| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| 5g |
|
||
| Other Sizes |
|
| 靶点 |
α-adrenergic receptor
α1-adrenergic receptor (Ki = 0.6 nM for α1A, 0.8 nM for α1B, 0.7 nM for α1D subtypes) [2] - α1-adrenergic receptor (IC50 = 1.1 μM for inhibiting prostate smooth muscle contraction) [4] |
|---|---|
| 体外研究 (In Vitro) |
Terazosin 在 PC-3 和人良性前列腺细胞中诱导细胞毒性,IC50 超过 100 μM。 Terazosin 还有效抑制血管内皮生长因子诱导的人脐静脉内皮细胞增殖和管形成(IC50 分别为 9.9 和 6.8 μM)。细胞测定:为了确定细胞毒性作用的作用模式,本研究中使用了多种鉴定技术。使用末端脱氧核苷酸转移酶脱氧尿苷三磷酸缺口末端标记原位检测凋亡细胞。结果显示,用特拉唑嗪 (100 μM) 处理 PC-3 细胞 12 小时后出现阳性反应。
人前列腺癌细胞(LNCaP、DU145)经Terazosin HCl dihydrate(10-100 μM)处理72小时后,呈剂量依赖性抑制细胞增殖。MTT法检测显示,100 μM浓度下LNCaP细胞活力降低65%,DU145细胞降低58%;流式细胞术检测显示,80 μM时LNCaP细胞凋亡率达32%,DU145细胞达28%[1] - 克隆形成实验显示,Terazosin HCl dihydrate(20 μM)处理后,LNCaP细胞克隆形成率较对照组降低40%。Western blot分析显示,Bax和切割型caspase-3蛋白表达上调,Bcl-2蛋白表达下调[1] - 大鼠前列腺平滑肌细胞与Terazosin HCl dihydrate(1-50 μM)孵育后,呈剂量依赖性抑制去氧肾上腺素诱导的收缩,IC50为1.1 μM,50 μM时抑制率达最大值(75%)[4] - 在人膀胱平滑肌细胞中,Terazosin HCl dihydrate(30 μM)通过阻断α1-肾上腺素受体,减少去甲肾上腺素诱导的钙内流达55%[2] |
| 体内研究 (In Vivo) |
特拉唑嗪对运动活动和僵直症产生剂量依赖性的完全抑制作用。脑室内注射该拮抗剂可保护纹状体和大脑皮质 α1 受体,但不能保护纹状体或皮质 D1 受体免受 N-乙氧基羰基-2-乙氧基-1,2-二羟基喹啉体内烷基化。心室内注射特拉唑嗪还会导致体温过低和呼吸频率降低,表明交感神经流出减少。特拉唑嗪不会损害水平钢丝测试的表现或游泳测试中协调运动的能力。 Terazosin 在裸鼠中显着抑制血管内皮生长因子诱导的血管生成,IC50 为 7.9 μM,表明其具有比细胞毒作用更有效的抗血管生成作用。
良性前列腺增生(BPH)模型大鼠口服Terazosin HCl dihydrate(5 mg/kg/天)4周后,前列腺重量减轻22%,尿流率提高30%(通过膀胱测压法检测)[4] - 接种LNCaP前列腺癌异种移植瘤的裸鼠,口服Terazosin HCl dihydrate(40 mg/kg/天)28天后,肿瘤体积较溶媒组缩小45%,肿瘤重量减轻42%。免疫组织化学检测显示,增殖标志物Ki-67表达降低,TUNEL阳性(凋亡)细胞增多[3] - 正常血压大鼠静脉注射Terazosin HCl dihydrate(2 mg/kg)后30分钟内,收缩压降低25 mmHg,效应持续4小时,由外周α1-肾上腺素受体拮抗介导[2] - BPH大鼠长期口服Terazosin HCl dihydrate(10 mg/kg/天)后,膀胱出口阻力恢复正常,残余尿量减少40%[4] |
| 酶活实验 |
α1-肾上腺素受体结合实验:制备人前列腺组织或表达重组α1A/α1B/α1D受体的细胞膜组分,将Terazosin HCl dihydrate(0.01-100 nM)与细胞膜及[³H]哌唑嗪(α1配体)在25°C孵育60分钟。过滤去除未结合配体,定量结合放射性强度,采用Scatchard分析法计算Ki值[2]
- 前列腺平滑肌收缩实验:将离体大鼠前列腺条置于含氧的克-林溶液器官浴中,在存在或不存在Terazosin HCl dihydrate(0.1-10 μM)的条件下,用去氧肾上腺素(1 μM)刺激。记录收缩张力,通过剂量-反应曲线推导IC50值[4] |
| 细胞实验 |
本研究采用多种鉴定技术来确定细胞毒性作用的作用方式。使用末端脱氧核苷酸转移酶脱氧尿苷三磷酸缺口末端标记可以原位检测凋亡细胞。数据表明,用 100 μM 特拉唑嗪处理 12 小时的 PC-3 细胞显示出阳性反应。
本研究中使用了PC-3细胞和人良性前列腺细胞的原代培养物。使用3-(4,5-二甲基噻唑-2-基)-2,5-二苯基溴化四氮唑测定法和乳酸脱氢酶释放反应检测细胞毒性作用。在裸鼠模型中测定体内血管生成作用,然后进行组织学检查和血红蛋白检测定量。在培养的人脐静脉内皮细胞中进行了细胞迁移、增殖和管形成的体外测定。结果terazosin/特拉唑嗪可诱导PC-3和人类良性前列腺细胞产生细胞毒性,IC50超过100微M。末端脱氧核苷酸转移酶脱氧尿苷三磷酸缺口末端标记和乳酸脱氢酶释放反应阳性与特拉唑嗪诱导的细胞毒性有关,表明细胞凋亡和坏死死亡。此外,特拉唑嗪作用引起的细胞毒性不是喹唑啉基结构的常见特征。特拉唑嗪显著抑制血管内皮生长因子诱导的裸鼠血管生成,IC50为7.9微M。,表明其抗血管生成作用比细胞毒性作用更强。特拉唑嗪还有效地抑制了血管内皮生长因子诱导的培养的人脐静脉内皮细胞的增殖和管形成(IC50分别为9.9和6.8微摩尔)。 结论:我们的数据表明,terazosin/特拉唑嗪通过抑制内皮细胞的增殖和管形成显示出直接的抗血管生成活性。这一作用可能部分解释了特拉唑嗪的体内抗肿瘤潜力[4]。 前列腺癌细胞增殖与凋亡实验:LNCaP和DU145细胞以5×10³个/孔接种于96孔板,培养24小时后用Terazosin HCl dihydrate(10-100 μM)处理72小时。MTT法检测细胞活力;Annexin V-FITC/PI染色后流式细胞术检测凋亡率;Western blot检测Bax、Bcl-2和切割型caspase-3蛋白表达[1] - 膀胱平滑肌钙内流实验:人膀胱平滑肌细胞接种于24孔板,负载钙敏感荧光染料。用Terazosin HCl dihydrate(10-50 μM)预处理细胞30分钟后,用去甲肾上腺素(1 μM)刺激,通过检测荧光强度定量钙内流[2] - 克隆形成实验:LNCaP细胞以1×10³个/孔接种于6孔板,用Terazosin HCl dihydrate(10-40 μM)处理24小时,每3天更换一次培养基。14天后结晶紫染色并计数克隆,计算克隆形成率=(处理组克隆数/对照组克隆数)×100%[3] |
| 动物实验 |
Dissolved in water; 0.05 mg/kg; oral gavage
