| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| Other Sizes |
|

| 靶点 |
D3 recepto ( Ki = 0.5 nM ); D2L Receptor ( Ki = 2.2 nM ); D2S Receptor ( Ki = 3.9 nM ); D4 receptor ( Ki = 5.1 nM )
|
|---|---|
| 体外研究 (In Vitro) |
- 在人iPSC衍生的多巴胺能神经元中,普拉克索(1 μM)可促进结构可塑性,表现为神经突生长和突触形成增加(通过β-微管蛋白III和突触素I的免疫细胞化学染色评估)。这种作用通过上调BDNF和激活mTOR信号通路介导,western blot分析显示BDNF蛋白水平和磷酸化mTOR升高可证实这一点[3]
- 在中脑培养物中,普拉克索(1 μM)可减轻左旋多巴诱导的毒性。与单独使用左旋多巴相比,它减少活性氧(ROS)生成和caspase-3激活,从而提高细胞活力(通过MTT测定)[4] - 在缺血性中风的体外模型中,普拉克索(10 μM)通过抑制线粒体通透性转换孔(mPTP)开放和维持线粒体膜电位(ΔΨm)防止缺血性细胞死亡。这通过JC-1染色(用于ΔΨm)和western blot分析显示线粒体细胞色素c释放减少得到证实[5] 普拉克索二盐酸盐对D1型受体具有低结合亲和力,IC50 >50,000 nM[1]。 普拉克索二盐酸盐二盐酸盐 (0.01-10 μM;72 小时) 产生剂量增加树突状结构和体细胞大小盐酸普拉克索切断中脑培养物中左旋多巴诱导的毒性,表明盐酸普拉克索可能对组织培养物中的多巴胺神经具有细胞保护作用[4]。 |
| 体内研究 (In Vivo) |
盐酸普拉克索 (0.25-1 mg/kg;ip) 显着减少动物的梗死体积[5]。 盐酸普拉克索改善神经功能恢复[5]。 盐酸普拉克索通过途径达到预防性中风中的艾滋病性细胞死亡[5]。动物模型:雄性Wistar大鼠,体重250-300g(16-18周龄)[5] 剂量:0.25mg/kg、1mg/kg给药方式:腹腔注射,于1小时、6小时、12小时,闭塞后 18 小时结果:与仅进行 tMCAO(短暂性大脑中动脉闭塞)的动物相比,梗塞体积减少。
|
| 酶活实验 |
在大脑中动脉闭塞(MCAO)诱导的大鼠缺血性中风模型中,普拉克索(1 mg/kg,静脉注射)在再灌注后24小时显著减少梗死体积(通过TTC染色评估)并改善神经功能评分。其保护作用与抑制缺血半暗带中线粒体细胞色素c释放和caspase-3激活相关[5]
巴胺受体的结合实验使用表达人D2、D3或D4受体的HEK293细胞膜制剂进行。将膜与[³H]螺哌隆(一种放射性标记配体)和递增浓度的普拉克索共同孵育,进行竞争结合实验。计算平衡解离常数(Ki),结果显示普拉克索对D3受体的亲和力最高,其次是D2和D4受体[1] 普拉克索是一种强效多巴胺受体激动剂,对帕金森病有很高的疗效,其血脑屏障(BBB)转运的主要特征是使用永生化大鼠脑毛细血管内皮细胞(RBEC)1作为体外BBB模型。[(14)C]RBEC1对普拉克索的摄取取决于温度和pH值,但不取决于钠离子浓度或膜电位。包括吡拉明在内的几种有机阳离子抑制了摄取。普拉克索和吡拉明之间存在相互抑制作用。此外,预加载未标记的普拉克索刺激了[(14)C]普拉克索的摄取。对RBEC1中的有机阳离子转运蛋白(rOCT1-3、rOCTN1-2)进行RT-PCR分析。rOCTN2的mRNA水平最高,其次是rOCTN1,而rOCT1、rOCT2和rOCT3的表达可以忽略不计。通过原位大鼠脑灌注技术测量的[(14)C]普拉克索的脑摄取被未标记的普拉克索显著抑制。这些结果表明,普拉克索至少部分是由有机阳离子敏感转运蛋白通过血脑屏障转运的。RBEC1中的普拉克索转运是pH依赖性的,但钠和膜电位无关[2]。 |
| 细胞实验 |
- 分析人iPSC衍生的多巴胺能神经元的结构可塑性:用普拉克索(1 μM)处理细胞24小时。通过抗β-微管蛋白III(神经元标志物)和突触素I(突触标志物)的抗体进行免疫细胞化学染色,评估神经突生长和突触形成。使用western blot测量BDNF和磷酸化mTOR的蛋白水平[3]
- 评估中脑培养物中左旋多巴诱导的毒性:用左旋多巴(100 μM)单独或与普拉克索(1 μM)联合处理培养物48小时。通过MTT测定细胞活力,通过Annexin V-FITC/PI染色结合流式细胞术定量凋亡细胞,检测凋亡情况[4] - 研究缺血细胞模型中的线粒体机制:将细胞暴露于缺血条件并使用普拉克索(10 μM)处理。使用JC-1染色(荧光探针)测量线粒体膜电位(ΔΨm),通过western blot分析线粒体细胞色素c释放[5] 抗帕金森病药物罗匹尼罗和普拉克索是D3受体(D3R-)的多巴胺能(DA)激动剂,用作治疗难治性抑郁症(TRD)的辅助疗法。虽然确切的抗抑郁作用机制尚不清楚,但已有人提出D3R在恢复TRD中受损的神经可塑性中的作用。由于D3R激动剂在人类DA神经元上高度表达,我们使用人类诱导多能干细胞(hiPSCs)的翻译模型研究了罗匹尼罗和普拉克索对结构可塑性的影响。将来自健康供体的两个hiPSC克隆分化为中脑DA神经元。在培养3天后,罗匹宁和普拉克索产生了树突分枝和胞体大小的剂量依赖性增加,这种作用被选择性D3R拮抗剂SB277011-A和S33084以及mTOR途径激酶抑制剂LY294002和雷帕霉素拮抗。所有治疗均能有效减轻D3R依赖性p70S6激酶磷酸化的增加。BDNF的免疫中和、TrkB受体的抑制和MEK-ERK信号传导的阻断同样阻止了罗匹尼罗诱导的结构可塑性,表明BDNF和D3R信号通路之间存在关键的相互作用。从两个hiPSC克隆中获得的DA神经元所获得的数据高度相似,这为它们表征通过多巴胺能机制起作用的药物的可靠性奠定了基础[3]。 |
| 动物实验 |
