| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 5g |
|
||
| 10g |
|
||
| 25g |
|
||
| Other Sizes |
|

| 靶点 |
Human Endogenous Metabolite; synthetic form of the thyroid hormone thyroxine (T4)
|
|---|---|
| 体外研究 (In Vitro) |
促甲状腺激素 (TSH) 水平与脱碘酶 (DIO) 相关,脱碘酶可催化甲状腺素(激素原)转化为活性甲状腺激素。 DIO3 起到抑制甲状腺激素分泌的作用,而 DIO1 和 DIO2 则催化甲状腺激素分泌的激活。垂体TSH分泌的负反馈调节很大程度上依赖于DIO1和DIO2的活性[1]。已知离子通道、泵和调节性收缩蛋白的表达受三碘甲状腺原氨酸 (T3) 和左旋甲状腺素 (T4) 激素的调节。此外,已证明甲状腺激素影响负责兴奋和收缩的钙流动和稳态,L-甲状腺素和三碘甲状腺原氨酸影响该过程的药理调节和分泌。与喂养标准饮食的对照组相比,喂养无碘饮食 12 周的大鼠的 L-甲状腺素和三碘甲状腺原氨酸水平显着降低(p<0.001)。在接受低剂量药物治疗的组中,L-甲状腺素水平升高(p=0.02),但三碘甲状腺原氨酸水平基本上与对照组相同(p=0.19)。与未治疗的甲状腺功能减退组相比,给予大剂量 L-甲状腺素的大鼠显示三碘甲状腺原氨酸和 L-甲状腺素的循环浓度显着增加(分别为 p<0.001 和 p=0.004),并且L-甲状腺素水平相对于对照值 (p=0.03)[2]。
|
| 体内研究 (In Vivo) |
促甲状腺激素 (TSH) 水平与脱碘酶 (DIO) 催化甲状腺素(激素原)转化为活性甲状腺激素相关。甲状腺激素分泌由 DIO1 和 DIO2 激活,而分泌由 DIO3 灭活。负反馈对垂体TSH分泌的调节很大程度上依赖于DIO1和DIO2的作用[1]。离子通道、泵和调节收缩蛋白的表达受三碘甲状腺原氨酸 (T3) 和 L-甲状腺素 (T4) 激素的调节。此外,已证明甲状腺激素影响钙稳态和通量,负责兴奋和收缩。已知三碘甲状腺原氨酸和 L-甲状腺素可以改变钙的药理调节和分泌。与给予常规饮食的对照组相比,给予无碘饮食 12 周的大鼠的三碘甲状腺原氨酸和 L-甲状腺素水平显着降低(p<0.001)。三碘甲状腺原氨酸水平与对照组基本相当(p=0.19),但低剂量 L-甲状腺素治疗组中 L-甲状腺素有所增加(p=0.02)。与未治疗的甲状腺功能减退组相比,接受高剂量 L-甲状腺素治疗的大鼠表现出显着更高的三碘甲状腺原氨酸和 L-甲状腺素循环浓度(分别为 p<0.001 和 p=0.004),并且 L-甲状腺素水平显着高于对照组值(p=0.03)[2]。
|
| 细胞实验 |
生化技术[2]
根据制造商的方案,使用标准大鼠甲状腺素(T4)和T3 ELISA试剂盒进行ELISA测定。如前所述,进行了蛋白质印迹分析。
|
| 动物实验 |
Rats: The experiment uses 22 female Sprague-Dawley rats. There are four groups of non-pregnant rats: 1) No thyroid function, 2) hypothyroidism, 3) hypothyroidism treated with low doses of L-thyroxine (20 μg/kg/day), and 4) high doses of L-thyroxine (100 μg/kg/day). While the intervention rats (groups 2-4) are fed an iodine-free diet for 12 weeks to induce hypothyroidism, the control group (group 1) is fed a standard diet. This is followed by an additional 4 weeks of feeding to allow for L-thyroxine treatment and screening for hypothyroidism. You have unlimited access to food and water (iodine-free diet). Groups 3 and 4, which represent the hypothyroid group, receive intraperitoneal injections of 20 μg/kg and 100 μg/kg of L-thyroxine per day, respectively, every 24 hours. Within weeks 12 and 16 of starting the iodine-free or control diet, blood samples are taken for thyroid function screening. After treatment, a hysterectomy is performed under general anesthesia (isoflurane 2%), and the two uterine horns are kept in physiological Krebs' solution until isometric tension measurements are taken, which should take no longer than an hour.
