| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 100mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| 5g |
|
||
| 10g |
|
||
| Other Sizes |
|
| 靶点 |
CYP3A4; CYP24A1
|
||
|---|---|---|---|
| 体外研究 (In Vitro) |
当男性接受持续性真菌感染治疗时,酮康唑 (R-41400)(一种咪唑抗真菌药物)经常会导致雄激素缺乏的症状,例如性欲下降、男性乳房发育症、阳痿、少精症和睾酮水平降低[1]。此外,酮康唑 (R-41400) 抑制细胞色素 P450[2]。酮康唑 (R-41400),通过寄生虫学、组织学和生化特征来评估这些喹啉类药物对曼氏血吸虫感染的抗血吸虫能力。将小鼠分为七组:未治疗组 (I)、未感染组 (II)、感染组 (III)、用 PZQ (1,000 mg/kg)、QN (400 mg/kg)、KTZ (10 mg/kg) 治疗组 (IV) )+QN作为IV组(V),HF(400mg/kg)(VI),和KTZ(作为V组)+HF(作为VI组)(VII)。与单独使用 QN 或 HF 治疗的患者相比,KTZ + QN 或 HF 对肝脏 CYP450(85.7% 和 83.8%)和 CYT b5(75.5% 和 73.5%)活性产生更大的抑制(P<0.05)。雌性数量(89.0% 和 79.3%)、蠕虫总数(81.4% 和 70.3%)和卵负载(肝脏;83.8%、66.0%,肠道;68%、64.5%)分别下降更多。还结合此进行了观察[3]。 CYP24A1 抑制剂会促进不依赖 caspase 的细胞凋亡途径的激活,增加全身骨化三醇的暴露,并增强抗增殖作用。此外,酮康唑是外泌体形成和/或分泌的强抑制剂[4]。
|
||
| 体内研究 (In Vivo) |
酮康唑(25 mg/kg,腹腔注射)显着降低血浆皮质酮并减少低剂量可卡因自我给药,而不影响大鼠的食物强化反应。酮康唑将大鼠口服地高辛的 AUC 从 63 mg xh/L 提高至 411 mg xh/L。在大鼠中,酮康唑将静脉注射地高辛的 AUC 从 93 mg × h/L 提高至 486 mg × h/L。酮康唑将大鼠体内地高辛的生物利用度从 0.68 增加至 0.84,同时平均吸收时间从 1.1 小时缩短至 0.3 小时。
|
||
| 酶活实验 |
酮康唑是一种咪唑类抗真菌药物,在接受慢性真菌感染治疗的男性中,通常会产生雄激素缺乏的特征,包括性欲下降、男性乳房发育症、阳痿、少精症和睾酮水平降低。基于这些对体内性腺功能的强效作用以及之前的体外研究,证明酮康唑对糖皮质激素受体蛋白、1,25(OH)2维生素D3和性类固醇结合球蛋白(SSBG)的亲和力,还研究了酮康唑与人雄激素受体(AR)的体外结合。在22摄氏度下测定了酮康唑与[3H]甲基三烯酮(R1881)在分散、完整培养的人皮肤成纤维细胞中雄激素结合位点的竞争。6.4+/-1.8(SE)x 10(-5)M酮康唑实现了[3H]R1881与AR结合的50%置换。在[3H]R1881含量增加的情况下,对酮康唑进行的其他结合研究表明,当采用Scatchard方法分析数据时,酮康唑与AR的相互作用是竞争性的。然而,应该指出的是,至少在血浆中,体内不太可能达到雄激素受体50%占有率所需的酮康唑剂量。最后,对其他咪唑类药物(如克霉唑、咪康唑和氟康唑)进行的雄激素结合研究表明,在这类化合物中,似乎只有酮康唑与雄激素受体相互作用。酮康唑似乎是第一个与SSBG和多种类固醇激素受体竞争性结合的非甾体化合物,这表明这些蛋白质的配体结合位点具有一些共同特征[2]。
|
||
| 细胞实验 |
高全身暴露于骨化三醇是获得最佳抗肿瘤效果所必需的。人癌症PC3细胞对骨化三醇治疗不敏感。因此,我们研究了酮康唑(KTZ)或RC2204对主要骨化三醇失活酶24-羟化酶(CYP24A1)的抑制是否调节骨化三醇的血清药代动力学和生物学效应。添加地塞米松(Dex)以尽量减少骨化三醇诱导的高钙血症,并作为KTZ抑制类固醇生物合成细胞色素P450酶的类固醇替代品。KTZ能有效抑制PC3细胞和C3H/HeJ小鼠肾组织中时间依赖性骨化三醇诱导的CYP24A1蛋白表达和酶活性。与单独使用骨化三醇相比,用骨化三醇和KTZ联合治疗的小鼠的全身骨化三醇暴露面积曲线下更高。KTZ和Dex协同增强骨化三醇介导的PC3细胞体外抗增殖作用;这种作用与细胞凋亡增强有关。用骨化三醇和KTZ/Dex治疗后,尽管胱天蛋白酶-9和胱天蛋白酶-3没有被激活,线粒体也没有释放细胞色素c,但胱天蛋白酶-8被激活,截短的Bid蛋白水平升高。观察到凋亡诱导因子向细胞核的易位,表明凋亡诱导因子介导的非胱天蛋白酶依赖性凋亡途径的作用。在PC3人前列腺癌症异种移植物小鼠模型中,钙三醇和KTZ/Dex组合抑制了克隆发生存活,并增强了单独使用钙三醇观察到的生长抑制。我们的结果表明,骨化三醇与CYP24A1抑制剂联合使用可增强抗增殖作用,增加全身骨化三醇暴露量,并促进胱天蛋白酶非依赖性凋亡途径的激活[3]。
|
||
| 动物实验 |
|
||
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Ketoconazole requires an acidic environment to become soluble in water. At pH values above 3 it becomes increasingly insoluble with about 10% entering solution in 1 h. At pH less than 3 dissolution is 85% complete in 5 min and entirely complete within 30 min. A single 200 mg oral dose produces a Cmax of 2.5-3 mcg/mL with a Tmax of 1-4 h. Administering ketoconazole with food consistently increases Cmax and delays Tmax but literature is contradictory regarding the effect on AUC, which may experience a small decrease. A bioavailablity of 76% has been reported for ketoconazole. Only 2-4% of the ketoconazole dose is eliminated unchanged in the urine. Over 95% is eliminated through hepatic metabolism. Ketoconazole has an estimated volume of distribution of 25.41 L or 0.36 L/kg. It distributes widely among the tissues, reaching effective concentrations in the skin, tendons, tears, and saliva. Distribution to vaginal tissue produces concentrations 2.4 times lower than plasma. Penetration into the CNS, bone, and seminal fluid are minimal. Ketoconazole has been found to enter the breast milk and cross the placenta in animal studies. Ketoconazole has an estimated clearance of 8.66 