 pmol/l,n=8)显著降低。然而,最高剂量的GA未能改变这些糖尿病大鼠的血浆胰岛素水平(5.66±1.39 pmol/l,n=8)。这意味着内源性胰岛素在该动物模型中不参与GA的作用。西格列汀以有效抑制二肽基肽酶-4(DPP-4)的剂量也减轻了这些糖尿病大鼠的高血糖。西格列汀显著增强了糖尿病大鼠注射GA后高血糖的降低(图1A)。此外,无论西格列汀预处理如何,氨苯蝶啶都能剂量依赖性地抑制这些糖尿病大鼠中GA诱导的变化(图1B)。 甘草酸(GA)对糖尿病大鼠血浆GLP-1水平变化的影响 [2] 在1型糖尿病大鼠中,甘草酸(GA)诱导血浆GLP-1水平呈剂量依赖性升高(图2A)。通过以有效抑制GLP-1失活酶DPP-4的剂量用西格列汀预处理,糖尿病大鼠中甘草酸(GA)的这种作用显著增强(图2A)。此外,与血糖的变化类似,在这些糖尿病大鼠中,无论是否用西格列汀预处理,氨苯蝶啶也以剂量依赖性方式逆转了GA诱导的血浆GLP-1水平的升高(图2B)。 NaI组在8周和16周时HMGB1的mRNA表达明显高于对照组。NaI组甲状腺球蛋白抗体、HMGB1、肿瘤坏死因子α、IL-6和IL-1β的血清水平显著升高,但甘草酸(GL)注射液显著降低了这些水平。NaI+甘草酸(GL)组的甲状腺炎患病率和淋巴细胞浸润率显著降低甘草酸(GL)给药也显著降低了甲状腺中TLR2、MyD88、HMGB1和核转录因子κB的蛋白表达,减轻了甲状腺炎的严重程度。[3] 结论:HMGB1可能通过引起炎症浸润在自身免疫性甲状腺炎中起关键作用,从而增加自身免疫性甲状腺疾病的严重程度甘草酸(GL)有效地减轻了碘诱导的NOD中的甲状腺炎。H-2h4小鼠通过与抑制TLR2-HMGB1信号传导相关的分子机制[3]。 特发性肺纤维化是一种进行性和致死性肺间质性疾病,目前缺乏有效的治疗方法。甘草酸/Glycyrrhizic acid (GA)是一种从传统中草药甘草中提取的天然化合物,最近有报道称其在动物模型中对肺损伤和肝纤维化有改善作用,但GA是否对肺纤维化有治疗作用尚不清楚。在这项研究中,我们研究了GA对博来霉素(BLM)诱导的肺纤维化大鼠模型肺纤维化的潜在治疗作用。结果表明,GA治疗显著改善了blm诱导的肺纤维化,减轻了blm诱导的炎症、氧化应激、上皮-间质转化和肺部转化生长因子- β信号通路的激活。此外,我们在体外证明了GA处理抑制3T6成纤维细胞的增殖,诱导细胞周期阻滞并促进细胞凋亡,这意味着GA介导的纤维增殖抑制可能有助于抗blm诱导的肺纤维化。总之,我们的研究表明GA在治疗肺纤维化方面具有治疗潜力[6].。 |
| 酶活实验 |
抗菌试验[4]
通过生长抑制效率和最小抑菌浓度(MIC)来评估GL凝胶的抗菌活性。金黄色葡萄球菌(S.aureus)和大肠杆菌(E.coli)分别被用作代表性的革兰氏阳性菌和革兰氏阴性菌。简而言之,将单个菌落接种到5 mL Luria Bertani(LB)肉汤培养基中,在37℃下以200 rpm的速度振荡培养过夜。过夜预培养后,将细菌悬浮液在LB培养基中稀释至106cfu mL-1,然后补充终浓度为0至2 mM的PBS或GL凝胶。然后将培养物在37℃下轻轻摇晃过夜。使用Synergy H1酶标仪在600nm波长下测量培养物的光密度。当没有观察到可见的细菌生长时,MIC被确定为抗菌材料的最低浓度。1遵循相同的程序实时监测用不同浓度的PBS或GL凝胶处理的细菌的生长动力学,除了在培养过程中的不同时间点记录每种培养物的OD600。特别是,将106cfu mL-1的金黄色葡萄球菌和大肠杆菌分别与终浓度为MIC的PBS或GL凝胶一起孵育。孵育2小时后,用PBS将细菌悬浮液稀释100倍,将100μL稀释的细菌铺在琼脂培养板上,在37℃下孵育过夜。 活/死荧光染色[4] 在MIC下用PBS或GL凝胶处理2小时后,通过离心收获金黄色葡萄球菌和大肠杆菌,并用0.9%NaCl洗涤3次。然后在黑暗中用SYTO 9和来自活/死染色试剂盒(L7012)的碘化丙啶(PI)对细菌进行染色30分钟。然后用LSM 700共聚焦激光扫描显微镜成像系统对细菌进行可视化。 细菌的形态学特征[4] SEM用于研究GL凝胶处理后细菌的形态。将106cfu mL-1的金黄色葡萄球菌和大肠杆菌与终浓度为MIC的PBS或GL凝胶一起孵育2小时,通过离心收集并用2.5%(w/w)戊二醛固定2小时。用PBS洗涤3次后,将细菌滴在硅片上并干燥过夜。硅片表面的细菌依次用分级乙醇水溶液(30%、50%、70%、80%、90%和100%)脱水10分钟。干燥过夜后,用金涂覆样品,并使用Phenom World Pro X扫描电子显微镜成像。 |
| 细胞实验 |
细胞活力测定[4]
对L929成纤维细胞进行细胞活力测定,以确定GL凝胶的体外细胞毒性。简而言之,L929细胞在添加了10%胎牛血清(FBS)的Dulbecco's Modified Eagle's Medium(DMEM)中在37℃、5%CO2的气氛中生长◦C.收获细胞,以每孔1×104个细胞的接种密度接种在96孔板中。孵育过夜后,将DMEM培养基替换为含有一定浓度的制备好的GL凝胶的新鲜培养基。孵育24小时后,用含有10%CellTiter BlueTM试剂的100μL培养基代替培养基,在37℃下孵育2小时◦C.使用Synergy H1酶标仪在550/590nm(Ex/Em)下测量荧光强度。通过与阴性对照(用PBS处理的L929细胞)进行比较来计算相对细胞存活率。 细胞成像[4] L929细胞接种在24孔板中,接种密度为每孔2×104个细胞。过夜培养后,用含有2mM GL凝胶的DMEM处理细胞,并在37℃下共培养◦用PBS洗涤处理过的细胞,并在室温下用4%(w/v)多聚甲醛固定15分钟。然后,用FITCphalloidin对细胞染色1小时,然后对细胞核酸进行DAPI染色15分钟。洗涤后,用LSM 700共聚焦激光扫描显微镜成像系统对细胞进行成像。 溶血试验[4] 通过以2000rpm离心5分钟从大鼠血液中分离红细胞(RBC)。沉淀的RBC在使用前用PBS洗涤3次。将红细胞悬浮在体积浓度为2%的PBS中,并补充终浓度为1-2mM的GL凝胶。用PBS和水处理的红细胞分别设置为阴性对照和阳性对照。在37℃下孵育2小时后,将处理过的红细胞以2000 rpm离心5分钟。使用酶标仪测量上清液在545 nm处的吸光度。溶血率使用以下方程式计算。 用于转染TGR5的CHO-K1细胞[2] 如前所述,使用成年中国仓鼠的卵巢从CHO细胞系制备CHO-K1细胞。在目前的实验中,根据我们之前的报告,使用人TGR5 cDNA的表达载体转染CHO-K1细胞。第二天,Western blot证实转染成功。然后,表达TGR5的细胞用于甘草酸(GA)处理。 细胞葡萄糖摄取的测量[2] 2-(N-(7-硝基苯-2-氧杂-1,3-二唑-4-基)氨基)-2-脱氧葡萄糖(2-NBDG)用于使用这种荧光葡萄糖类似物测定葡萄糖摄取,如我们之前的报告所述。使用荧光分光光度计测定每个细胞样品中的荧光强度。用BCA试剂盒测定蛋白质。然后,在接受甘草酸(GA)处理的细胞中定量2-NBDG的摄取。在预处理30分钟后,还将氨苯蝶啶的有效性与赋形剂治疗组进行了比较。 细胞中cAMP的测定[2] 按照我们之前的方法,用甘草酸(GA)处理细胞72小时。然后用ELISA试剂盒测定细胞内cAMP水平,类似于我们之前的法。每次测量都进行了两次。 细胞外GLP-1的测定[2] 我们使用NCI-H716细胞(每孔5×105个细胞)在37°C下用指定浓度的甘草酸(GA)处理1小时。然后,根据我们之前的方法,使用ELISA试剂盒分析细胞外GLP-1水平。对指定样品进行每次重复测量。 细胞培养与处理[6] 小鼠成纤维细胞系3T6购自中国科学院细胞库。细胞在添加10% FBS的DMEM中培养,在湿度为95%空气和5% CO2的37℃环境中培养。 甘草酸/Glycyrrhizic acid (GA)在DMSO中溶解成180mm浓原液,用PBS稀释成9mm工作液。分别用5、10、25、50、100、200 μM GA处理3T6细胞24 h,采用乳酸脱氢酶活性测定试剂盒测定条件培养基中乳酸脱氢酶(LDH)活性,分析细胞毒性。在后续实验中,分别选择低剂量(25 μM)、中剂量(50 μM)和高剂量(100 μM)的GA处理细胞。 增殖试验[6] 采用3-(4,5-二甲基噻唑-2-基)-2,5-二苯基溴化四氮唑(MTT)法测定细胞增殖情况。3T6细胞以每孔3000个细胞的密度接种于96孔微孔板中,37°C培养24 h。每孔中加入Glycyrrhizic acid (GA)/甘草酸(GA)至指定的终浓度(0、25、50或100 μM)。GA处理24或48 h后,将MTT加入培养基中,终浓度为0.2 mg/ml, 37℃孵育4 h。然后,抽吸培养基,在每孔200 μl DMSO中使甲醛晶体完全溶解。用ELX-800型微孔板仪记录490 nm处的光密度。每个分析点在5个重复中进行。 流式细胞术分析细胞周期和凋亡[6] 甘草酸/Glycyrrhizic acid (GA)处理24 h后,流式细胞术分析细胞周期和凋亡情况。为了分析细胞周期,收集细胞,在70%乙醇中4°C固定2 h,与碘化丙啶(PI)溶液在37°C下黑暗孵育30 min,然后在FACSCalibur流式细胞仪上分析。按照说明书使用Annexin V-FITC/PI细胞凋亡检测试剂盒检测细胞凋亡。染色后用流式细胞术分析细胞凋亡情况。 抓伤试验[6] 细胞迁移是通过成熟的体外划伤实验来评估的(Liang等,2007)。用5 μM丝裂霉素c孵育3T6细胞2 h,抑制细胞增殖。用200 μl移液管尖端水平穿过细胞单层表面均匀划痕。将分离的细胞用无血清培养基洗净,在37℃5% CO2培养箱中,用浓度Glycyrrhizic acid (GA)的无血清培养基培养24 h。在抓伤后0、6、12、24 h倒置显微镜下拍摄细胞,计算创面愈合率为(原始间隙距离-指定时间点的间隙距离)/原始间隙距离× 100%。 Transwell Assay [6] 3T6细胞用5 μM丝裂霉素- c预处理2 h,在浓度甘草酸的培养基中重悬。将200 μl悬液中的2 × 104个细胞置于预涂有Matrigel的Transwell腔中。将Transwell室置于24孔板中,每孔含800 μl培养基,培养基中添加20% FBS。37℃,5% CO2气氛下培养24 h。然后擦拭Transwell膜上表面的细胞和基质,用多聚甲醛固定膜下表面的细胞,并用结晶紫染色。在200 ×倒置显微镜下观察细胞,在每个膜上的5个视野中计数入侵细胞的数量。 |
