| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| 5g |
|
||
| 10g |
|
||
| Other Sizes |
|

| 靶点 |
EGFR (IC50 = 2 nM)
|
|---|---|
| 体外研究 (In Vitro) |
体外活性:Erlotinib HCl 有效抑制完整细胞中的 EGFR 活化,包括 HNS 人头颈肿瘤细胞 (IC50 20nM)、DiFi 人结肠癌细胞和 MDA MB-468 人乳腺癌细胞。 Erlotinib HCl (1 μM) 诱导 DiFi 人结肠癌细胞凋亡。厄洛替尼抑制一组 NSCLC 细胞系的生长,包括 A549、H322、H3255、H358 H661、H1650、H1975、H1299、H596,IC50 范围为 29 nM 至 >20 μM。 Erlotinib HCl(2 μM) 显着抑制 AsPC-1 和 BxPC-3 胰腺细胞的生长。厄洛替尼盐酸盐与吉西他滨联合使用在 KRAS 突变的胰腺癌细胞中被认为具有累加效应。 10 微摩尔的 Erlotinib HCl 可抑制 EGFR Y845(Src 依赖性磷酸化)和 Y1068(自动磷酸化)位点的磷酸化。与厄洛替尼盐酸盐联合使用可以下调雷帕霉素刺激的 Akt 活性,并对细胞生长抑制产生协同作用。激酶测定:96 孔板在 37°C 下孵育过夜,每孔加入 100 μL 0.25 mg/mL PGT 的 PBS 溶液。通过抽吸除去过量的PGT,并用洗涤缓冲液(PBS中的0.1% Tween 20)洗涤板3次。激酶反应在 50 μL 50 mM HEPES (pH 7.3) 中进行,其中含有 125 mM 氯化钠、24 mM 氯化镁、0.1 mM 原钒酸钠、20 μM ATP、1.6 μg/mL EGF 和 15 ng EGFR,亲和力从A431细胞膜纯化。添加 DMSO 中的厄洛替尼 HCl,使 DMSO 最终浓度为 2.5%。通过添加 ATP 启动磷酸化,并在室温下持续摇动 8 分钟。通过抽吸反应混合物终止激酶反应并用洗涤缓冲液洗涤4次。通过每孔 50 μL HRP 偶联的 PY54 抗磷酸酪氨酸抗体孵育 25 分钟来测量磷酸化 PGT,该抗体在封闭缓冲液(PBS 中的 3% BSA 和 0.05% Tween 20)中稀释至 0.2 μg/mL。通过抽吸除去抗体,并用洗涤缓冲液洗涤板4次。通过添加 TMB Microwell 过氧化物酶底物(每孔 50 μL)来产生结肠测量信号,并通过添加 0.09 M 硫酸(每孔 50 μL)来终止。通过测量 450 nm 处的吸光度来估算磷酸酪氨酸。对照信号通常为 0.6-1.2 吸光度单位,在没有 AlP、EGFR 或 PGT 的孔中基本上没有背景,并且与 10 分钟的孵育时间成正比。细胞测定:将呈指数生长的细胞(A549、H322、H3255、H358 H661、H1650、H1975、H1299、H596 细胞)接种于 96 孔塑料板中,并暴露于埃罗替尼、培美曲塞或恒定浓度组合的连续稀释液中比例为 4:1,一式三份,持续 72 小时。通过细胞计数和 3-(4,5-二甲基噻唑-2-基)-2,5-二苯基四唑溴化物测定来测定细胞活力。生长抑制表示为药物处理的存活细胞与 PBS 处理的对照细胞的百分比(被认为是 100% 活力)。 IC50 值是与未处理的对照细胞相比,药物暴露 72 小时导致 50% 细胞生长抑制的浓度,并通过 CalcuSyn 软件计算。
表皮生长因子受体(EGFR)在很大比例的癌症中过表达,并导致恶性表型。CP-358774是一种直接作用的人EGFR酪氨酸激酶抑制剂,IC50为2 nM,可减少完整肿瘤细胞中的EGFR自磷酸化,IC50为20 nM。在分离激酶和全细胞的检测中,这种抑制对EGFR酪氨酸激酶的选择性高于我们检查过的其他酪氨酸激酶。在100mg/kg的剂量下,CP-358774完全阻止了EGF诱导的人HN5肿瘤中EGFR的自磷酸化,该肿瘤在无胸腺小鼠中作为异种移植物生长,并完全阻止了接受治疗的小鼠的肝EGFR自磷酸化。CP-358774在细胞培养物中以亚摩尔浓度抑制DiFi人结肠肿瘤细胞的增殖,并阻断G1期的细胞周期进程。这种抑制剂在DiFi细胞中产生低磷酸化形式的视网膜母细胞瘤蛋白的显著积累和p27KIP1的积累,这可能有助于细胞周期阻滞。根据DNA片段的形成和其他标准,抑制EGFR也会触发这些细胞的凋亡。这些结果表明,CP-358774具有治疗依赖EGFR途径增殖或存活的肿瘤的潜力。[1] B-DIM和厄洛替尼对胰腺癌症细胞生存能力的影响[2] 值得注意的是,在我们的试点研究中,如材料和方法所示,使用了不同浓度的B-DIM和厄洛替尼,如表1所示。此外,在分析了EGFR、NF-κB和COX-2的基础表达水平后,我们选择了两种细胞系(BxPC-3),其NF-κB、EGFR和COX-2的表达水平为组成型激活水平,而NF-κA、EGFR和COX-2的表达水平较低(MIAPaCa)。我们的结果促使我们选择B-DIM和厄洛替尼的后续浓度,如下所示。用B-DIM(20µmol/L)、埃洛替尼(2µmol/L)和组合处理的BxPC-3和MIPaCa胰腺癌症细胞的细胞活力通过MTT测定进行测定,数据如图1A和B所示。在用任一药剂处理的Bx PC-3细胞中观察到细胞活力的显著抑制,联合处理进一步增强了细胞活力(P=0.0001)。此外,我们还通过克隆形成试验测试了治疗对细胞存活率的影响,如下所示。MIAPaCa细胞的类似处理导致单独使用B-DIM显著抑制活细胞,但当同时暴露于类似浓度的B-DIM和厄洛替尼时则没有,联合治疗没有增强这种效果(P=0.0890)。MIAPaCa细胞对厄洛替尼的不敏感性与最近发表的一份报告一致 克隆形成试验抑制细胞生长/存活[2] 为了确定B-DIM和厄洛替尼对细胞生长的影响,用每种单一药物或其组合处理细胞,并通过克隆形成试验评估细胞存活率。