L/h. Ketoconazole is rapidly absorbed from the GI tract. Following oral administration, ketoconazole is dissolved in gastric secretions and converted to the hydrochloride salt prior to absorption from the stomach. The effect of food on the rate and extent of GI absorption of ketoconazole has not been clearly determined. Some clinicians have reported that administration of ketoconazole to fasting individuals results in higher plasma concentrations of the drug than does administration with food. However, the manufacturer states that administration of ketoconazole with food increases the extent of absorption and results in more consistent plasma concentrations of the drug. The manufacturer suggests that food increases absorption of ketoconazole by increasing the rate and/or extent of dissolution of ketoconazole (e.g., by increasing bile secretions) or by delaying stomach emptying. Ketoconazole is a weak dibasic agent and thus requires acidity for dissolution and absorption. The bioavailability of oral ketoconazole depends on the pH of the gastric contents in the stomach; an increase in the pH results in decreased absorption of the drug. Decreased bioavailability of ketoconazole has been reported in patients with acquired immunodeficiency syndrome (AIDS), probably because of gastric hypochlorhydria associated with this condition; concomitant administration of dilute hydrochloric acid solution normalized absorption of the drug in these patients.198 Concomitant administration of an acidic beverage may increase bioavailability of oral ketoconazole in some individuals with achlorhydria. For more Absorption, Distribution and Excretion (Complete) data for KETOCONAZOLE (19 total), please visit the HSDB record page. Metabolism / Metabolites The major metabolite of ketoconazole appears to be M2, an end product resulting from oxidation of the imidazole moiety. CYP3A4 is known to be the primary contributor to this reaction with some contribution from CYP2D6. Other metabolites resulting from CYP3A4 mediated oxidation of the imidazole moiety include M3, M4, and M5. Ketoconazole may also undergo N-deacetylation to M14, , alkyl oxidation to M7, N-oxidation to M13, or aromatic hydroxylation to M8, or hydroxylation to M9. M9 may further undergo oxidation of the hydroxyl to form M12, N-dealkylation to form M10 with a subsequent N-dealkylation to M15, or may form an iminium ion. No metabolites are known to be active however oxidation metabolites of M14 have been implicated in cytotoxicity. Ketoconazole is partially metabolized, in the liver, to several inactive metabolites by oxidation and degradation of the imidazole and piperazine rings, by oxidative O-dealkylation, and by aromatic hydroxylation. Biological Half-Life Ketoconazole experiences biphasic elimination with the first phase having a half-life of 2 hours and a terminal half life of 8 hours. Plasma concentrations of ketoconazole appear to decline in a biphasic manner with a half-life of approximately 2 hours in the initial phase and approximately 8 hours in the terminal phase. Elimination from plasma is biphasic with a half-life of 2 hours during the first 10 hours and 8 hours thereafter. |
||
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