| 动物实验 |
Animal/Disease Models: Iodine-induced autoimmune thyroiditis mouse model [3]
Doses: 50 mg/kg Route of Administration: intraperitoneal (ip) injection, one time/day, Results lasting for 4 weeks: diminished serum TgAb, HMGB1, TNF-α, IL-6, IL-1β levels. Reduce the prevalence and lymphocyte infiltration of thyroiditis and reduce the severity of thyroiditis. Assay of plasma glucose and GLP-1 levels in diabetic rats [2] Diabetic rats were orally treated with 5 mg/kg/day sitagliptin to inhibit DPP-4 or vehicle for two week before the administration of Glycyrrhizic acid (GA). Rats were fasted overnight without water restriction before the experiment. Then, Glycyrrhizic acid (GA) at desired dose was administrated to rats by intraperitoneal injection with or without pretreatment with sitagliptin for 30 min. The blood samples were collected 1 h after administration of Glycyrrhizic acid (GA) from the femoral vein of rats under pentobarbital anaesthesia (30 mg/kg, i.p.). The plasma glucose levels were measured in an automatic analyzer as described previously. The plasma GLP-1 levels were estimated with a commercial ELISA kit, as described in our previous report. A total of 80 male NOD.H-2h4 mice were randomly divided into a control or iodine supplement (NaI) group at four weeks of age, and the control group was fed with regular water, whereas the NaI group was supplied with 0.005% sodium iodine water. Another 24 male NOD.H-2h4 mice were also randomized into three groups (eight mice per group) as follows: control, NaI, and GL treatment after iodine supplementation (NaI + GL). The NOD.H-2h4 mice were fed with 0.005% sodium iodide water for eight weeks to enhance autoimmune thyroiditis. After iodine treatment, the mice received intraperitoneal injections of GL for four weeks. The severity of lymphocytic infiltration in the thyroid gland was measured by histopathological studies. The serum levels of HMGB1, tumor necrosis factor alpha, interleukin (IL)-6, IL-1β, and thyroglobulin antibody titers were measured using an enzyme-linked immunosorbent assay. HMGB1 expression was measured by immunohistochemical staining and real-time polymerase chain reaction. TLR2, HMGB1, MyD88, and nuclear transcription factor κB were measured by Western blot.[3] Establishment of BLM-induced Pulmonary Fibrosis in Rats and Glycyrrhizic acid (GA) Treatment [6] Forty male 8-weeks-old Sprague-Dawley rats, weighing around 250 g, were used in this study. The rats were randomly divided into five groups with eight rats in each group: control, BLM, BLM+GA50, BLM+GA100, and BLM+GA200. Induction of pulmonary fibrosis with BLM was conducted according to a previously described method (Thrall et al., 1979). All rats were anesthetized with 10% hydrate chloride at 3.5 ml/kg body weight (bw). Following anesthesia, a midline cut of the neck skin was made, and the trachea was exposed by blunt dissection. The needle of 1 ml syringe was inserted into the trachea, and bleomycin, dissolved in 100 μl sterile saline, was injected into the rat’s lungs at a dose of 5 mg/kg bw, while an equal volume of saline was injected into the rats from the Control group. The rats were rotated immediately after injection to ensure an even distribution of BLM in the lungs, and then the neck skin incision was sewn. Thereafter, the rats from the BLM+GA50, BLM+GA100, and BLM+GA200 groups received an intraperitoneal injection of GA at a dose of 50, 100, and 200 mg/kg bw respectively every day for a total of 28 days, and the rest animals received saline. The rats were sacrificed 28 days after BLM induction, the bronchoalveolar lavage fluids (BALFs) were collected by intratracheal instillation and draining of 1.5 ml saline for three times, and then the lungs were excised for further analysis. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Glycyrrhizic acid is mainly absorbed after presystemic hydrolysis and formation of glycyrrhetinic acid. Therefore, after oral administration of a dose of 100 mg of glycyrrhizic acid, this major metabolite appears in plasma in a concentration of 200 ng/ml while glycyrrhizic acid cannot be found. The finding of a minimal amount of glycyrrhizic acid in urine suggests the existence of a partial absorption in the gastrointestinal tract. Glycyrrhizic acid presents a biphasic elimination from the central compartment with a dose-dependent second elimination phase. The majority of the administered dose is eliminated by the bile in which glycyrrhizic acid can be eliminated unchanged and undergoes enterohepatic cycling. On the other hand, the major metabolite, glycyrrhetinic acid, forms glucuronide and sulfate conjugates. These conjugates are efficiently transported into the bile and duodenum where commensal bacteria hydrolizes the conjugate for the formation of glycyrrhetinic acid and further reabsorption. This reabsorption behavior seems to be related to the activity of 3-alpha-hydroxysteroid dehydrogenase which transports very efficiently the metabolite from the plasma to the bile. About 1.1-2.5% of the administered dose of glycyrrhizic acid can be found in urine which corresponds to the minimal cycling and reabsorption of this compound. The apparent volume of distribution of glycyrrhizic acid either in the central compartment and in steady-state are in the range of 37-64 ml/kg and 59-98 ml/kg, respectively. The constant reabsorption of glycyrrhetic acid in the duodenum causes a delay in the terminal plasma clearance. The reported total body clearance of glycyrrhizic acid is reported to be in the range of 16-25 ml.kg/h. GLYCYRRHIZIN WAS ABSORBED IN RAT SMALL INTESTINE; THERE WAS NO DETECTABLE AMT OF GLYCYRRHETINIC ACID IN BLOOD AFTER BOLUS INJECTION OF GLYCYRRHIZIN INTO PORTAL VEIN; GLYCYRRHETINIC ACID WAS PRESENT IN DETECTABLE AMT IN BLOOD AFTER ORAL ADMIN. Glycyrrhizic acid (GZA) and glycyrrhetinic acid (GRA) can be determined rapidly and precisely by high-performance liquid chromatography (HPLC) in biological fluids and tissues from experimental animals and humans. From plasma and tissues, glycyrrhizic acid and glycyrrhetinic acid are extracted by organic solvents and the extracts can directly be used for HPLC. From bile or urine, extraction and determination of glycyrrhizic acid and glycyrrhetinic acid are more difficult due to interfering endogenous compounds and conjugation of glycyrrhetinic acid with glucuronides or sulfates. Extraction of glycyrrhizic acid and glycyrrhetinic acid from urine or bile can be performed by ion-pairing followed by extraction with organic solvents or by solid phase extraction. Glycyrrhetinic acid conjugates can be determined by chromatographic separation or by pretreatment with beta-glucuronidase. The pharmacokinetics of glycyrrhetinic acid and glycyrrhizic acid can be described by a biphasic elimination from the central compartment with a dose-dependent second elimination phase. Depending on the dose, the second elimination phase in humans has a half-life of 3.5 hours for glycyrrhizic acid and between 10-30 hours for glycyrrhetinic acid. The major part of both glycyrrhetinic acid or glycyrrhizic acid is eliminated by the bile. While glycyrrhizic acid can be eliminated unmetabolized and undergoes enterohepatic cycling, Glycyrrhetinic acid is conjugated to glycyrrhetinic acid glucuronide or sulfate prior to biliary excretion. Orally administered glycyrrhizic acid is almost completely hydrolyzed by intestinal bacteria and reaches the systemic circulation as glycyrrhetinic acid. Glycyrrhizic acid is currently of clinical interest for treatment of chronic hepatitis. It is also applied as a sweetener in food products and chewing tobacco. In some highly exposed subgroups of the population, serious side effects such as hypertension and electrolyte disturbances have