In rat models of ischemic stroke: Male Sprague-Dawley rats underwent middle cerebral artery occlusion (MCAO) for 2 hours to induce ischemia. pramipexole was administered intravenously at a dose of 1 mg/kg immediately after reperfusion. Neurological function was evaluated using a standard scoring system at 24 hours post-surgery, and infarct volume was measured by TTC staining of brain sections [5]
A dopamine D2 receptor agonist, pramipexole, has been found to elicit neuroprotection in patients with Parkinson's disease and restless leg syndrome. Recent evidence has shown that pramipexole mediates its neuroprotection through mitochondria. Considering this, we examined the possible mitochondrial role of pramipexole in promoting neuroprotection following an ischemic stroke of rat. Male Wistar rats underwent transient middle cerebral artery occlusion (tMCAO) and then received pramipexole (0.25 mg and 1 mg/kg body weight) at 1, 6, 12 and 18 h post-occlusion. A panel of neurological tests and 2,3,5-triphenyl tetrazolium chloride (TTC) staining were performed at 24 h after the surgery. Flow cytometry was used to detect the mitochondrial membrane potential, and mitochondrial levels of reactive oxygen species (ROS) and Ca2+, respectively. Mitochondrial oxidative phosphorylation was analyzed by oxygraph (oxygen electrode). Western blotting was used to analyze the expression of various proteins such as Bax, Bcl-2 and cytochrome c Pramipexole promoted the neurological recovery as shown by the panel of neurobehavioral tests and TTC staining. Post-stroke treatment with pramipexole reduced levels of mitochondrial ROS and Ca2+ after ischemia. Pramipexole elevated the mitochondrial membrane potential and mitochondrial oxidative phosphorylation. Western blotting showed that pramipexole inhibited the transfer of cytochrome c from mitochondria to cytosol, and hence inhibited the mitochondrial permeability transition pore. Thus, our results have demonstrated that post-stroke administration of pramipexole induces the neurological recovery through mitochondrial pathways in ischemia/reperfusion injury[5]. |
| 药代性质 (ADME/PK) |
pramipexole is rapidly absorbed after oral administration, with a time to peak plasma concentration (Tmax) of approximately 6 hours. Oral bioavailability is about 90%, and plasma protein binding is low (<20%). It has an elimination half-life of 8-12 hours and is primarily excreted unchanged in urine [1]
- pramipexole exhibits high blood-brain barrier permeability, with a brain-to-plasma concentration ratio of approximately 0.8. Its transport across the blood-brain barrier is mediated by the organic cation transporter 3 (OCT3) [2] |