IDENTIFICATION AND USE: Ketokonazole is used as antifungal medication. HUMAN EXPOSURE AND TOXICITY: Transient increases in serum AST, ALT, and alkaline phosphatase concentrations may occur during ketoconazole therapy. Serious hepatotoxicity has occurred in patients receiving oral ketoconazole, including cases that were fatal or required liver transplantation. Hepatotoxicity may be hepatocellular (in most cases), cholestatic, or a mixed pattern of injury. Although ketoconazole-induced hepatotoxicity usually is reversible following discontinuance of the drug, recovery may take several months and rarely death has occurred. Symptomatic hepatotoxicity usually is apparent within the first few months of ketoconazole therapy, but occasionally may be apparent within the first week of therapy. Some patients with ketoconazole-induced hepatotoxicity had no obvious risk factors for liver disease. Serious hepatotoxicity has been reported in patients receiving high oral ketoconazole dosage for short treatment durations and in patients receiving low oral dosage of the drug for long durations. Many of the reported cases of hepatotoxicity occurred in patients who received the drug for the treatment of tinea unguium (onychomycosi or the treatment of chronic, refractory dermatophytoses. Ketoconazole-induced hepatitis has been reported in some children. Usual dosages (ie, 200-400 mg daily) of ketoconazole have been reported to transiently (for 2-12 hours) inhibit testicular testosterone synthesis. A compensatory increase in serum luteinizing hormone (LH) concentrations may occur. Dosages of 800-1200 mg daily have been reported to have a more prolonged effect on testosterone synthesis; in one study in males receiving these high dosages, serum testosterone concentrations remained at a subnormal level (ie, less than 300 ng/dL) throughout the day in about 30% of those receiving 800 mg daily and in all of those receiving 1200 mg daily. Oligospermia, decreased libido, and impotence often occurred in these males and azoospermia occurred rarely. The drug apparently directly inhibits synthesis of adrenal steroids and testosterone in vitro and in vivo. Ketoconazole appears to inhibit steroid synthesis principally by blocking several P-450 enzyme systems (eg, 11beta-hydroxylase, C-17,20-lyase, cholesterol side-chain cleavage enzyme). Overall the results show that many of the commonly used azole fungicides act as endocrine disruptors in vivo, although the profile of action in vivo varies. As ketoconazole is known to implicate numerous endocrine-disrupting effects in humans. ANIMAL STUDIES: After oral administration toxicity was manifested in mice, rats and guinea pigs by sedation, catalepsy, ataxia, tremors, convulsions and pre-lethal loss of the righting reflex at doses >320 mg/kg. In dogs, toxicity was manifested by diarrhea and vomiting at doses >80 mg/kg. Ketoconazole has been administered by the oral (gavage) and intravenous routes to mice, rats, guinea pigs and dogs. Toxicity after intravenous administration was manifested by spasms, convulsions and dyspnea in rats, mice and guinea pigs; pre-lethal loss of the righting reflex occurred in mice and guinea pigs, and dogs. Toxicity in dogs was also manifested by licking and convulsions. In rats the overall incidence of and type of tumors was not significantly different between treated and control groups, except for high-dosed female rats who had a decrease of the overall tumor rate. In developmental studies in rats the incidence of stillborn fetuses increased from a control value of 0.5% to 32.7% in rats dosed with 40 mg/kg and cannibalization of young occurred in two litters. In mice a significant decline in sperm motility and