与单独使用任何一种药物相比,B-DIM和厄洛替尼的组合显著抑制了BxPC-3细胞中的集落形成(图2A和B)。MIAPaCa细胞的类似处理(图2C)显示,单独使用B-DIM和联合使用都能抑制集落形成,但联合使用并不能增强这种效果,如BxPC-3细胞所示(图2A和B)。这些结果与软琼脂试验获得的结果相似。总的来说,克隆发生测定的结果与MTT数据一致,如图1A和B所示,表明B-DIM在BxPC-3和MIPaCa胰腺癌症细胞之间具有不同的作用。这些差异的机制得到了进一步的研究,结果将在以下部分呈现,但首先我们确定了B-DIM、厄洛替尼和联合用药对凋亡细胞死亡的影响。 厄洛替尼、B-DIM和联合用药诱导细胞凋亡[2] 通过使用细胞死亡检测ELISA确定不同处理的凋亡效应,进一步研究了抑制细胞存活的潜在机制。与单独使用任何一种药物的凋亡作用相比,B-DIM和厄洛替尼的组合仅在BxPC-3细胞中显著诱导了凋亡(图1C)。对MIAPaCa细胞的类似处理显示,联合用药没有诱导细胞凋亡(图1D)。这些结果与MTT法的细胞存活率测定结果一致。随后,我们试图找到进一步的凋亡证据,如下所述。 B-DIM通过厄洛替尼增强细胞凋亡信号传导[2] 在用B-DIM(20µmol/L)、厄洛替尼(2µmol/L)和组合处理的BxPC-3和MIAPaCa细胞中测定了PARP切割(图3)。我们仅在BxPC-3细胞中发现了72小时处理后大量PARP(116 kDa)蛋白切割产物(85 kDa片段)(图3)。相比之下,经类似处理的MIAPaCa细胞仅显示出单独使用B-DIM和联合使用但不单独使用厄洛替尼对PARP的小切割。凋亡的诱导可能部分是由于重要存活基因的失活;因此,我们研究了B-DIM、厄洛替尼及其组合是否会影响关键的生存蛋白。 B-DIM对凋亡相关分子的影响[2] 使用BxPC-3和MIAPaCa细胞来评估B-DIM和/或厄洛替尼对存活素、Bcl-2、Bcl-xL和c-IAP1/2表达的影响。与单独使用任何一种药物相比,联合治疗的细胞中Bcl-2、Bcl-xL、survivin和c-IAP1/2蛋白的表达显著降低(图3)。单独或联合用药对MIAPaCa细胞中的抗凋亡蛋白没有影响。这些结果表明,B-DIM、厄洛替尼及其组合下调了关键存活蛋白,进而诱导BxPC-3细胞凋亡,但在MIAPaCa细胞中没有。为了进一步确定B-DIM致敏BxPC-3细胞对厄洛替尼诱导的细胞活力抑制和凋亡诱导的分子机制,我们研究了EGFR及其下游信号通路的作用。 B-DIM对EGFR蛋白表达的影响[2] 通过免疫印迹法测定EGFR的表达。在MIAPaCa细胞中未发现EGFR的基线表达。与单独使用任何一种药物相比,当暴露于厄洛替尼联合B-DIM时,表达EGFR的BxPC-3细胞显示出EGFR表达和磷酸化EGFR水平的显著降低(图3)。众所周知,EGFR的激活反过来可以调节一种重要的转录因子NF-κB,它是存活素、c-IAP1/2、Bcl-2和Bcl-xL等几种生存基因的已知调节因子。因为我们发现与单独使用B-DIM和厄洛替尼相比,BxPC-3细胞中survivin、c-IAP1/2、Bcl-2和Bcl-xL的下调程度更大,而且这些基因受NF-κB的转录调节,所以我们研究了每种处理对NF-κB DNA结合活性的影响。 B-DIM抑制NF-κBDNA结合活性[2] 在B-DIM处理和厄洛替尼处理的细胞中评估核转录因子NF-κB的激活。与单独使用埃罗替尼相比,暴露于埃罗替尼和B-DIM的BxPC-3细胞中NF-κB活化受到显著抑制(图4A)。MIAPaCa细胞中没有显示出这种抑制作用(图4B)。这些结果表明,B-DIM和厄洛替尼的组合对细胞生长、凋亡诱导、存活因子抑制、EGFR抑制和NF-κB失活有更大的抑制作用。 由于NF-κB在促生存和抗凋亡过程的调节中起着重要作用,我们测试了p65 cDNA转染NF-κB的过表达是否可以消除B-DIM诱导和厄洛替尼诱导的凋亡过程。此外,众所周知,NF-κB转录调节COX-2,COX-2产生PGE2,进而诱导细胞存活。因此,我们测试了塞来昔布、厄洛替尼或单独的B-DIM是否会影响p65 cDNA转染细胞中B-DIM和厄洛替尼的活性。 厄洛替尼、B-DIM和塞来昔布阻断p65 cDNA转染刺激的NF-κB活性的激活[2] 用p65 cDNA转染BxPC-3和MIAPaCa细胞,然后用厄洛替尼(2µmol/L)、B-DIM(20µmol/L)或塞来昔布(5µmol/L)处理或未处理48小时,对其细胞质和核蛋白进行NF-κB活性分析,通过蛋白质印迹分析和EMSA进行测量。结果显示,与未处理的细胞相比,厄洛替尼、B-DIM和塞来昔布对BxPC-3细胞中p65蛋白和NF-κB DNA结合活性的抑制作用更大(图5A和B),对MIAPaCa细胞的影响很小。重要的是,如图5A和B所示,NF-κB p65 cDNA转染仅在BxPC-3细胞中显著增强了NF-κBp65蛋白和DNA结合活性。另一方面,在MIAPaCa细胞中没有观察到这种变化。由于NF-κB的激活诱导COX-2表达,导致PGE2产生并释放到培养基中,我们测量了用埃罗替尼、B-DIM和COX-2抑制剂塞来昔布处理的未转染和转染细胞中PGE2的水平。 p65 cDNA转染细胞中PGE2合成的抑制[2] 我们测量了从BxPC-3和MIAPaCa细胞收集的条件培养基中PGE2的水平,作为COX-2活性的指标。我们发现BxPC-3细胞分泌高水平的PGE2,而MIAPaCa细胞显示出非常低的PGE2水平,这与COX-2的低组成性表达是一致的。用p65cDNA转染BxPC-3和MIAPaCa细胞,然后用厄洛替尼(10nmol/L)、B-DIM(1µmol/L)或塞来昔布(1nmol/L)处理,以分析释放到培养基中的PGE2水平(图5C)。单独用厄洛替尼处理细胞时,PGE2水平没有变化(P=0.084)。然而,在用B-DIM(P=0.006)和塞来昔布(P=0.005)处理的BxPC-3细胞中观察到PGE2水平显著降低。