been reported. In order to analyze the health risks of exposure to this compound, the kinetics of glycyrrhizic acid and its active metabolites were evaluated quantitatively. Glycyrrhizic acid and its metabolites are subject to complex kinetic processes, including enterohepatic cycling and presystemic metabolism. In humans, detailed information on these processes is often difficult to obtain. Therefore, a model was developed that describes the systemic and gastrointestinal tract kinetics of glycyrrhizic acid and its active metabolite glycyrrhetic acid in rats. Due to the physiologically based structure of the model, data from earlier in vitro and in vivo studies on absorption, enterohepatic cycling, and presystemic metabolism could be incorporated directly. The model demonstrates that glycyrrhizic acid and metabolites are transported efficiently from plasma to the bile, possibly by the hepatic transfer protein 3-alpha-hydroxysteroid dehydrogenase. Bacterial hydrolysis of the biliary excreted metabolites following reuptake of glycyrrhetic acid causes the observed delay in the terminal plasma clearance of glycyrrhetic acid. These mechanistic findings, derived from analysis of experimental data through physiologically based pharmacokinetic modeling, can eventually be used for a quantitative health risk assessment of human exposure to glycyrrhizic acid containing products. Copyright 2000 Academic Press. To assess the multiplicity for the biliary excretion of xenobiotic conjugates, glycyrrhizic acid (glycyrrhizin) was studied in rats after intravenous (IV) injection of 10 mg/kg glycyrrhizic acid and IV infusion of inhibitors, dibromosulfophthalein and indocyanine green. Indocyanine green did not affect the biliary excretion of glycyrrhizic acid, whereas dibromosulfophthalein reduced it significantly. The plasma level of glycyrrhizic acid was increased by dibromosulfophthalein, but not by indocyanine green. In Eisai hyperbilirubinemic rats, the biliary excretion of glycyrrhizic acid was severely impaired, resulting in an increased plasma level. The findings suggested that the biliary excretion of glycyrrhizic acid is mediated by the system shared by liquiritigenin glucuronides and dibromosulfophthalein, but not by indocyanine green, and that the system is hereditarily defective in Eisai hyperbilirubinemic rats. Metabolism / Metabolites When orally administered, glycyrrhizic acid is almost completely hydrolyzed by intestinal bacteria for the formation of glycyrrhetinic acid, which is an active metabolite and can enter systemic circulation, and two molecules of glucuronic acid. This metabolite is transported and taken in the liver for its metabolization to form glucuronide and sulfate conjugates. BOLUS INJECTION OF GLYCYRRHIZIN GIVEN RATS IN PORTAL VEIN, GAVE RISE IN BLOOD LEVEL OF SUBSTANCE WHICH APPEARS TO BE GLUCURONIC ACID CONJUGATE FORMED AS METABOLITE OF GLYCYRRHETINIC ACID. Biological Half-Life Depending on the dose, the second elimination phase in humans has a half-life of 3.5 hours. |
| 毒性/毒理 (Toxicokinetics/TK) |
Effects During Pregnancy and Lactation
◉ Summary of Use during Lactation Licorice (Glycyrrhiza glabra) root contains glycyrrhizin (also called glycyrrhizic acid or glycyrrhizinic acid) and a mixture of the potassium and calcium salts of glycyrrhizic acid. Glycyrrhizin is metabolized to the active glycyrrhetinic acid in the intestine. Deglycyrrhizinated licorice (DGL) has had glycyrrhizin removed. Licorice is a purported galactogogue, and is included in some Asian proprietary mixtures to increase milk supply; however, no scientifically valid clinical trials support this use. In fact, licorice usually reduces serum prolactin, which might decrease milk production in the early stages of lactation. Women taking licorice have experienced elevated blood pressure. Galactogogues should never replace evaluation and counseling on modifiable factors that affect milk production. Some mothers in Türkiye reportedly use licorice to improve the taste and quality of their milk. Glycyrrhizin is detectable in the breastmilk of some