density in cauda epididymis was noted. A sharp decline in fertility (50% negative) in ketoconazole treated mice was observed. A significant reduction in the total protein and sialic acid contents of testes, epididymis, seminal vesicle and ventral prostate were noticed. The cholesterol contents of testes were raised while fructose contents of seminal vesicle were reduced significantly. The ketoconazole treatment altered the biochemical milieu of the reproductive tract. In the rabbit, ketoconazole produces evidence of maternal toxicity, embryotoxicity and teratogenicity at a high dose of 40 mg/kg/day. Ketoconazole did not show any signs of mutagenic potential when evaluated using the dominant lethal mutation test or the Ames Salmonella microsomal activator assay. ECOTOXICITY STUDIES: Ketoconazole induced CYP1A and CYP3A expression in rainbow trout. However, the most pronounced effect of ketoconazole was a 60 to 90% decrease in CYP3A catalytic activities in rainbow trout and in killifish. Ketoconazole interacts with 14-α demethylase, a cytochrome P-450 enzyme necessary for the conversion of lanosterol to ergosterol. This results in inhibition of ergosterol synthesis and increased fungal cellular permeability. Other mechanisms may involve the inhibition of endogenous respiration, interaction with membrane phospholipids, inhibition of yeast transformation to mycelial forms, inhibition of purine uptake, and impairment of triglyceride and/or phospholipid biosynthesis. Ketoconazole can also inhibit the synthesis of thromboxane and sterols such as aldosterone, cortisol, and testosterone. (A1990, A1991, A1992, A1993) Hepatotoxicity Mild and transient elevations in liver enzymes occur in 4% to 20% of patients on oral ketaconazole. These abnormalities are usually transient and asymptomatic and uncommonly require dose adjustment or discontinuation. Clinically apparent hepatotoxicity from ketaconazole is well described in the literature and is estimated to occur in 1:2,000 to 1:15,000 users. The liver injury typically presents with an acute hepatitis-like picture 1 to 6 months after starting therapy. While most cases present with a hepatocellular pattern of injury, cholestatic forms have been described. Rash, fever and eosinophilia are rare as is autoantibody formation. Recovery upon stopping therapy may be delayed and generally takes 1 to 3 months. Severe cases with acute liver failure and death or need for emergency liver transplantation have been described. Likelihood score: A (well established cause cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Because there is little published experience with ketoconazole or levoketoconazole during breastfeeding and its potential liver enzyme inhibition and liver toxicity, other agents are preferred. The manufacturers recommend that mothers taking ketoconazole or levoketoconazole avoid breastfeeding during treatment and for 1 day after the last dose. Use of ketoconazole shampoo or topical use on the skin by the mother poses little to no risk to the breastfed infant. However, topical use on the breast or nipples should be avoided in nursing mothers because of possible oral ingestion by the infant and the availability of safer alternatives. Only water-miscible cream or gel products should be applied to the breast because ointments may expose the infant to high levels of mineral paraffins via licking. ◉ Effects in Breastfed Infants A mother taking ketoconazole 200 mg orally for 10 days noticed no adverse effects in her breastfed 1-month-old infant. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding Ketoconazole is approximately 84% bound to plasma albumin with another 15% associated with blood cells for a total of 99% binding within the plasma. Toxicity Data Hepatotoxicity, LD50=86 mg/kg (orally in rat) LD50: 44 mg/kg (Intravenous, Mouse) (T66) LD50: 702 mg/kg (Oral, Mouse) (T66) Interactions Because gastric acidity is necessary for the dissolution and absorption of ketoconazole, concomitant use of drugs that decrease gastric acid output or increase gastric pH (e.g., antacids, antimuscarinics, histamine H2-receptor antagonists, proton-pump inhibitors, sucralfate) may decrease absorption of ketoconazole resulting in decreased plasma concentrations of the antifungal. Concomitant use of antacids, antimuscarinics, histamine H2-receptor antagonists, proton-pump inhibitors (e.g., omeprazole, lanosprazole), or sucralfate is not recommended in patients receiving ketoconazole. Elevated plasma concentrations of digoxin have been reported in patients receiving ketoconazole. Although it is unclear whether concomitant use of ketoconazole caused these increased concentrations, digoxin concentrations should be monitored closely in patients receiving the antifungal agent. Like other imidazole derivatives, ketoconazole may enhance the anticoagulant effect of coumarin anticoagulants. When ketoconazole is used concomitantly with these drugs, the anticoagulant effect should be carefully monitored and dosage of the anticoagulant adjusted accordingly. Concomitant use of mefloquine (single 500-mg dose) and ketoconazole (400 mg once daily for 10 days) in healthy adults increased the mean peak plasma concentration and AUC of mefloquine by 64 and 79%, respectively, and increased the mean elimination half-life of mefloquine from 322 hours to 448 hours. Because of the risk of a potentially fatal prolongation of the corrected QT (QTc) interval, the manufacturer of mefloquine states that ketoconazole should not be used concomitantly with mefloquine or within 15 weeks after the last mefloquine dose. For more Interactions (Complete) data for KETOCONAZOLE (51 total), please visit the HSDB record page. Non-Human Toxicity Values LD50 Rats oral 166 mg/kg LD50 Rats iv 86 mg/kg LD50 Mice oral 618 mg/kg LD50 Mice iv 41,500 ug/kg LD50 Dog oral 178 mg/kg |
||
| 参考文献 |
|
||
| 其他信息 |
Therapeutic Uses
Antifungal agents Nizoral Tablets should be used only when other effective antifungal therapy is not available or tolerated and the potential benefits are considered to outweigh the potential risks. Nizoral (ketoconazole) Tablets are indicated for the treatment of the following systemic fungal infections in patients who have failed or who are intolerant to other therapies: blastomycosis, coccidioidomycosis, histoplasmosis, chromomycosis, and paracoccidioidomycosis. Nizoral Tablets should not be used for fungal meningitis because it penetrates poorly into the cerebrospinal fluid. /Included in US product label/ Oral ketoconazole has been used for the palliative treatment of Cushing's syndrome (hypercortisolism), including adrenocortical hyperfunction associated with adrenal or pituitary adenoma or ectopic corticotropin-secreting tumors. Based on ketoconazole's endocrine effects, the drug has been used in the treatment of advanced prostatic carcinoma. Safety and efficacy of ketoconazole have not been established for either of