与未转染的细胞相比,p65 cDNA转染的BxPC-3细胞中PGE2水平显著升高(P=0.009),表明NF-κB可以诱导COX-2表达。然而,使用任何药物后,MIAPaCa细胞中的PGE2水平都没有变化。总的来说,这些结果表明PGE2的产生是通过NF-κB和COX-2途径介导的,塞来昔布可以下调NF-κB和COX-2。这些结果随后与凋亡程度相关(图5D),如下所示。 p65 cDNA转染细胞中NF-κB失活导致的细胞凋亡[1] 将p65 cDNA转染到BxPC-3和MIAPaCa细胞中,然后用厄洛替尼(2µmol/L)、B-DIM(20µmol/L)或塞来昔布(5µmol/L)处理48小时(图5D)。用厄洛替尼处理的p65 cDNA转染的BxPC-3细胞的凋亡程度(P=0.034)远低于用厄洛替尼处理的未转染细胞(P=0.007)。在BxPC-3细胞中,B-DIM和塞来昔布治疗均观察到类似的结果。然而,在MIAPaCa细胞中,没有观察到这种程度的凋亡。这些结果表明,p65 cDNA转染激活NF-κB可以消除厄洛替尼、B-DIM和塞来昔布的凋亡诱导作用。 |
| 体内研究 (In Vivo) |
在 100 mg/kg 的剂量下,Erlotinib HCl 完全阻止 EGF 诱导的人类 HN5 肿瘤中 EGFR 的自磷酸化,该肿瘤作为无胸腺小鼠的异种移植物以及治疗小鼠的肝脏 EGFR 的自磷酸化。 Erlotinib HCl (100 mg/Kg) 抑制 H460a 和 A549 肿瘤模型,抑制率分别为 71% 和 93%。
B-DIM增强厄洛替尼对原发性肿瘤的体内治疗效果[2] 研究了B-DIM和厄洛替尼组合在携带原位植入BxPC-3胰腺肿瘤细胞的SCID小鼠中的潜在治疗效用。选择每只小鼠口服3.5mg/d的B-DIM剂量,而厄洛替尼剂量(腹腔注射50mg/kg体重)基于之前发表的报告,如图6A所示。共28只小鼠分为四组。为了确定单一药物治疗与联合治疗的疗效,我们确定了所有治疗组的平均胰腺重量。在我们的实验条件下,与对照组肿瘤相比,通过强饲治疗和单独使用厄洛替尼给予B-DIM分别使肿瘤重量减轻了20%和35%(图6C)。然而,在实验条件下,与未经治疗的对照组、单独使用B-DIM或单独使用厄洛替尼治疗组相比,B-DIM和厄洛替尼联用治疗组的肿瘤重量显著降低(P<0.01)。这些结果首次表明,在原位模型中,B-DIM和厄洛替尼联合使用抑制胰腺肿瘤生长的疗效。 B-DIM在体内抑制NF-κBDNA结合活性[2] 在B-DIM治疗和厄洛替尼治疗的肿瘤组织中评估NF-κB的激活。结果表明,B-DIM和厄洛替尼下调了NF-κB(图6B)。图6B(底部)显示了所有七只小鼠的结果。这些体内结果与我们的体外发现相似,表明NF-κB的失活至少是B-DIM在我们的实验动物模型中增强厄洛替尼诱导的抗肿瘤活性的分子机制之一。 阻断表皮生长因子受体(EGFR)在急性肾损伤(AKI)中的作用存在争议。在这里,我们研究了厄洛替尼(一种可以阻断EGFR活性的选择性酪氨酸激酶抑制剂)对顺铂(CP)诱导的急性肾损伤的肾脏保护作用。从诱导CP肾毒性(CP-N)的前一天到第3天,给各组动物服用厄洛替尼或赋形剂。此外,我们使用人肾近端肾小管细胞(HK-2)分析了厄洛替尼对CP-N相关信号通路的影响。与对照组相比,厄洛替尼治疗的大鼠肾功能明显改善,肾小管间质损伤减轻,凋亡和增殖细胞数量减少。厄洛替尼治疗的大鼠肾皮质促纤维化基因的mRNA显著减少。厄洛替尼治疗显著降低了Bax/Bcl-2 mRNA和蛋白比值。在体外,我们观察到厄洛替尼显著降低了HK-2中CP诱导的MEK1和Akt的磷酸化过程。综上所述,这些数据表明厄洛替尼具有肾脏保护特性,这可能是通过减少肾小管细胞的凋亡和增殖来介导的,这些作用反映了对EGFR下游信号通路的抑制。这些结果表明,厄洛替尼可能有助于预防接受CP化疗的患者发生急性肾损伤[PLoS One. 2014 Nov 12;9(11):e111728.]。 |
| 酶活实验 |
包被 96 孔板的过程包括每孔加入 100 μL 0.25 mg/mL PGT 的 PBS 溶液,在 37 °C 下孵育一整夜。使用抽吸去除多余的 PGT,并对板进行 3 次洗涤缓冲液洗涤(PBS 中的 0.1% Tween 20)。使用 50 μL 50 mM HEPES (pH 7.3),其中含有 0.1 mM 原钒酸钠、125 mM 氯化钠、24 mM 氯化镁、20 μM ATP、1.6 μg/mL EGF 和来自 A431 细胞膜的 15 ng 亲和纯化的 EGFR用于激酶反应。通过在 DMSO 中添加盐酸厄洛替尼可达到 2.5% 的最终 DMSO 浓度。添加 ATP 后,磷酸化开始,并在室温下持续振荡八分钟。通过抽吸反应混合物终止激酶反应,并用洗涤缓冲液洗涤 4 次。通过每孔 50 μL HRP 偶联的 PY54 抗磷酸酪氨酸抗体孵育 25 分钟来测量磷酸化 PGT,该抗体在封闭缓冲液(PBS 中的 3% BSA 和 0.05% Tween 20)中稀释至 0.2 μg/mL。通过抽吸除去抗体,并用洗涤缓冲液洗涤板4次。通过添加 TMB Microwell 过氧化物酶底物(每孔 50 μL)来产生结肠测量信号,并通过添加 0.09 M 硫酸(每孔 50 μL)来终止。通过测量 450 nm 处的吸光度来估算磷酸酪氨酸。在没有 AlP、EGFR 或 PGT 的孔中,对照信号通常在 0.6 至 1.2 吸光度单位之间,几乎没有背景,并且与 10 分钟的孵育时间成正比。
|
| 细胞实验 |
将一式三份的、呈指数生长的细胞接种到厄洛替尼、培美曲塞或以 4:1 恒定浓度比连续稀释的组合中 72 小时。使用细胞计数和 3-(4,5-二甲基噻唑-2-基)-2,5-二苯基四唑溴化物测定来测量细胞活力。与 PBS 处理的对照细胞(被认为 100% 存活)相比,经药物处理的对照细胞存活的百分比称为生长抑制。 CalcuSyn 软件确定 IC50 值,即与未处理的对照细胞相比,药物暴露 72 小时导致细胞生长抑制 50% 的浓度。