|
| 药代性质 (ADME/PK) |
Absorption
Absorption of orally administered T4 from the gastrointestinal tract ranges from 40% to 80% with the majority of the levothyroxine dose absorbed from the jejunum and upper ileum. T4 absorption is increased by fasting, and decreased in malabsorption syndromes and by certain foods such as soybeans, milk, and dietary fiber. Absorption may also decrease with age. In addition, many drugs affect T4 absorption including bile acide sequestrants, sucralfate, proton pump inhibitors, and minerals such as calcium (including in yogurt and milk products), magnesium, iron, and aluminum supplements. To prevent the formation of insoluble chelates, levothyroxine should generally be taken on an empty stomach at least 2 hours before a meal and separated by at least 4 hours from any interacting agents. Route of Elimination Thyroid hormones are primarily eliminated by the kidneys. A portion of the conjugated hormone reaches the colon unchanged and is eliminated in the feces. Approximately 20% of T4 is eliminated in the stool. Urinary excretion of T4 decreases with age. Circulating thyroid hormones are greater than 99% bound to plasma proteins, including thyroxine-binding globulin (TBG), thyroxine-binding prealbumin (TBPA), and albumin (TBA), whose capacities and affinities vary for each hormone. The higher affinity of both TBG and TBPA for T4 partially explains the higher serum levels, slower metabolic clearance, and longer half-life of T4 compared to T3. Protein-bound thyroid hormones exist in reverse equilibrium with small amounts of free hormone. Only unbound hormone is metabolically active. Many drugs and physiologic conditions affect the binding of thyroid hormones to serum proteins. Thyroid hormones do not readily cross the placental barrier. NIH; DailyMed. Current Medication Information for Synthroid (Levothyroxine Sodium) Tablet (Updated: December 2015). Available from, as of April 4, 2016: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=665c1eab-2649-498b-8da8-b15b3b743a21 Levothyroxine Sodium for Injection is administered via the intravenous route. Following administration, the synthetic levothyroxine cannot be distinguished from the natural hormone that is secreted endogenously. NIH; DailyMed. Current Medication Information for Levothyroxine Sodium (Levothyroxine Sodium) Anhydrous Injection, Powder, Lyophilized, For Solution (Updated: March 2015). Available from, as of April 4, 2016: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=f88f44d8-2f18-4155-9d78-6323d19fbafe Absorption of orally administered T4 from the gastrointestinal (GI) tract ranges from 40% to 80%. The majority of the levothyroxine dose is absorbed from the jejunum and upper ileum. The relative bioavailability of Synthroid tablets, compared to an equal nominal dose of oral levothyroxine sodium solution, is approximately 93%. T4 absorption is increased by fasting, and decreased in malabsorption syndromes and by certain foods such as soybean infant formula. Dietary fiber decreases bioavailability of T4. Absorption may also decrease with age. In addition, many drugs and foods affect T4 absorption. NIH; DailyMed. Current Medication Information for Synthroid (Levothyroxine Sodium) Tablet (Updated: December 2015). Available from, as of April 4, 2016: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=665c1eab-2649-498b-8da8-b15b3b743a21 Levothyroxine is variably absorbed from the GI tract (range: 40-80%). In animals, levothyroxine is absorbed in the proximal and middle jejunum; the drug is not absorbed from the stomach or distal colon and little, if any, absorption occurs in the duodenum. Studies in humans indicate that levothyroxine is absorbed from the jejunum and ileum and some absorption also occurs in the duodenum. The degree of absorption of levothyroxine from the GI tract depends on the product formulation and type of intestinal contents, including plasma protein and soluble dietary factors that may bind thyroid hormone and make it unavailable for diffusion. In addition, concurrent oral administration of infant soybean