these indications. Oral ketoconazole also has been used in the treatment of hypercalcemia in patients with sarcoidosis and the treatment of tuberculosis-associated hypercalcemia and idiopathic infantile hypercalcemia and hypercalciuria. /NOT included in US product label/ Ketoconazole has been used for the treatment of sporotrichosis caused by Sporothrix schenckii; however, the drug is not recommended since it is less effective and associated with more adverse effects than some other azoles. Oral itraconazole is considered the drug of choice for the treatment of cutaneous, lymphocutaneous, or mild pulmonary or osteoarticular sporotrichosis and for follow-up therapy in more severe infections after a response has been obtained with IV amphotericin B. /NOT included in US product label/ For more Therapeutic Uses (Complete) data for KETOCONAZOLE (18 total), please visit the HSDB record page. Drug Warnings /BOXED WARNING/ WARNING. Nizoral Tablets should be used only when other effective antifungal therapy is not available or tolerated and the potential benefits are considered to outweigh the potential risks. Hepatotoxicity: Serious hepatotoxicity, including cases with a fatal outcome or requiring liver transplantation has occurred with the use of oral ketoconazole. Some patients had no obvious risk factors for liver disease. Patients receiving this drug should be informed by the physician of the risk and should be closely monitored. QT Prolongation and Drug Interactions Leading to QT Prolongation: Co-administration of the following drugs with ketoconazole is contraindicated: dofetilide, quinidine, pimozide, cisapride, methadone, disopyramide, dronedarone, ranolazine. Ketoconazole can cause elevated plasma concentrations of these drugs and may prolong QT intervals, sometimes resulting in life-threatening ventricular dysrhythmias such as torsades de pointes. Transient increases in serum AST, ALT, and alkaline phosphatase concentrations may occur during ketoconazole therapy. Serious hepatotoxicity has occurred in patients receiving oral ketoconazole, including cases that were fatal or required liver transplantation. Hepatotoxicity may be hepatocellular (in most cases), cholestatic, or a mixed pattern of injury. Although ketoconazole-induced hepatotoxicity usually is reversible following discontinuance of the drug, recovery may take several months and rarely death has occurred. Symptomatic hepatotoxicity usually is apparent within the first few months of ketoconazole therapy, but occasionally may be apparent within the first week of therapy. Some patients with ketoconazole-induced hepatotoxicity had no obvious risk factors for liver disease. Serious hepatotoxicity has been reported in patients receiving high oral ketoconazole dosage for short treatment durations and in patients receiving low oral dosage of the drug for long durations. Many of the reported cases of hepatotoxicity occurred in patients who received the drug for the treatment of tinea unguium (onychomycosi or the treatment of chronic, refractory dermatophytoses. Ketoconazole-induced hepatitis has been reported in some children. Coadministration of a number of CYP3A4 substrates such as dofetilide, quinidine cisapride and pimozide is contraindicated with Nizoral Tablets. Coadministration with ketoconazole can cause elevated plasma concentrations of these drugs and may increase or prolong both therapeutic and adverse effects to such an extent that a potentially