为了评估用 B-DIM、厄洛替尼或两者处理的细胞的存活率,将 3,000–5,000 个 BxPC-3 和 MIAPaCa 细胞接种到 96 孔板的每孔中,并在 37°C 下孵育整夜。最初,在一系列浓度下测试 B-DIM (10-50 µM) 和厄洛替尼 (1-5 µM)。根据初步结果为每次检测选择 B-DIM (20 µM) 和厄洛替尼 (2 µM) 的浓度。标准 MTT 测定用于测量 B-DIM (20 µM)、厄洛替尼 (2 µM) 及其组合对 BxPC-3 和 MIAPaCa 细胞的影响。 72小时后进行3次测定。 Tecan 微孔板荧光计测量 595 nm 处的颜色强度。用 DMSO 处理的细胞的值为 100%,并被视为未处理的对照。除了上述测定之外,我们还进行了克隆形成测定来评估治疗效果[2]。 细胞活力测定[2] 为了测试用B-DIM、厄洛替尼或其组合处理的细胞的存活率,将BxPC-3和MIAPaCa细胞(每孔3000-5000个)铺在96孔板中,并在37°C下孵育过夜。我们最初测试了B-DIM(10-50µmol/L)和埃罗替尼(1-5µmol/L)的一系列浓度。根据初步结果,所有测定均选择B-DIM(20µmol/L)和埃罗替尼(2µmol/L)的浓度。72小时后,通过标准3-(4,5-二甲基噻唑-2-基)-2,5-二苯基溴化四唑(MTT)法测定B-DIM(20µmol/L)、埃罗替尼(2µmol/L)和联合用药对BxPC-3和MIAPaCa细胞的影响,并重复三次。通过帝肯微孔板荧光计在595nm下测量颜色强度。DMSO处理的细胞被认为是未处理的对照,并被赋予100%的值。除上述检测外,我们还进行了克隆形成检测,以评估治疗效果,如下所示。 克隆形成试验[2] 为了测试用B-DIM、厄洛替尼或其组合处理的细胞的存活率,将BxPC-3和MIAPaCa细胞(每孔50000-100000)铺在六孔板中,并在37°C下孵育过夜。在暴露于20µmol/L B-DIM、2µmol/L厄洛替尼和组合72小时后,对细胞进行胰蛋白酶处理,计数活细胞(台盼蓝排除),并在100至1000个细胞的100 mm培养皿中平板培养,以确定平板效率并评估处理对克隆存活的影响。然后将细胞在37°C的5%CO2/5%O2/90%N2培养箱中培养约10至12天。菌落用2%结晶紫染色并计数。存活分数在克隆形成效率方面与未经处理的对照细胞标准化,BxPC-3和MIAPaCa细胞的克隆形成效率均为83%。除此试验外,还对细胞进行了类似的处理,将其铺在软琼脂中(软琼脂集落试验),并在37°C下孵育。12天后,还对所有未处理和处理过的孔中的软琼脂菌落进行了计数。 ELISA定量细胞凋亡[2] 细胞死亡检测ELISA试剂盒(罗氏应用科学公司)用于检测未处理和处理的BxPC-3和MIAPaCa细胞的凋亡。接种在六孔板中的细胞用B-DIM(20µmol/L)、厄洛替尼(2µmol/L)或其组合处理。细胞被胰蛋白酶消化,如前所述,使用了约10000个细胞。使用帝肯微孔板荧光计测量405nm处的颜色强度。这个实验重复了三次。 蛋白质提取和蛋白质印迹分析[2] 用B-DIM(20µmol/L)、厄洛替尼(2µmol/L)或联合治疗72小时的BxPC-3和MIAPaCa细胞用于评估治疗对存活素、Bcl-2、Bcl-xL、EGFR、EGFR-pTyr1173、c-IAP1/2、Src、聚ADP核糖聚合酶(PARP)和β-actin表达的影响。实验至少进行了三次。如前所述收获细胞。将样品装载在7%至12%的SDS-PAGE上进行分离,并电泳转移到硝化纤维膜上。每层膜都与抗survivin、Bcl-2、Bcl-xL、Src、c-IAP1/2、EGFR、EGFR-pTyr1173、PARP和β-actin的单克隆抗体一起孵育。印迹与过氧化物酶偶联的二抗一起孵育。然后使用化学发光检测系统测量信号强度。 NF-κB活化的电泳迁移率变化分析[2] 为了评估B-DIM和厄洛替尼对BxPC-3和MIAPaCa细胞的影响,细胞要么未经处理,要么用B-DIM(20µmol/L)、厄洛替宁(2µmol/L)或组合处理,至少重复实验三次,持续72小时。如前所述,使用Dounce均质器在400µL冰冷的裂解缓冲液中均质化细胞或切碎的肿瘤组织。 |
| 动物实验 |
Mice: Erlotinib (5 mg/kg) is administered p.o. or i.p. to Bcrp1/Mdr1a/1b-/- and WT mice. The selection of i.p. administration is predicated on full bioavailability and optimal drug absorption. Three series of samples are taken from the lateral tail vein tip. Whole blood samples are taken during the first series at 15, min, 0.5, 1.5, 5, and 10 h following injection. The sampling times of the two subsequent series are adjusted to 5 and 15 minutes and 0.5, 1.5, 4, and 8 hours after injection based on the findings of this initial group. Blood samples are collected, centrifuged right away, and the plasma is kept at -20°C until high-performance liquid chromatographic analysis is performed.