Mice terazosin, a water-soluble alpha 1 antagonist that can be administered in high doses intraventricularly was used to study the relationship between brain alpha 1 adrenoceptor neurotransmission and behavioral activation in the mouse. The antagonist was found to produce a dose-dependent, complete inhibition of motor activity and catalepsy which were reversed preferentially by coinfusion of an alpha 1 agonist (phenylephrine) compared to a D1 (SKF38393) or a D2 agonist, (quinpirole). Blockade of central beta-1 (betaxolol), alpha-2 (RX821002) or beta-2 (ICI 118551) adrenoceptors had smaller or non-significant effects. Terazosin's selectivity for alpha 1 receptors versus dopaminergic receptors was verified under the present conditions by showing that the intraventricularly administered antagonist protected striatal and cerebral cortical alpha 1 receptors but not striatal or cortical D1 receptors from in vivo alkylation by N-ethoxycarbonyl-2-ethoxy-1, 2-dihydroxyquinoline. That its effect was due to blockade of brain rather than peripheral receptors was shown by the finding that intraperitoneal doses of terazosin three to 66 times greater than the maximal intraventricular dose produced less behavioral inhibition. Intraventricular terazosin also produced hypothermia and a reduced respiratory rate suggestive of a reduced sympathetic outflow. However, external heat did not affect the inactivity, and captopril, a hypotensive agent, did not mimic it. Terazosin did not impair performance on a horizontal wire test or the ability to make co-ordinated movements in a swim test suggesting that its activity-reducing effect was not due to sedation and may have a motivational or sensory gating component. It is concluded that central alpha 1-noradrenergic neurotransmission is required for behavioral activation to environmental change in the mouse and may operate on sensorimotor and motivational processes. Neuroscience. 1999;94(4):1245-52. BPH model rats (male Wistar, 12 weeks old) were induced by testosterone propionate injection. After 4 weeks of model establishment, rats were treated with Terazosin HCl dihydrate (5 mg/kg/day) dissolved in distilled water via oral gavage for 4 weeks. Prostate weight, urinary flow rate, and residual urine volume were measured at sacrifice [4] - Nude mice (BALB/c-nu) were subcutaneously inoculated with LNCaP cells (1×10⁶ cells/mouse). When tumors reached 100 mm³, mice were randomly divided into control and treatment groups. Terazosin HCl dihydrate was administered orally at 40 mg/kg/day for 28 days. Tumor volume was measured every 4 days, and mice were sacrificed to weigh tumors and collect samples for immunohistochemistry [3] - Normotensive Sprague-Dawley rats (male, 10 weeks old) received intravenous injection of Terazosin HCl dihydrate (2 mg/kg) dissolved in 0.9% saline. Systolic blood pressure was measured at 15-minute intervals for 6 hours using a tail-cuff system [2] |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Approximately 90%. Approximately 10% of the oral dose is excreted unchanged in the urine and approximately 20% is excreted in the feces. 40% of the total dose is eliminated in urine and 60% of the total dose is eliminated in the feces. 