women taking licorice, but studies measuring glycyrrhetinic acid have not been performed. Licorice has been used safely and effectively in combination with other herbs given to infants as a tea for the short-term treatment of colic. However, two infants whose mothers had an excessive intake of an herbal tea that contained licorice had signs of anethole toxicity. Because both of these papers reported on herbal mixtures, the effect(s) of licorice alone cannot be determined. Licorice and licorice extract are "generally recognized as safe" (GRAS) as foods by the U.S. Food and Drug Administration. Long-term, excessive use of licorice can cause hypertension, hypokalemia, and disturbances of adrenal hormones, and therefore should probably be avoided during nursing. Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to prove the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does not certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information about dietary supplements is available elsewhere on the LactMed Web site. ◉ Effects in Breastfed Infants Two breastfed infants, aged 15 and 20 days, were admitted to the hospital for a reported lack of weight gain in the previous 7 to 10 days, caused by "difficult feeding". The parents reported restlessness and vomiting during the past day. One of the mothers also reported feeling drowsy and weak. On examination, the infants were afebrile but had hypotonia, lethargy, emesis, weak cry, poor sucking and weak responses to painful stimuli. Infant laboratory values, electrocardiograms and blood pressures were normal, and septic work-ups were negative. Both mothers had both been drinking more than 2 liters daily of an herbal tea mixture reportedly containing licorice, fennel, anise, and goat's rue to stimulate lactation. After the mothers discontinued breastfeeding and the herbal tea, the infants improved within 24 to 36 hours. Symptoms of the affected mother also resolved rapidly after discontinuing the herbal tea. After 2 days, breastfeeding was reinstituted with no further symptoms in the infants. Both infants were doing well at 6 months of age. The authors attributed the maternal and infant symptoms to anethole, which is found in both anise and fennel; however, the anethole levels were not measured in breastmilk, nor were the teas tested for their content. ◉ Effects on Lactation and Breastmilk A woman with a history of excessive licorice intake had amenorrhea, severe headaches, hypertension, hypokalemia. She had elevated serum prolactin levels that remained abnormal for one month after licorice discontinuation and normalized by 6 months after discontinuation. In a study of 25 men and 25 women, the baseline and thyrotropin-stimulated serum prolactin levels were measured to determine normal serum prolactin values. Subjects who regularly ingested licorice had lower basal and lower stimulated serum prolactin concentrations. A traditional, nonstandardized decoction of peony and licorice roots called Shaoyao-Gancao-Tang in Chinese and Shakuyaku-Kanzo-To in Japanese was studied in women with elevated serum prolactin caused by long-term (>6 months) ingestion of risperidone. Patients received either bromocriptine 5 mg daily for 4 weeks followed by 4 weeks of 22.5 grams daily of the peony-licorice decoction (equivalent to 25 mg of glycyrrhetinic acid), or the same drugs in the reverse order. Evaluation of serum prolactin found that both treatments reduced serum prolactin by 21 to 28% from baseline at 4 and 8 weeks. Forty women who complained of an insufficient milk supply at 5 days postpartum were given a combination herbal supplement as 2 capsules of Lactare (Pharma Private Ltd., Madras, India; currently available from TTK Pharma, Chennai, India) 3 times daily. Each capsule contained wild asparagus 200 mg, ashwagandha (Withania somnifera) 100 mg, fenugreek 50 mg, licorice 50 mg, and garlic 20 mg. By day 4 of therapy, no infants required supplementary feeding. Infants were weighed before and after each feeding on the fifth day of maternal therapy to determine the amount of milk ingested. On the