Rats: There are male Crl:CD (SD) rats (244-297 g) that are seven weeks old. Erlotinib hydrochloride (10 mg/kg and 20 mg/kg) is given orally to the animals by gavage. Mice: The treatment groups consist of seven randomly assigned female ICR-SCID mice, aged 6-7 weeks: (a) control (no treatment); (b) B-DIM (50 mg/kg body weight) administered intragastrically once daily; (c) Erlotinib (50 mg/kg body weight) administered daily intraperitoneally for 15 days; and (d) B-DIM and Erlotinib administered according to the schedule for individual treatments. After receiving their last dose of medication, all mice are killed on day three, and their body weight is recorded. A portion of the tissue is immediately frozen in liquid nitrogen and kept cold (−70°C) for later use, while the remaining portion is fixed in formalin and prepared for paraffin block processing. The presence of a tumor or tumors in each pancreas is verified by staining a fixed tissue section with H&E. Rats: Male Sprague-Dawley (SD) rats six weeks of age, weighing 180–210 g, are utilized. On day 0, SD rats (n=28) receive an intraperitoneal injection of 7 mg/kg of freshly prepared ciprofloxacin (CP) at a concentration of 1 mg/mL. For the purpose of examining Erlotinib's effects, 28 CP-N rats are split into two groups. Animals in two groups (n = 14) are given daily oral gavages of either Erlotinib (20 mg/kg) (CP+E, n = 14) or vehicle (CP+V, n = 14) from day -1 (24 hours before the CP injection) to day 3. Groups treated with vehicles are given the same amount of saline. At six weeks of age, a normal control group (NC, n = 5) consists of five male SD rats. From the first to the third day, the NC rats receive an equivalent volume of saline orally via gavage. Day 4 (96 hours post-CP injection): rats are anesthetized, and following a cardiac puncture, they are sacrificed by exsanguination. The kidneys and blood are simultaneously extracted. Renal tissue is sectioned and fixed in 2% paraformaldehyde/phosphate-buffered saline (PBS) for later use, or it can be snap-frozen in liquid nitrogen. In order to reduce suffering as much as possible, diethyl ether gas anesthesia is used during all surgical procedures. Mice were randomized into the following treatment groups (n = 7): (a) untreated control; (b) only B-DIM (50 mg/kg body weight), intragastric once every day; (c) Erlotinib (50 mg/kg body weight), everyday i.p. for 15 days; and (d) B-DIM and Erlotinib, following schedule as for individual treatments. All mice were killed on day 3 following last dose of treatment, and their body weight was determined. One part of the tissue was rapidly frozen in liquid nitrogen and stored at −70°C for future use and the other part was fixed in formalin and processed for paraffin block. H&E staining of fixed tissue section was used to confirm the presence of tumor(s) in each pancreas. [2] Cisplatin (CP) was freshly prepared in saline at a concentration of 1 mg ml−1 and then injected intraperitoneally in SD rats (n = 28) at a dose of 7 mg/kg on day 0. The dose of CP was selected based on a previous stud. To investigate the effect of Erlotinib, 28 CP-N rats were divided into two groups. Separate groups (n = 14) each of animals were administered with either Erlotinib (20 mg/kg, Cugai Pharmaceutical/F. Hoffmann-La Roche, Basel, Switzerland) (CP+E, n = 14) or vehicle (CP+V, n = 14) daily by oral gavage from day -1 (24 hours prior to the CP injection) to day 3. Vehicle-treated groups received an equivalent volume of saline. Five male SD rats at the age of 6 weeks were used as a normal control group (NC, n = 5). The NC rats were given an equivalent volume of saline daily by oral gavage from day -1 to day 3. At day 4 (96 hours after CP injection), each rat was anesthetized and sacrificed by exsanguination after the cardiac puncture; blood was collected by cardiac puncture and kidneys were collected (Figure 1). Renal tissue was divided; separate portions were snap-frozen in liquid nitrogen or fixed in 2% paraformaldehyde/phosphate-buffered saline (PBS) for later use. All surgery was performed under diethyl ether gas anesthesia, and all efforts were made to minimize suffering. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Erlotinib is about 60% absorbed after oral administration and its bioavailability is substantially increased by food to almost 100%. Peak plasma levels occur 4 hours after dosing. The solubility of erlotinib is pH dependent. Solubility decreases pH increases. Smoking also decrease the exposure of erlotinib. Following a 100 mg oral dose, 91% of the dose was recovered in which 83% was in feces (1% of the dose as unchanged parent compound) and 8% in urine (0.3% of the dose as unchanged parent compound). Apparent volume of distribution = 232 L Smokers have a 24% higher rate of erlotinib clearance. Erlotinib is about 60% absorbed after oral administration and its bioavailability is substantially increased by food to almost 100%. Peak plasma levels occur 4 hours after dosing. The solubility of erlotinib is pH dependent. Erlotinib solubility decreases as pH increases. Following absorption, erlotinib is approximately 93% protein bound to plasma albumin and alpha-1 acid glycoprotein. Erlotinib has an apparent volume of distribution of 232 liters. Time to reach steady state plasma concentration /is/ 7 - 8 days. No significant relationships of clearance to covariates of patient age, body weight or gender were observed. Smokers had a 24% higher rate of erlotinib clearance. Following a 100 mg oral dose, 91% of the dose was recovered: 83% in feces (1% of the dose as intact parent) and 8% in urine (0.3% of the dose as intact parent). For more Absorption, Distribution and Excretion (Complete) data for Erlotinib (10 total), please visit the HSDB record page. Metabolism / Metabolites Metabolism occurs in the liver. In vitro assays of cytochrome P450 metabolism showed that erlotinib is metabolized primarily by CYP3A4 and to a lesser extent by CYP1A2, and the extrahepatic isoform CYP1A1. Metabolism and excretion of erlotinib, an orally active inhibitor of epidermal growth factor receptor tyrosine kinase, were studied in healthy male volunteers after a single oral dose of (14)C-erlotinib hydrochloride (100-mg free base equivalent, approximately 91 microCi/subject)... In plasma, unchanged erlotinib represented the major circulating component, with the pharmacologically active metabolite M14 accounting for approximately 5% of the total circulating radioactivity. Three major biotransformation pathways of erlotinib are O-demethylation of the side chains followed by oxidation to a carboxylic acid, M11 (29.4% of dose); oxidation of the acetylene moiety to a carboxylic acid, M6 (21.0%); and hydroxylation of the aromatic ring to M16 (9.6%). In addition, O-demethylation of M6 to M2, O-demethylation of the side chains to M13 and M14, and conjugation of the oxidative metabolites with glucuronic acid (M3, M8, and M18) and sulfuric acid (M9) play a minor role in the metabolism of erlotinib. The identified metabolites accounted for >90% of the total radioactivity recovered in urine and feces. The metabolites observed in humans were similar to those found in the toxicity species, rats and dogs. Erlotinib has known human metabolites that include Erlotinib M14. Biological Half-Life Median half-life of 36.2 hours. A population pharmacokinetic analysis in 591 patients receiving the single-agent erlotinib hydrochloride 2nd/3rd line regimen showed a median half-life of 36.2 hours. |