| 毒性/毒理 (Toxicokinetics/TK) |
- pramipexole showed low acute toxicity in animal studies, with a median lethal dose (LD50) >2000 mg/kg following oral administration in mice. Repeated dose studies in rats and dogs did not reveal significant hepatic or renal toxicity [1]
- pramipexole has minimal potential for drug-drug interactions due to its low plasma protein binding and limited metabolism by cytochrome P450 enzymes [1] - In mesencephalic cultures, pramipexole (1 μM) reduced levodopa-induced toxicity, as indicated by decreased ROS production, caspase-3 activation, and apoptotic cell death [4] Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation No information is available on the use of pramipexole during breastfeeding, but it suppresses serum prolactin and may interfere with breastfeeding. An alternate drug may be preferred, especially while nursing a newborn or preterm infant. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information in nursing mothers was not found as of the revision date. Pramipexole lowers serum prolactin.[1] The prolactin level in a mother with established lactation may not affect her ability to breastfeed. |
| 参考文献 |
|
| 其他信息 |
- pramipexole is a non-ergoline dopamine agonist that selectively binds to D2, D3, and D4 receptors, with highest affinity for D3 receptors [1]
- The neuroprotective effects of pramipexole in various models (dopaminergic neurons, ischemic stroke) are linked to multiple mechanisms, including activation of BDNF/mTOR signaling (structural plasticity) and inhibition of mitochondrial dysfunction (reduced mPTP opening, cytochrome c release) [3,5] - pramipexole is clinically used for treating Parkinson's disease, leveraging its dopamine receptor agonist activity to modulate dopaminergic neurotransmission [1] Pramipexole hydrochloride anhydrous is a hydrochloride that is the anhydrous dihydrochloride salt of pramipexole. It has a role as a dopamine agonist and an antiparkinson drug. It contains a pramipexole(2+). Pramipexole Dihydrochloride is the hydrochloride salt of pramipexole, a benzothiazole derivative. As a nonergot dopamine agonist, pramipexole binds to D2 and D3 dopamine receptors in the striatum and substantia nigra of the brain. Compared to other dopamine agonists, the use of this agent may be associated with fewer dyskinetic side effects in treated subjects. (NCI04) A benzothiazole derivative and dopamine agonist with antioxidant properties that is used in the treatment of PARKINSON DISEASE and RESTLESS LEGS SYNDROME. See also: Pramipexole (has active moiety). Drug