day of the test weighing, infants' milk intake averaged 388 mL, and the fluid and caloric intake was considered adequate. This study cannot be considered as valid evidence of a galactogogue effect of these herbs because it lacks randomization, blinding, a placebo control, and maternal instruction in breastfeeding technique. Additionally, infants were breastfed only 6 to 8 times daily, which is insufficient to maximize milk supply at this stage of lactation. Women who were between 14 and 90 days postpartum and reported lactation failure were given instructions on breastfeeding technique and encouraged to exclusively breastfeed. If their infant had gained less than 15 grams in 1 week, they were randomized to receive either two tablespoonfuls of a mixture containing wild asparagus or an identical placebo for 4 weeks. In each 100 grams, the mixture contained Asparagus racemosus 15 grams, Anethum soiva 1 gram, Ipomea digitata 1 gram, Glycyrrhiza glabra 1 gram, Spinacia oleracea 2.5 grams, Cuminum cyminum 0.5 gram, and panchatrinamol 1 gram. Of the 64 women randomized, 11 did not complete the trial. Serum prolactin measurements were made before a morning nursing before treatment and after 4 weeks of treatment. Infant weight gains and the number of supplemental feedings were recorded initially and after 4 weeks of therapy. No differences were found in the changes in serum prolactin, infant weight gain or amount of supplementation between the treatment and placebo groups after 4 weeks of therapy. No side effects or changes in liver function tests occurred during the study. A study in Japan compared the use of a mixture of 13 herbs, including licorice, to ergonovine for their effects on lactation and serum prolactin in postpartum women. The herbal mixture, called Xiong-gui-tiao-xue-yin, was given in a randomized fashion to 41 women in a dose of 2 grams of a dried aqueous extract 3 times daily. A comparable group of 41 women were randomized to receive methylergonovine 0.375 mg daily. Therapy was started on the day of delivery, but the duration of therapy was not specified. Plasma oxytocin and prolactin were measured on days 1 and 6; milk volumes were measured daily, although the method of measuring milk volume was not specified. Serum prolactin was higher on days 1 and 6 in the women who received the herbals; plasma oxytocin was lower on day 1 in the women who received the herbal, but not different on day 6. Milk volumes were greater on days 4, 5, and 6 in women who received the herbal mixture. This study has serious flaws that make its interpretation impossible. First, milk volume measurement is subject to considerable variability depending on the measurement method used, but the method was not specified. Second, methylergonovine has caused decreases in serum prolactin and milk production in some studies. Because of the lack of a placebo group, the differences found could be a negative effect of methylergonovine rather than a positive effect of the herbal preparation. Because this study used a multi-ingredient combination product in which licorice was only one component, the results might be different from studies in which licorice was used alone. In an uncontrolled, non-blinded multicenter study in India, 1132 patients who reported inadequate milk supply were give a mixture (Lactancia, Corona Remedies Pvt. Ltd.) To take in a dose of 30 grams twice daily. The product contains Asparagus racemosus (wild asparagus, shatavari), Cuminum cyminum (cumin), Glycyrrhiza glabra (licorice), Spinacia oleracea (spinach) as well as amino acids, vitamins, minerals and DHA. Most of the mothers (1049) had improved lactation and increased infant weight. However, with no placebo control group, results cannot be attributed to the product. Protein Binding Glycyrrhizic acid does not bind to any plasma proteins as it is not absorbed systemically. On the other hand, its main active metabolite, glycyrrhetinic acid presents a very large binding to serum proteins such as albumin. |
| 参考文献 |
|
| 其他信息 |
Glycyrrhizinate dipotassium is an organic molecular entity.