25L to 30L. Plasma clearance is 80mL/min and renal clearance is 10mL/min. Metabolism / Metabolites The majority of terazosin is hepatically metabolized. The metabolites recovered include 6-O-demethyl terazosin, 7-O-methyl terazosin, a piperozine derivative, and a diamine derivative. Hepatic. One of the four metabolites identified (piperazine derivative of terazosin) has antihypertensive activity. Route of Elimination: Approximately 10% of an orally administered dose is excreted as parent drug in the urine and approximately 20% is excreted in the feces. Half Life: 12 hours Biological Half-Life Terazosin has a mean half life 12 hours though this can be as high as 14 hours in patients over 70 years and as low as 11.4 hours in patients 20 to 39 years old. After oral administration of Terazosin HCl dihydrate (5 mg) to healthy volunteers, peak plasma concentration (Cmax) of 28 ng/mL was achieved at 1 hour, with oral bioavailability of 70% [4] - The elimination half-life (t1/2) of Terazosin HCl dihydrate in humans is 12 hours, and 60% of the administered dose is excreted in urine within 24 hours (30% as unchanged drug, 30% as metabolites) [4] - In rats, oral administration of Terazosin HCl dihydrate (10 mg/kg) showed Cmax of 156 ng/mL at 1.5 hours, with wide tissue distribution (highest concentrations in prostate and vascular smooth muscle) [2] |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
Terazosin selectively and competitively inhibits vascular postsynaptic alpha(1)-adrenergic receptors, resulting in peripheral vasodilation and a reduction of vascular resistance and blood pressure. Unlike the nonselective alph-adrenergic blockers phenoxybenzamine and phentolamine, terazosin does not block presynaptic alpha(2)-receptors and, hence, does not cause reflex activation of norepinephrine release to produce reflex tachycardia. Hepatotoxicity Terazosin has been associated with a low rate of serum aminotransferase elevations that in controlled trials was no higher than with placebo therapy. These elevations were transient and did not require dose modification. Instances of serum enzyme elevations, but no instances of clinically apparent acute liver injury with jaundice due to terazosin, have been published. Furthermore, product labels do not include discussion of hepatic toxicity. Cholestatic hepatitis and jaundice have been reported with other alpha-adrenergic blockers. Thus, acute symptomatic liver injury due to terazosin must be exceedingly rare if it occurs at all. Likelihood score: E (unlikely cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Because no information is available on the use of terazosin during breastfeeding, an alternate drug may be preferred, especially while nursing a newborn or preterm infant. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information in nursing mothers was not found as of the revision date. However, the pharmacologically similar drug prazosin does not affect serum prolactin concentration in patients with hypertension. The prolactin level in a mother with established lactation may not affect her ability to breastfeed. Protein Binding 90-94%. In clinical studies for BPH, Terazosin HCl dihydrate (1-10 mg/day, po) was well-tolerated, with mild adverse events including dizziness (11%), postural hypotension (8%), and headache (5%); no severe liver or kidney toxicity was reported [4] - Plasma protein binding of Terazosin HCl dihydrate is 90% in human plasma and 88% in rat plasma [2] - Acute oral LD50 of Terazosin HCl dihydrate in mice is 1200 mg/kg [3] - No significant drug-drug interactions were observed when co-administered with nonsteroidal anti-inflammatory drugs (NSAIDs) or antihypertensive agents [4] |