| 毒性/毒理 (Toxicokinetics/TK) |
Hepatotoxicity
Elevations in serum aminotransferase levels are common during erlotinib therapy of pancreatic and lung cancers, and values above 5 times the upper limit of normal occur in at least 10% of patients. Similar rates of ALT elevations, however, can occur with comparable antineoplastic regimens. The abnormalities are usually asymptomatic and self-limited, but may require dose adjustment or discontinuation (Case 1). In addition, there have been rare reports of clinically apparent liver injury attributed to erlotinib therapy. The time to onset is typically within days or weeks of starting therapy, and the liver injury can be severe, there being at least a dozen fatal instances reported in the literature. The onset of injury can be abrupt and the pattern of serum enzyme elevations is usually hepatocellular (Case 2). Immunoallergic features (rash, fever and eosinophilia) are not common and autoantibody formation has not been reported. Routine monitoring of liver tests during therapy is recommended. The rate of clinically significant liver injury and hepatic failure is increased in patients with preexisting cirrhosis or hepatic impairment due to liver tumor burden. Likelihood score: B (likely but uncommon cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation No information is available on the clinical use of erlotinib during breastfeeding. Because erlotinib is 93% bound to plasma proteins, the amount in milk is likely to be low. However, its half-life is about 36 hours and it might accumulate in the infant. It is also given in combination with gemcitabine for pancreatic cancer, which may increase the risk to the infant. The manufacturer recommends that breastfeeding be discontinued during erlotinib therapy and for 2 weeks after the final dose. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding 93% protein bound to albumin and alpha-1 acid glycoprotein (AAG) |
| 参考文献 | |
| 其他信息 |
Erlotinib Hydrochloride is the hydrochloride salt of a quinazoline derivative with antineoplastic properties. Competing with adenosine triphosphate, erlotinib reversibly binds to the intracellular catalytic domain of epidermal growth factor receptor (EGFR) tyrosine kinase, thereby reversibly inhibiting EGFR phosphorylation and blocking the signal transduction events and tumorigenic effects associated with EGFR activation.
A quinazoline derivative and ANTINEOPLASTIC AGENT that functions as a PROTEIN KINASE INHIBITOR for EGFR associated tyrosine kinase. It is used in the treatment of NON-SMALL CELL LUNG CANCER. See also: Erlotinib (has active moiety). Drug Indication Non-small cell lung cancer (NSCLC)Tarceva is also indicated for switch maintenance treatment in patients with locally advanced or metastatic non-small cell lung cancer with EGFR activating mutations and stable disease after first-line chemotherapy. Tarceva is also indicated for the treatment of patients with locally advanced or metastatic non-small cell lung cancer after failure of at least one prior chemotherapy regimen. In patients with tumours without EGFR activating mutations, Tarceva is indicated when other treatment options are not considered suitable. When prescribing Tarceva, factors associated with prolonged survival should be taken into account. No survival benefit or other clinically relevant effects of the treatment have been demonstrated in patients with Epidermal Growth Factor Receptor (EGFR)-IHC - negative tumours. Pancreatic cancer Tarceva in combination with gemcitabine is indicated for the treatment of patients with metastatic pancreatic cancer . When prescribing Tarceva, factors associated with prolonged survival should be taken into account. The epidermal growth factor receptor (EGFR) is overexpressed in a significant percentage of carcinomas and contributes to the malignant phenotype. CP-358,774 is a directly acting inhibitor of human EGFR tyrosine kinase with an IC50 of 2 nM and reduces EGFR autophosphorylation in intact tumor cells with an IC50 of 20 nM. This inhibition is selective for EGFR tyrosine kinase relative to other tyrosine kinases we have examined, both in assays of isolated kinases and whole cells. At doses of 100 mg/kg, CP-358,774 completely prevents EGF-induced autophosphorylation of EGFR in human HN5 tumors growing as xenografts in athymic mice and of the hepatic EGFR of the treated mice. CP-358,774 inhibits the proliferation of DiFi human colon tumor cells at submicromolar concentrations in cell culture and blocks cell cycle progression at the G1 phase. This inhibitor produces a marked accumulation of retinoblastoma protein in its underphosphorylated form and accumulation of p27KIP1 in DiFi cells, which may contribute to the cell cycle block. Inhibition of the EGFR also triggers apoptosis in these cells as determined by formation of DNA fragments and other criteria. These results indicate that CP-358,774 has potential for the treatment of tumors that are dependent on the EGFR pathway for proliferation or survival.[1] Purpose: This study was undertaken to select the optimal combination schedule of erlotinib and pemetrexed for the treatment of relapsed non-small cell lung cancer (NSCLC) using a panel of human NSCLC lines. Experimental design: Human NSCLC cell lines, with variable expression of the known molecular determinants of erlotinib sensitivity, were exposed to pemetrexed and erlotinib using different schedules. Antitumor effect was measured by growth inhibition by cell count and 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide assay, cell cycle distribution and apoptosis by flow cytometry, and expression of cell cycle mediators by immunoblots. The cytotoxic interaction between pemetrexed and erlotinib (i.e., synergistic, additive, or antagonistic) was determined by median effect analysis. Results: When cells were exposed to concurrent pemetrexed and erlotinib or sequential pemetrexed followed by erlotinib, cytotoxic synergism was observed in both erlotinib-sensitive and erlotinib-resistant human NSCLC cell lines. This was independent of the mutation status of epidermal growth factor receptor or K-Ras genes. Synergism