serious adverse reaction may occur. For example, increased plasma concentrations of some of these drugs can lead to QT prolongation and sometimes resulting in life-threatening ventricular tachyarrhythmias including occurrences of torsades de pointes, a potentially fatal arrhythmia. Additionally, the following other drugs are contraindicated with Nizoral Tablets: methadone, disopyramide, dronedarone, ergot alkaloids such as dihydroergotamine, ergometrine, ergotamine, methylergometrine, irinotecan, lurasidone, oral midazolam, alprazolam, triazolam, felodipine, nisoldipine, ranolazine, tolvaptan, eplerenone, lovastatin, simvastatin and colchicine. The use of Nizoral Tablets is contraindicated in patients with acute or chronic liver disease. For more Drug Warnings (Complete) data for KETOCONAZOLE (46 total), please visit the HSDB record page. Pharmacodynamics Ketoconazole, similarly to other azole antifungals, is a fungistatic agent which causes growth arrest in fungal cells thereby preventing growth and spread of the fungus throughout the body. |
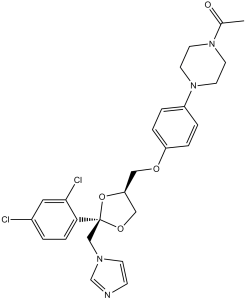
| 分子式 |
C26H28CL2N4O4
|
|---|---|
| 分子量 |
531.4309
|
| 精确质量 |
530.148
|
| 元素分析 |
C, 58.76; H, 5.31; Cl, 13.34; N, 10.54; O, 12.04
|
| CAS号 |
65277-42-1
|
| 相关CAS号 |
(+)-Ketoconazole;142128-59-4;(-)-Ketoconazole;142128-57-2;Ketoconazole-d8;1217706-96-1;Ketoconazole-d4;1398065-75-2
|
| PubChem CID |
456201
|
| 外观&性状 |
White to off-white solid powder
|
| 密度 |
1.4±0.1 g/cm3
|
| 沸点 |
753.4±60.0 °C at 760 mmHg
|
| 熔点 |
146°C
|
| 闪点 |
409.4±32.9 °C
|
| 蒸汽压 |
0.0±2.5 mmHg at 25°C
|
| 折射率 |
1.642
|
| LogP |
3.55
|
| tPSA |
69.06
|
| 氢键供体(HBD)数目 |
0
|
| 氢键受体(HBA)数目 |
6
|
| 可旋转键数目(RBC) |
7
|
| 重原子数目 |
36
|
| 分子复杂度/Complexity |
735
|
| 定义原子立体中心数目 |
2
|
| SMILES |
CC(=O)N1CCN(CC1)C2=CC=C(C=C2)OC[C@H]3CO[C@](O3)(CN4C=CN=C4)C5=C(C=C(C=C5)Cl)Cl
|
| InChi Key |
XMAYWYJOQHXEEK-OZXSUGGESA-N
|
| InChi Code |
InChI=1S/C26H28Cl2N4O4/c1-19(33)31-10-12-32(13-11-31)21-3-5-22(6-4-21)34-15-23-16-35-26(36-23,17-30-9-8-29-18-30)24-7-2-20(27)14-25(24)28/h2-9,14,18,23H,10-13,15-17H2,1H3/t23-,26-/m0/s1
|
| 化学名 |
1-[4-[4-[[(2R,4S)-2-(2,4-dichlorophenyl)-2-(imidazol-1-ylmethyl)-1,3-dioxolan-4-yl]methoxy]phenyl]piperazin-1-yl]ethanone
|
| 别名 |
Ketoconazole; Nizoral, Kuric, (+)-Ketoconazole; 65277-42-1; 142128-59-4; (2R,4S)-ketoconazole; Kuric; MFCD00058579; Fungoral, Ketoderm; Xolegel, Extina
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: 2.5 mg/mL (4.70 mM) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (4.70 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (4.70 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 配方 4 中的溶解度: 30% propylene glycol, 5% Tween 80, 65% D5W: 30mg/mL 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.8817 mL | 9.4086 mL | 18.8172 mL | |
| 5 mM | 0.3763 mL | 1.8817 mL | 3.7634 mL | |
| 10 mM | 0.1882 mL | 0.9409 mL | 1.8817 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT04869449 | Recruiting | Drug: Ketoconazole | Glioblastoma Glioblastoma Multiforme |
Milton S. Hershey Medical Center | May 12, 2022 | Early Phase 1 |
| NCT04212000 | Completed | Drug: Levoketoconazole Drug: Ketoconazole |
Healthy | Cortendo AB | December 16, 2019 | Phase 1 |
| NCT00830388 | Completed Has Results | Drug: Ketoconazole 2% Foam | Tinea Versicolor | Boni Elewski, MD | November 2008 | Phase 4 |
| NCT01330563 | Completed | Drug: CKD-501, Ketoconazole | Type 2 Diabetes Mellitus | Chong Kun Dang Pharmaceutical | March 2011 | Phase 1 |
|
|
|