| 参考文献 | |
| 其他信息 |
Recent evidence from our laboratory has demonstrated that alpha1-adrenoceptor antagonists doxazosin and terazosin induced apoptosis in prostate epithelial and smooth muscle cells in patients with benign prostatic hypertrophy (BPH; J. Urol., 159: 1810-1815, 1998; J. Urol., 161: 2002-2007, 1999). In this study, we investigated the biological action of three alpha1-adrenoceptor antagonists, doxazosin, terazosin, and tamsulosin, against prostate cancer cell growth. The antigrowth effect of the three alpha1-adrenoceptor antagonists was examined in two human prostate cancer cell lines, PC-3 and DU-145, and a prostate smooth muscle cell primary culture, SMC-1, on the basis of: (a) cell viability assay; (b) rate of DNA synthesis; and (c) induction of apoptosis. Our results indicate that treatment of prostate cancer cells with doxazosin or terazosin results in a significant loss of cell viability, via induction of apoptosis in a dose-dependent manner, whereas tamsulosin had no effect on prostate cell growth. Neither doxazosin nor terazosin exerted a significant effect on the rate of cell proliferation in prostate cancer cells. Exposure to phenoxybenzamine, an irreversible inhibitor of alpha1-adrenoceptors, does not abrogate the apoptotic effect of doxazosin or terazosin against human prostate cancer or smooth muscle cells. This suggests that the apoptotic activity of doxazosin and terazosin against prostate cells is independent of their capacity to antagonize alpha1-adrenoceptors. Furthermore, an in vivo efficacy trial demonstrated that doxazosin administration (at tolerated pharmacologically relevant doses) in SCID mice bearing PC-3 prostate cancer xenografts resulted in a significant inhibition of tumor growth. These findings demonstrate the ability of doxazosin and terazosin (but not tamsulosin) to suppress prostate cancer cell growth in vitro and in vivo by inducing apoptosis without affecting cell proliferation. This evidence provides the rationale for targeting both drugs, already in clinical use and with established adverse-effect profiles, against prostatic tumors for the treatment of advanced prostate cancer.[2]
Human ether-a-go-go-related gene (HERG) potassium channels are expressed in multiple tissues including the heart and adenocarcinomas. In cardiomyocytes, HERG encodes the alpha-subunit underlying the rapid component of the delayed rectifier potassium current, I(Kr), and pharmacological reduction of HERG currents may cause acquired long QT syndrome. In addition, HERG currents have been shown to be involved in the regulation of cell proliferation and apoptosis. Selective alpha 1-adrenoceptor antagonists are commonly used in the treatment of hypertension and benign prostatic hyperplasia. Recently, doxazosin has been associated with an increased risk of heart failure. Moreover, quinazoline-derived alpha 1-inhibitors induce apoptosis in cardiomyocytes and prostate tumor cells independently of alpha1-adrenoceptor blockade. To assess the action of the effects of prazosin, doxazosin, and terazosin on HERG currents, we investigated their acute electrophysiological effects on cloned HERG potassium channels heterologously