formula, soybean flour, cotton seed meal, walnuts, foods containing large amounts of fiber, ferrous sulfate, antacids, sucralfate, calcium carbonate, cation-exchange resins (e.g., sodium polystyrene sulfonate), simethicone, or bile acid sequestrants may decrease absorption of levothyroxine. The extent of levothyroxine absorption is increased in the fasting state and decreased in malabsorption states (e.g., sprue); absorption also may decrease with age. American Society of Health-System Pharmacists 2015; Drug Information 2015. Bethesda, MD. 2015, p. 3230 For more Absorption, Distribution and Excretion (Complete) data for LEVOTHYROXINE (7 total), please visit the HSDB record page. Metabolism / Metabolites Approximately 70% of secreted T4 is deiodinated to equal amounts of T3 and reverse triiodothyronine (rT3), which is calorigenically inactive. T4 is slowly eliminated through its major metabolic pathway to T3 via sequential deiodination, where approximately 80% of circulating T3 is derived from peripheral T4. The liver is the major site of degradation for both T4 and T3, with T4 deiodination also occurring at a number of additional sites, including the kidney and other tissues. Elimination of T4 and T3 involves hepatic conjugation to glucuronic and sulfuric acids. The hormones undergo enterohepatic circulation as conjugates are hydrolyzed in the intestine and reabsorbed. Conjugated compounds that reach the colon are hydrolyzed and eliminated as free compounds in the feces. Other minor T4 metabolites have been identified. Yields l-tyrosine in rabbit, in rat /From table/ Goodwin, B.L. Handbook of Intermediary Metabolism of Aromatic Compounds. New York: Wiley, 1976., p. T-14 Yields 3,3',5-triiodo-L-thyronine in man, rat, dog, rabbit. /From table/ Goodwin, B.L. Handbook of Intermediary Metabolism of Aromatic Compounds. New York: Wiley, 1976., p. T-14 Yields l-thyroxine-4'-beta-d-glucuronide in dog, in man, in rat. Yields l-thyroxine-4'-sulfate in dog. /From table/ Goodwin, B.L. Handbook of Intermediary Metabolism of Aromatic Compounds. New York: Wiley, 1976., p. T-14 Yields 3,3',5,5'-tetraiodothyropyruvic acid in rat. Yields l-thyronine in rat. /From table/ Goodwin, B.L. Handbook of Intermediary Metabolism of Aromatic Compounds. New York: Wiley, 1976., p. T-14 Yields 3,3'-diiodo-l-thyronine in dog. Yields 3,3',5,5'-tetraiodothyroacetic acid in man, in rat. /From table/ Goodwin, B.L. Handbook of Intermediary Metabolism of Aromatic Compounds. New York: Wiley, 1976., p. T-14 Biological Half-Life T4 half-life is 6 to 7 days. T3 half-life is 1 to 2 days. In dogs orally administered levothyroxine has relatively ... short elimination half life when compared to humans. ... The serum half life is approximately 12-16 hours. Plumb D.C. Veterinary Drug Handbook. 8th ed. (pocket). Ames, IA: Wiley-Blackwell, 2015., p. 842 The usual plasma half-lives of thyroxine and triiodothyronine are 6-7 days and approximately 1-2 days, respectively. The plasma half-lives of thyroxine and triiodothyronine are decreased in patients with hyperthyroidism and increased in those with hypothyroidism. |
| 毒性/毒理 (Toxicokinetics/TK) |
Effects During Pregnancy and Lactation
◉ Summary of Use during Lactation Levothyroxine (T4) is a normal component of human milk. Limited data on exogenous replacement doses of levothyroxine during breastfeeding indicate no adverse effects in infants. The American Thyroid Association recommends that subclinical and overt hypothyroidism should be treated with levothyroxine in lactating women seeking to breastfeed. Adequate levothyroxine treatment during lactation may normalize milk production in hypothyroid lactating mothers with low milk supply. Levothyroxine dosage requirement may be increased in the postpartum period compared to prepregnancy requirements in patients with Hashimoto's thyroiditis. ◉ Effects in Breastfed Infants Effects of exogenous thyroid hormone administration to mothers on their infant have not been reported. One case of apparent mitigation of cretinism in hypothyroid infants by breastfeeding has been