A widely used anti-inflammatory agent isolated from the licorice root. It is metabolized to GLYCYRRHETINIC ACID, which inhibits 11-BETA-HYDROXYSTEROID DEHYDROGENASES and other enzymes involved in the metabolism of CORTICOSTEROIDS. Therefore, glycyrrhizic acid, which is the main and sweet component of licorice, has been investigated for its ability to cause hypermineralocorticoidism with sodium retention and potassium loss, edema, increased blood pressure, as well as depression of the renin-angiotensin-aldosterone system. See also: Glycyrrhizin (has active moiety); Glycyrrhiza Glabra (part of); Glycyrrhizinate dipotassium; xylitol (component of) .. Glycyrrhizic acid (GA) is belonged to triterpenoid saponin that is contained in the root of licorice and is known to affect metabolic regulation. Recently, glucagon like peptide-1 (GLP-1) has widely been applied in diabetes therapeutics. However, the role of GLP-1 in GA-induced anti-diabetic effects is still unknown. Therefore, we are interested in understanding the association of GLP-1 with GA-induced effects. In type 1-like diabetic rats induced by streptozotocin (STZ-treated rats), GA increased the level of plasma GLP-1, which was blocked by triamterene at a dose sufficient to inhibit Takeda G-protein-coupled receptor 5 (TGR5). The direct effect of GA on TGR5 has been identified using the cultured Chinese hamster ovary cells (CHO-K1 cells) transfected TGR5 gene. Moreover, in intestinal NCI-H716 cells that secreted GLP-1, GA promoted GLP-1 secretion with a marked elevation of calcium levels. However, both effects of GA were reduced by ablation of TGR5 with siRNA in NCI-H716 cells. Therefore, we demonstrated that GA can enhance GLP-1 secretion through TGR5 activation.[2] Taken together, we demonstrated for the first time that GA could increase plasma GLP-1 level via TGR5 activation in tyep 1-like diabetic rats. Therefore, GA could have future applications in the clinic. [2] igh mobility group box-1 (HMGB1), a non-histone protein, plays an important role in autoimmune diseases. However, the significance of HMGB1 in the pathogenesis of autoimmune thyroiditis has not been reported. The purpose of this study was to explore whether HMGB1 participates in the pathogenesis of autoimmune thyroiditis, and whether glycyrrhizin (GL), a direct inhibitor of HMGB1, attenuates the severity of thyroid inflammatory infiltration in a murine model of autoimmune thyroiditis.[3] Injectable low-molecular-weight hydrogels (LMWHs) from biocompatible materials have attracted much attention in biomedical applications because they can adapt any desired sizes and cavity shapes. Searching for simple, biocompatible injectable LMWHs owning inherent antibacterial activity without complicated chemical modification remains an open question to avoid the tedious synthesis/purification process and the easy bacterial infection of hydrogels in a moist environment. In this work, glycyrrhizic acid (GL), a naturally occurring compound, was found to form a stable transparent LMWH at 37 °C in physiological phosphate buffered saline (PBS) with nanoclusters as the microstructures. Moreover, this hydrogel exhibited great injectable and moldable properties. The antibacterial study showed that the growth of Gram-positive Staphylococcus aureus (S. aureus) could be completely inhibited by GL, whereas noneffect on Gram-negative Escherichia coli (E. coli) was observed. In addition, cell viability and hemolysis assay revealed that GL had good biocompatibility and hemocompatibility to mammalian cells because of its natural origin. Our simple biocompatible injectable moldable LMWH with inherent antibacterial ability has potential in the area of biomaterials and 3D bioprinting. In summary, we used natural glycyrrhizic acid as a gelator to construct a stable LMWH at 37 °C in physiological PBS without additional chemical modification. This nanocluster-structured LMWH exhibited great injectable and moldable properties. Moreover, the growth of Gram-positive S. aureus could be completely inhibited by GL compared with Gram-negative E. coli. In addition, cell viability and hemolysis assays revealed that GL has low cytotoxicity and good hemocompatibility to mammalian cells because of its natural origin. Our work provides a simple, biocompatible injectable moldable LMWH with inherent antibacterial ability, which will be of great interest in the area of biomaterials and 3D bioprinting.