expressed in Xenopus oocytes and HEK 293 cells.Prazosin, doxazosin, and terazosin blocked HERG currents in Xenopus oocytes with IC(50) values of 10.1, 18.2, and 113.2 microM respectively, whereas the IC(50) values for HERG channel inhibition in human HEK 293 cells were 1.57 microM, 585.1 nM, and 17.7 microM. Detailed biophysical studies revealed that inhibition by the prototype alpha 1-blocker prazosin occurred in closed, open, and inactivated channels. Analysis of the voltage-dependence of block displayed a reduction of inhibition at positive membrane potentials. Frequency-dependence was not observed. Prazosin caused a negative shift in the voltage-dependence of both activation (-3.8 mV) and inactivation (-9.4 mV). The S6 mutations Y652A and F656A partially attenuated (Y652A) or abolished (F656A) HERG current blockade, indicating that prazosin binds to a common drug receptor within the pore-S6 region. In conclusion, this study demonstrates that HERG potassium channels are blocked by prazosin, doxazosin, and terazosin. These data may provide a hypothetical molecular explanation for the apoptotic effect of quinazoline-derived alpha1-adrenoceptor antagonists.[3] Metastatic prostate cancer progresses from androgen-dependent to androgen-independent. Terazosin, a long-acting selective alpha1-adrenoreceptor antagonist, induces apoptosis of prostate cancer cells in an alpha1-adrenoreceptor-independent manner, while genistein, a major soy isoflavone, inhibits the growth of several types of cancer cells. The present study was designed to test the therapeutic potential of a combination of terazosin and genistein using a metastatic, hormone-independent prostatic cancer cell line, DU-145. Terazosin or genistein treatment inhibited the growth of DU-145 cells in a dose-dependent manner, whereas had no effect on normal prostate epithelial cells. Addition of 1 microg/ml of terazosin, which was inactive alone, augmented the growth inhibitory effect of 5 microg/ml of genistein. Co-treatment with terazosin resulted in the genistein-induced arrest of DU-145 cells in G2/M phase being overridden and an increase in apoptotic cells, as evidenced by procaspase-3 activation and PARP cleavage. The combination also caused a greater decrease in the levels of the apoptosis-regulating protein, Bcl-XL, and of VEGF165 and VEGF121 than genistein alone. In conclusion, the terazosin/genistein combination was more effective in inhibiting cell growth and VEGF expression as well as inducing apoptosis of the metastatic, androgen-independent prostate cancer cell line, DU-145, than either alone. The doses used in this study are in lower and nontoxic anticancer dosage range, suggesting this combination has potential for therapeutic use.[4] Terazosin HCl dihydrate is a selective α1-adrenergic receptor antagonist with high affinity for all α1 subtypes (α1A, α1B, α1D) [2] - Clinically, it is approved for the treatment of benign prostatic hyperplasia (BPH) and hypertension, exerting effects via relaxing prostate/bladder neck smooth muscle and peripheral vascular smooth muscle [4] - Beyond its approved indications, Terazosin HCl dihydrate exhibits potential anti-tumor activity against prostate cancer by inducing apoptosis and inhibiting cell proliferation [1,3] - The drug’s long elimination half-life allows once-daily oral administration, improving patient compliance for chronic conditions like BPH [4] |