reported, but the amounts of thyroid hormones in milk are not optimal, and this result has been disputed. The thyroid hormone content of human milk from the mothers of very preterm infants appears not to be sufficient to affect the infants' thyroid status. The amounts of thyroid hormones in milk are apparently not sufficient to interfere with diagnosis of hypothyroidism. In a telephone follow-up study, 5 nursing mothers reported taking levothyroxine (dosage unspecified). The mothers reported no adverse reactions in their infants. One mother who had undergone a thyroidectomy was taking levothyroxine 100 mcg daily as well as calcium carbonate and calcitriol. Her breastfed infant was reportedly "thriving" at 3 months of age. A woman with propionic acidemia took levothyroxine 50 mcg daily as well as biotin, carnitine, and various amino acids while exclusively breastfeeding her infant for 2 months and nonexclusively for 10 months. At that time, the infant had normal growth and development. ◉ Effects on Lactation and Breastmilk Adequate thyroid hormone serum levels are required for normal lactation. Replacing deficient thyroid levels should improve milk production caused by hypothyroidism. Supraphysiologic doses would not be expected to further improve lactation. |
| 参考文献 |
|
| 其他信息 |
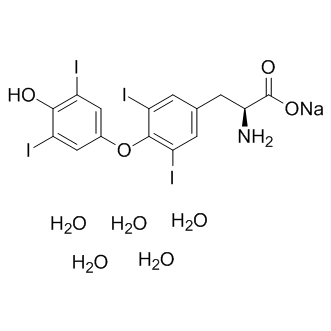
Levothyroxine Sodium is the sodium salt of levothyroxine, a synthetic levoisomer of thyroxine (T4) that is similar to the endogenous hormone produced by the thyroid gland. In peripheral tissues, levothyroxine is deiodinated by 5'-deiodinase to form triiodothyronine (T3). T3 enters the cell and binds to nuclear thyroid hormone receptors; the activated hormone-receptor complex in turn triggers gene expression and produces proteins required in the regulation of cellular respiration; thermogenesis; cellular growth and differentiation; and the metabolism of proteins, carbohydrates and lipids. T3 also exhibits cardiostimulatory effects.
The major hormone derived from the thyroid gland. Thyroxine is synthesized via the iodination of tyrosines (MONOIODOTYROSINE) and the coupling of iodotyrosines (DIIODOTYROSINE) in the THYROGLOBULIN. Thyroxine is released from thyroglobulin by proteolysis and secreted into the blood. Thyroxine is peripherally deiodinated to form TRIIODOTHYRONINE which exerts a broad spectrum of stimulatory effects on cell metabolism. |
| 分子式 |
C15H20I4NNAO9
|
|---|---|
| 分子量 |
888.926400000001
|
| 精确质量 |
888.721
|
| CAS号 |
6106-07-6
|
| 相关CAS号 |
Thyroxine sulfate;77074-49-8;L-Thyroxine;51-48-9;L-Thyroxine sodium;55-03-8
|
| PubChem CID |
23665037
|
| 外观&性状 |
White to light yellow solid
|
| 密度 |
2.381
|
| 熔点 |
207-210 (dec.)(lit.)
|
| LogP |
3.601
|
| tPSA |
141.76
|
| 氢键供体(HBD)数目 |
7
|
| 氢键受体(HBA)数目 |
10
|
| 可旋转键数目(RBC) |
5
|
| 重原子数目 |
30
|
| 分子复杂度/Complexity |
426
|
| 定义原子立体中心数目 |
1
|
| SMILES |
[O-]C([C@H](CC1=CC(I)=C(C(I)=C1)OC2=CC(I)=C(O)C(I)=C2)N)=O.[Na+].O.O.O.O.O
|
| InChi Key |
JMHCCAYJTTWMCX-QWPJCUCISA-M
|
| InChi Code |
InChI=1S/C15H11I4NO4.Na.5H2O/c16-8-4-7(5-9(17)13(8)21)24-14-10(18)1-6(2-11(14)19)3-12(20)15(22)23;;;;;;/h1-2,4-5,12,21H,3,20H2,(H,22,23);;5*1H2/q;+1;;;;;/p-1/t12-;;;;;;/m0....../s1
|
| 化学名 |
sodium;(2S)-2-amino-3-[4-(4-hydroxy-3,5-diiodophenoxy)-3,5-diiodophenyl]propanoate;pentahydrate
|
| 别名 |
L-Thyroxine sodium salt pentahydrate; L-Thyroxine sodium salt pentahydrate; 6106-07-6; L-Thyroxine sodium pentahydrate; Sodium L-thyroxine pentahydrate; levothyroxine sodium pentahydrate; Levothyroxine sodium; Sodium levothyroxine; eltroxin; Sodium levothyroxine pentahydrate
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO: ~100 mg/mL (~112.5 mM)
|
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (2.81 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: 2.5 mg/mL (2.81 mM) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 悬浊液; 超声助溶。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.1249 mL | 5.6247 mL | 11.2495 mL | |
| 5 mM | 0.2250 mL | 1.1249 mL | 2.2499 mL | |
| 10 mM | 0.1125 mL | 0.5625 mL | 1.1249 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。