[4] Excessive macroautophagy/autophagy is one of the causes of cardiomyocyte death induced by cardiovascular diseases or cancer therapy, yet the underlying mechanism remains unknown. We and other groups previously reported that autophagy might contribute to cardiomyocyte death caused by sunitinib, a tumor angiogenesis inhibitor that is widely used in clinic, which may help to understand the mechanism of autophagy-induced cardiomyocyte death. Here, we found that sunitinib-induced autophagy leads to apoptosis of cardiomyocyte and cardiac dysfunction as the cardiomyocyte-specific Atg7-/+ heterozygous mice are resistant to sunitinib. Sunitinib-induced maladaptive autophagy selectively degrades the cardiomyocyte survival mediator CCN2 (cellular communication network factor 2) through the TOLLIP (toll interacting protein)-mediated endosome-related pathway and cardiomyocyte-specific knockdown of Ccn2 through adeno-associated virus serotype 9 (AAV9) mimics sunitinib-induced cardiac dysfunction in vivo, suggesting that the autophagic degradation of CCN2 is one of the causes of sunitinib-induced cardiotoxicity and death of cardiomyocytes. Remarkably, deletion of Hmgb1 (high mobility group box 1) inhibited sunitinib-induced cardiomyocyte autophagy and apoptosis, and the HMGB1-specific inhibitor glycyrrhizic acid (GA) significantly mitigated sunitinib-induced autophagy, cardiomyocyte death and cardiotoxicity. Our study reveals a novel target protein of autophagic degradation in the regulation of cardiomyocyte death and highlights the pharmacological inhibitor of HMGB1 as an attractive approach for improving the safety of sunitinib-based cancer therapy. [5] |
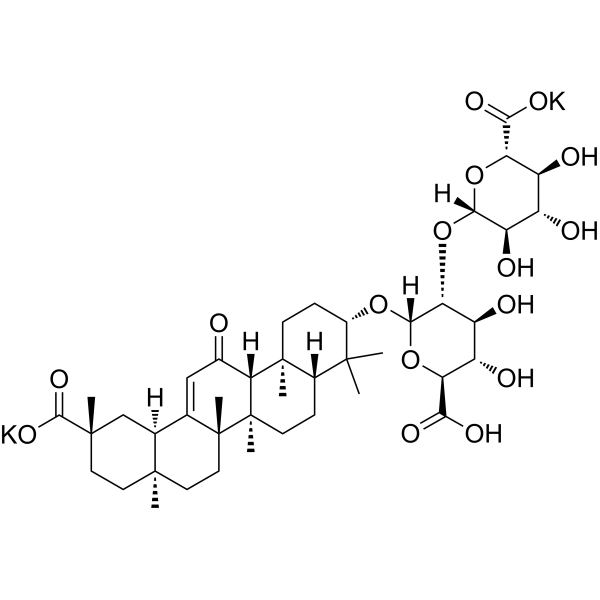
| 分子式 |
C42H60K2O16
|
|---|---|
| 分子量 |
899.1128
|
| 精确质量 |
898.315
|
| CAS号 |
68797-35-3
|
| 相关CAS号 |
Ammonium glycyrrhizinate;53956-04-0;Glycyrrhizic acid;1405-86-3
|
| PubChem CID |
656852
|
| 外观&性状 |
White to off-white solid powder
|
| tPSA |
272.7
|
| 氢键供体(HBD)数目 |
6
|
| 氢键受体(HBA)数目 |
16
|
| 可旋转键数目(RBC) |
5
|
| 重原子数目 |
60
|
| 分子复杂度/Complexity |
1720
|
| 定义原子立体中心数目 |
19
|
| SMILES |
C[C@]12CC[C@](C[C@H]1C3=CC(=O)[C@@H]4[C@]5(CC[C@@H](C([C@@H]5CC[C@]4([C@@]3(CC2)C)C)(C)C)O[C@@H]6[C@@H]([C@H]([C@@H]([C@H](O6)C(=O)[O-])O)O)O[C@H]7[C@@H]([C@H]([C@@H]([C@H](O7)C(=O)[O-])O)O)O)C)(C)C(=O)O.[K+].[K+]
|
| InChi Key |
BIVBRWYINDPWKA-VLQRKCJKSA-L
|
| InChi Code |
InChI=1S/C42H62O16.2K/c1-37(2)21-8-11-42(7)31(20(43)16-18-19-17-39(4,36(53)54)13-12-38(19,3)14-15-41(18,42)6)40(21,5)10-9-22(37)55-35-30(26(47)25(46)29(57-35)33(51)52)58-34-27(48)23(44)24(45)28(56-34)32(49)50;;/h16,19,21-31,34-35,44-48H,8-15,17H2,1-7H3,(H,49,50)(H,51,52)(H,53,54);;/q;2*+1/p-2/t19-,21-,22-,23-,24-,25-,26-,27+,28-,29-,30+,31+,34-,35-,38+,39-,40-,41+,42+;;/m0../s1
|
| 化学名 |
dipotassium;(2S,3S,4S,5R,6R)-6-[(2S,3R,4S,5S,6S)-2-[[(3S,4aR,6aR,6bS,8aS,11S,12aR,14aR,14bS)-11-carboxy-4,4,6a,6b,8a,11,14b-heptamethyl-14-oxo-2,3,4a,5,6,7,8,9,10,12,12a,14a-dodecahydro-1H-picen-3-yl]oxy]-6-carboxylato-4,5-dihydroxyoxan-3-yl]oxy-3,4,5-trihydroxyoxane-2-carboxylate
|
| 别名 |
Dipotassium glycyrrhizinate; Glycyrrhizinate dipotassium; 68797-35-3; Dipotassium glycyrrhizate; CHEBI:79402; CA2Y0FE3FX; Neubormitin; Glycyrrhizic acid dipotassium;
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
H2O : ~50 mg/mL (~55.61 mM)
DMSO : ~20.83 mg/mL (~23.17 mM) |
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: 100 mg/mL (111.22 mM) in PBS (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶。
请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.1122 mL | 5.5611 mL | 11.1221 mL | |
| 5 mM | 0.2224 mL | 1.1122 mL | 2.2244 mL | |
| 10 mM | 0.1112 mL | 0.5561 mL | 1.1122 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT04028869 | Completed | Drug: Glycyrrhizic acid preparation | Autoimmune Liver Disease | Beijing Ditan Hospital | March 1, 2018 | |
| NCT04742660 | Completed | Drug: Ammonium Glycyrrhizinate | Postoperative Nausea | Konkuk University Medical Center | May 11, 2021 | Not Applicable |
| NCT05895773 | Completed | Drug: Povidone-Iodine Drug: Saline spray |
Ventilator Associated Pneumonia | Menoufia University | June 24, 2023 | Phase 2 Phase 3 |
| NCT05788705 | Not yet recruiting | Dietary Supplement: "apigenin" and "glycyrrhizin" |
Rheumatoid Arthritis | Adel A.Gomaa | July 2023 | Not Applicable |