was associated with a combination of cell cycle effects from both agents. In contrast, exposure of cells to erlotinib followed by pemetrexed was mostly antagonistic in erlotinib-sensitive cells and additive at best in erlotinib-resistant cells. Antagonism was associated with erlotinib-induced G(1)-phase blockade of erlotinib-sensitive cells, which protects cells from pemetrexed cytotoxicity. Pemetrexed induced an epidermal growth factor receptor-mediated activation of the phosphatidylinositol 3-kinase/AKT pathway, which was inhibited by erlotinib and a specific phosphatidylinositol 3-kinase inhibitor, LY294002. Conclusions: The combination of pemetrexed and erlotinib is synergistic in NSCLC in vitro if exposure to erlotinib before pemetrexed is avoided, particularly in tumors that are sensitive to erlotinib. Based on these findings, a randomized phase II study comparing the progression-free survival between an intermittent combination of erlotinib and pemetrexed (experimental arm) and pemetrexed alone (control arm) in patients with relapsing NSCLC has been initiated.[2] Purpose: This study was undertaken to select the optimal combination schedule of erlotinib and pemetrexed for the treatment of relapsed non-small cell lung cancer (NSCLC) using a panel of human NSCLC lines. Experimental design: Human NSCLC cell lines, with variable expression of the known molecular determinants of erlotinib sensitivity, were exposed to pemetrexed and erlotinib using different schedules. Antitumor effect was measured by growth inhibition by cell count and 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide assay, cell cycle distribution and apoptosis by flow cytometry, and expression of cell cycle mediators by immunoblots. The cytotoxic interaction between pemetrexed and erlotinib (i.e., synergistic, additive, or antagonistic) was determined by median effect analysis. Results: When cells were exposed to concurrent pemetrexed and erlotinib or sequential pemetrexed followed by erlotinib, cytotoxic synergism was observed in both erlotinib-sensitive and erlotinib-resistant human NSCLC cell lines. This was independent of the mutation status of epidermal growth factor receptor or K-Ras genes. Synergism was associated with a combination of cell cycle effects from both agents. In contrast, exposure of cells to erlotinib followed by pemetrexed was mostly antagonistic in erlotinib-sensitive cells and additive at best in erlotinib-resistant cells. Antagonism was associated with erlotinib-induced G(1)-phase blockade of erlotinib-sensitive cells, which protects cells from pemetrexed cytotoxicity. Pemetrexed induced an epidermal growth factor receptor-mediated activation of the phosphatidylinositol 3-kinase/AKT pathway, which was inhibited by erlotinib and a specific phosphatidylinositol 3-kinase inhibitor, LY294002. Conclusions: The combination of pemetrexed and erlotinib is synergistic in NSCLC in vitro if exposure to erlotinib before pemetrexed is avoided, particularly in tumors that are sensitive to erlotinib. Based on these findings, a randomized phase II study comparing the progression-free survival between an intermittent combination of erlotinib and pemetrexed (experimental arm) and pemetrexed alone (control arm) in patients with relapsing NSCLC has been initiated.[3] The receptor for epidermal growth factor (EGFR) is overexpressed in many cancers. One important signaling pathway regulated by EGFR is the phosphatidylinositol 3'-kinase (PI3K)-phosphoinositide-dependent kinase 1-Akt pathway. Activation of Akt leads to the stimulation of antiapoptotic pathways, promoting cell survival. Akt also regulates the mammalian target of rapamycin (mTOR)-S6K-S6 pathway to control cell growth in response to growth factors and nutrients. Recent reports have shown that the sensitivity of non-small-cell lung cancer cell lines to EGFR inhibitors such as erlotinib (Tarceva, OSI Pharmaceuticals) is dependent on inhibition of the phosphatidylinositol 3'-kinase-phosphoinositide-dependent kinase 1-Akt-mTOR pathway. There can be multiple inputs to this pathway as activity can be regulated by other receptors or upstream mutations. Therefore, inhibiting EGFR alone may not be sufficient for substantial inhibition of all tumor cells, highlighting the need for multipoint intervention. Herein, we sought to determine if rapamycin, an inhibitor of mTOR, could enhance erlotinib sensitivity for cell lines derived from a variety of tissue types (non-small-cell lung, pancreatic, colon, and breast). Erlotinib could inhibit extracellular signal-regulated kinase, Akt, and S6 only in cell lines that were the most sensitive. Rapamycin could fully inhibit S6 in all cell lines, but this was accompanied by activation of Akt phosphorylation. However, combination with erlotinib could down-modulate rapamycin-stimulated Akt activity. Therefore, in select cell lines, inhibition of both S6 and Akt was achieved only with the combination of erlotinib and rapamycin. This produced a synergistic effect on cell growth inhibition, observations that extended in vivo using xenograft models. These results suggest that combining rapamycin with erlotinib might be clinically useful to enhance response to erlotinib.[4] Our objective was the preclinical assessment of the pharmacokinetics, monotherapy and combined antitumor activity of the epidermal growth factor receptor (HER1/EGFR) tyrosine kinase inhibitor erlotinib in athymic nude mice bearing non-small cell lung cancer (NSCLC) xenograft models. Immunohistochemistry determined the HER1/EGFR status of the NSCLC tumor models. Pharmacokinetic studies assessed plasma drug concentrations of erlotinib in tumor- and non-tumor-bearing athymic nude mice. These were followed by maximum tolerated dose (MTD) studies for erlotinib and each chemotherapy. Erlotinib was then assessed alone and in combination with these chemotherapies in the NSCLC xenograft models. Complete necropsies were performed on most of the animals in each study to further assess antitumor or toxic effects. Erlotinib monotherapy dose-dependently inhibited tumor growth in the H460a tumor model, correlating with circulating levels of drug. There was antitumor activity at the MTD with each agent tested in both the H460a and A549 tumor models (erlotinib 100 mg/kg: 71 and 93% tumor growth inhibition; gemcitabine 120 mg/kg: 93 and 75% tumor growth inhibition; cisplatin 6 mg/kg: 81 and 88% tumor growth inhibition). When each compound was given at a fraction of the MTD, tumor growth inhibition was suboptimal. Combinations of gemcitabine or cisplatin with erlotinib were assessed at 25% of the MTD to determine efficacy. In both NSCLC models, doses of gemcitabine (30 mg/kg) or cisplatin (1.5 mg/kg) with erlotinib (25 mg/kg) at 25% of the MTD were well tolerated. For the slow growing A549 tumor, there was significant tumor growth inhibition in the gemcitabine/erlotinib and cisplatin/erlotinib combinations (above 100 and 98%, respectively), with partial regressions. For the faster growing H460a tumor, there was significant but less remarkable tumor growth inhibition in these same combinations (86 and 53% respectively). These results show that in NSCLC xenograft tumors with similar levels of EGFR expression, the antitumor activity of erlotinib is robust both as monotherapy and in combination with chemotherapies.