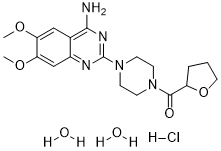
| 分子式 |
C19H30CLN5O6
|
|
|---|---|---|
| 分子量 |
459.92
|
|
| 精确质量 |
459.188
|
|
| 元素分析 |
C, 49.62; H, 6.57; Cl, 7.71; N, 15.23; O, 20.87
|
|
| CAS号 |
70024-40-7
|
|
| 相关CAS号 |
(R)-Terazosin; 109351-34-0; (S)-Terazosin; 109351-33-9; Terazosin; 63590-64-7; Terazosin hydrochloride; 63074-08-8
|
|
| PubChem CID |
63016
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| 沸点 |
664.5ºC at 760 mmHg
|
|
| 熔点 |
215 - 217ºC
|
|
| LogP |
2.314
|
|
| tPSA |
121.5
|
|
| 氢键供体(HBD)数目 |
4
|
|
| 氢键受体(HBA)数目 |
10
|
|
| 可旋转键数目(RBC) |
4
|
|
| 重原子数目 |
31
|
|
| 分子复杂度/Complexity |
544
|
|
| 定义原子立体中心数目 |
0
|
|
| SMILES |
Cl[H].O1C([H])([H])C([H])([H])C([H])([H])C1([H])C(N1C([H])([H])C([H])([H])N(C2N=C(C3=C([H])C(=C(C([H])=C3N=2)OC([H])([H])[H])OC([H])([H])[H])N([H])[H])C([H])([H])C1([H])[H])=O.O([H])[H].O([H])[H]
|
|
| InChi Key |
NZMOFYDMGFQZLS-UHFFFAOYSA-N
|
|
| InChi Code |
InChI=1S/C19H25N5O4.ClH.2H2O/c1-26-15-10-12-13(11-16(15)27-2)21-19(22-17(12)20)24-7-5-23(6-8-24)18(25)14-4-3-9-28-14;;;/h10-11,14H,3-9H2,1-2H3,(H2,20,21,22);1H;2*1H2
|
|
| 化学名 |
[4-(4-amino-6,7-dimethoxyquinazolin-2-yl)piperazin-1-yl]-(oxolan-2-yl)methanone;dihydrate;hydrochloride
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (5.44 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (5.44 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (5.44 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 配方 4 中的溶解度: 4.55 mg/mL (9.89 mM) in PBS (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶 (<60°C). 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.1743 mL | 10.8715 mL | 21.7429 mL | |
| 5 mM | 0.4349 mL | 2.1743 mL | 4.3486 mL | |
| 10 mM | 0.2174 mL | 1.0871 mL | 2.1743 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT04551040 | Active Recruiting |
Drug: Terazosin | Healthy | University of Iowa | March 26, 2021 | Phase 1 |
| NCT04760860 | Not yet recruiting | Drug: Terazosin Hydrochloride Other: Placebo |
Dementia With Lewy Bodies | Qiang Zhang | October 2024 | Phase 1 Phase 2 |
| NCT04386317 | Recruiting | Drug: Terazosin | REM Sleep Behavior Disorder Pre-motor Parkinson's Disease |
Cedars-Sinai Medical Center | November 1, 2020 | Phase 2 |
| NCT05109364 | Recruiting | Drug: Terazosin therapy | REM Sleep Behavior Disorder Pre-motor Parkinson's Disease |
Cedars-Sinai Medical Center | September 23, 2022 | Phase 2 |
| NCT05855577 | Not yet recruiting | Drug: Terazosin | Parkinson Disease Gait Analysis Metabolic Disease |
I.R.C.C.S. Fondazione Santa Lucia |
December 2023 | Phase 4 |
 Representative traces of urethral (a) and abdominal (b) pressure changes induced by duloxetine (1 mg/kg iv) in the presence of intrathecal (it) methiothepin maleate (A), terazosin (B), coapplication of methiothepin maleate and terazosin (C), and coapplication.Am J Physiol Renal Physiol. 2008 Jul; 295(1): F264–F271. Representative traces of urethral (a) and abdominal (b) pressure changes induced by duloxetine (1 mg/kg iv) in the presence of intrathecal (it) methiothepin maleate (A), terazosin (B), coapplication of methiothepin maleate and terazosin (C), and coapplication.Am J Physiol Renal Physiol. 2008 Jul; 295(1): F264–F271. |
|---|
 |
  |