Indication Sifrol is indicated for treatment of the signs and symptoms of idiopathic Parkinson's disease, alone (without levodopa) or in combination with levodopa, i. e. over the course of the disease, though to late stages when the effect of levodopa wears off or becomes inconsistent and fluctuations of the therapeutic effect occur (end-of-dose or 'on-off' fluctuations). Sifrol is indicated for symptomatic treatment of moderate to severe idiopathic restless-legs syndrome in dosages up to 0. 54 mg of base (0. 75 mg of salt). |
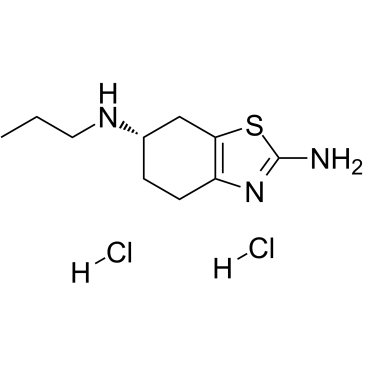
| 分子式 |
C10H19CL2N3S
|
|---|---|
| 分子量 |
284.25
|
| 精确质量 |
283.067
|
| 元素分析 |
C, 42.25; H, 6.74; Cl, 24.95; N, 14.78; S, 11.28
|
| CAS号 |
104632-25-9
|
| 相关CAS号 |
Dexpramipexole dihydrochloride; 104632-27-1; Pramipexole; 104632-26-0; Pramipexole dihydrochloride hydrate; 191217-81-9; Dexpramipexole; 104632-28-2; Pramipexole-d7 dihydrochloride; Pramipexole-d5 dihydrochloride; 1217601-58-5; Pramipexole-d7-1 dihydrochloride; 2702798-58-9
|
| PubChem CID |
119569
|
| 外观&性状 |
White to off-white solid powder
|
| 沸点 |
378ºC at 760 mmHg
|
| 熔点 |
288-290ºC
|
| 闪点 |
182.4ºC
|
| 蒸汽压 |
6.49E-06mmHg at 25°C
|
| LogP |
4.158
|
| tPSA |
79.18
|
| 氢键供体(HBD)数目 |
4
|
| 氢键受体(HBA)数目 |
4
|
| 可旋转键数目(RBC) |
3
|
| 重原子数目 |
16
|
| 分子复杂度/Complexity |
188
|
| 定义原子立体中心数目 |
1
|
| SMILES |
Cl[H].Cl[H].S1C(N([H])[H])=NC2=C1C([H])([H])[C@]([H])(C([H])([H])C2([H])[H])N([H])C([H])([H])C([H])([H])C([H])([H])[H]
|
| InChi Key |
QMNWXHSYPXQFSK-KLXURFKVSA-N
|
| InChi Code |
InChI=1S/C10H17N3S.2ClH/c1-2-5-12-7-3-4-8-9(6-7)14-10(11)13-8;;/h7,12H,2-6H2,1H3,(H2,11,13);2*1H/t7-;;/m0../s1
|
| 化学名 |
(6S)-6-N-propyl-4,5,6,7-tetrahydro-1,3-benzothiazole-2,6-diamine;dihydrochloride
|
| 别名 |
Pramipexole 2HCl; Pramipexole Dihydrochloride; Mirapex ER; Pramipexole hydrochloride; Pramipexole dihydrochloride; 104632-25-9; (S)-N6-Propyl-4,5,6,7-tetrahydrobenzo[d]thiazole-2,6-diamine dihydrochloride; Mirapex ER; PRAMIPEXOLE HYDROCHLORIDE; (S)-Pramipexole Dihydrochloride; PRAMIPEXOLE HCl; Pramipexole (dihydrochloride); SND919; Mirapex; SUD 919CL2Y; SUD919CL2Y; U-98528E; Sifrol; SND 919; KNS-760704
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO: ~56 mg/mL (~197.0 mM)
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: 100 mg/mL (351.80 mM) in PBS (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶。
请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 3.5180 mL | 17.5901 mL | 35.1803 mL | |
| 5 mM | 0.7036 mL | 3.5180 mL | 7.0361 mL | |
| 10 mM | 0.3518 mL | 1.7590 mL | 3.5180 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。