[5] The receptor for epidermal growth factor (EGFR) is overexpressed in many cancers. One important signaling pathway regulated by EGFR is the phosphatidylinositol 3'-kinase (PI3K)-phosphoinositide-dependent kinase 1-Akt pathway. Activation of Akt leads to the stimulation of antiapoptotic pathways, promoting cell survival. Akt also regulates the mammalian target of rapamycin (mTOR)-S6K-S6 pathway to control cell growth in response to growth factors and nutrients. Recent reports have shown that the sensitivity of non-small-cell lung cancer cell lines to EGFR inhibitors such as erlotinib (Tarceva, OSI Pharmaceuticals) is dependent on inhibition of the phosphatidylinositol 3'-kinase-phosphoinositide-dependent kinase 1-Akt-mTOR pathway. There can be multiple inputs to this pathway as activity can be regulated by other receptors or upstream mutations. Therefore, inhibiting EGFR alone may not be sufficient for substantial inhibition of all tumor cells, highlighting the need for multipoint intervention. Herein, we sought to determine if rapamycin, an inhibitor of mTOR, could enhance erlotinib sensitivity for cell lines derived from a variety of tissue types (non-small-cell lung, pancreatic, colon, and breast). Erlotinib could inhibit extracellular signal-regulated kinase, Akt, and S6 only in cell lines that were the most sensitive. Rapamycin could fully inhibit S6 in all cell lines, but this was accompanied by activation of Akt phosphorylation. However, combination with erlotinib could down-modulate rapamycin-stimulated Akt activity. Therefore, in select cell lines, inhibition of both S6 and Akt was achieved only with the combination of erlotinib and rapamycin. This produced a synergistic effect on cell growth inhibition, observations that extended in vivo using xenograft models. These results suggest that combining rapamycin with erlotinib might be clinically useful to enhance response to erlotinib.[6] Background: Epidermal growth factor receptor (EGFR) and mammalian target of rapamycin (mTOR) are crucial targets in cancer therapy. Combined inhibition of both targets yielded synergistic effects in vitro and in vivo in several cancer entities. However, the impact of EGFR and mTOR expression and combined inhibition in neuroendocrine lung tumors other than small-cell lung cancer remains unclear. Material and methods: Expression and activation of EGFR/AKT/mTOR pathway constituents were investigated in typical and atypical bronchial carcinoid (AC) tumors and large-cell neuroendocrine lung carcinomas (LCNEC) by immunohistochemistry in 110 tumor samples, and correlated with clinicopathological parameters and patient survival. Cytotoxicity of mTOR inhibitor everolimus and EGFR inhibitor erlotinib alone and in combination was assessed using growth inhibition assay in NCI-H720 AC and SHP-77 LCNEC cells. Cell cycle phase distribution was determined by FACS. Apoptosis-associated activation of caspase-3/7 was measured by Caspase-Glo® assay. Activity status of EGFR and mTOR pathway components was analyzed by immunoblotting. Results: Activation of the EGFR/AKT/mTOR axis could be demonstrated in all entities and was significantly increased in higher grade tumors. Neoadjuvant chemotherapy correlated significantly with p-AKT expression and p-ERK loss. Erlotinib combined with everolimus exerted synergistic combination effects in AC and LCNEC cells by induction of apoptosis, while cell cycle phase distribution remained unaffected. These effects could be explained by synergistic downregulation of phospho-mTOR, phospho-p70S6 kinase and phospho-AKT expression by everolimus and erlotinib. Conclusions: Our study indicates that EGFR and mTOR are clinically important targets in bronchial neuroendocrine tumors, and further in vivo and clinical exploration of combined inhibition is warranted.[7] |
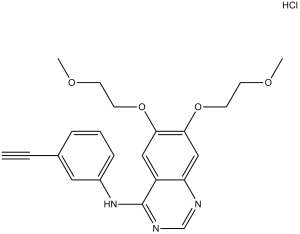
| 分子式 |
C22H23N3O4.HCL
|
|---|---|
| 分子量 |
429.90
|
| 精确质量 |
429.145
|
| 元素分析 |
C, 61.47; H, 5.63; Cl, 8.25; N, 9.77; O, 14.89
|
| CAS号 |
183319-69-9
|
| 相关CAS号 |
Erlotinib-d6 hydrochloride;1189953-78-3;Erlotinib;183321-74-6;Erlotinib mesylate;248594-19-6;Erlotinib-13C6 hydrochloride;1210610-07-3;Erlotinib-d6;1034651-23-4
|
| PubChem CID |
176871
|
| 外观&性状 |
White to off-white solid powder
|
| 沸点 |
553.6ºC at 760 mmHg
|
| 熔点 |
223-225ºC
|
| 闪点 |
288.6ºC
|
| 蒸汽压 |
4.52E-12mmHg at 25°C
|
| LogP |
4.28
|
| tPSA |
74.73
|
| 氢键供体(HBD)数目 |
2
|
| 氢键受体(HBA)数目 |
7
|
| 可旋转键数目(RBC) |
11
|
| 重原子数目 |
30
|
| 分子复杂度/Complexity |
525
|
| 定义原子立体中心数目 |
0
|
| SMILES |
Cl[H].O(C([H])([H])C([H])([H])OC([H])([H])[H])C1C([H])=C2C(=NC([H])=NC2=C([H])C=1OC([H])([H])C([H])([H])OC([H])([H])[H])N([H])C1=C([H])C([H])=C([H])C(C#C[H])=C1[H]
|
| InChi Key |
GTTBEUCJPZQMDZ-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C22H23N3O4.ClH/c1-4-16-6-5-7-17(12-16)25-22-18-13-20(28-10-8-26-2)21(29-11-9-27-3)14-19(18)23-15-24-22;/h1,5-7,12-15H,8-11H2,2-3H3,(H,23,24,25);1H
|
| 化学名 |
N-(3-ethynylphenyl)-6,7-bis(2-methoxyethoxy)quinazolin-4-amine;hydrochloride
|
| 别名 |
NSC718781 HCl; NSC-718781 HCl; CP358774 HCl, NSC 718781 HCl; erlotinib HCl; Tarceva; N-(3-ethynylphenyl)-6,7-bis(2-methoxyethoxy)quinazolin-4-amine hydrochloride; OSI-774; OSI 774; Erlotinib (Hydrochloride); CP-358774 HCl; CP 358774 HCl; OSI-774 HCl; OSI 774 HCl; OSI774 HCl; Erlotinib hydrochloride
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 0.5 mg/mL (1.16 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 5.0 mg/mL澄清DMSO储备液加入400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 0.5 mg/mL (1.16 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 5.0 mg/mL 澄清 DMSO 储备液加入 900 μL 20% SBE-β-CD 生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: 0.5 mg/mL (1.16 mM) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 悬浊液; 超声助溶。 配方 4 中的溶解度: 15% Captisol: 15 mg/mL 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.3261 mL | 11.6306 mL | 23.2612 mL | |
| 5 mM | 0.4652 mL | 2.3261 mL | 4.6522 mL | |
| 10 mM | 0.2326 mL | 1.1631 mL | 2.3261 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
GDC-0449 and Erlotinib Hydrochloride With or Without Gemcitabine Hydrochloride in Treating Patients With Metastatic Pancreatic Cancer or Solid Tumors That Cannot Be Removed by Surgery
CTID: NCT00878163
Phase: Phase 1 Status: Active, not recruiting
Date: 2024-09-19
|
 |
 |