| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g | |||
| Other Sizes |

| 靶点 |
Tubulin; Microtubule (Ki = 85 nM)
|
||
|---|---|---|---|
| 体外研究 (In Vitro) |
长春新碱的 Ki 值为 85 nM,可抑制稳态微管组装末端微管蛋白二聚体的净添加[1]。在低剂量下,长春新碱可抑制有丝分裂,并通过稳定纺锤体引起中期停滞,从而防止染色体分离。当使用较高浓度时,长春新碱有可能导致微管完全解聚[2]。长春新碱的 IC50 为 0.1 μM,可抑制 SH-SY5Y 细胞的增殖并导致肿瘤细胞凋亡。 Vincristine 降低细胞周期蛋白 D 的表达,同时诱导有丝分裂停滞并促进 caspase-3、-9 和细胞周期蛋白 B 的产生[3]。长春新碱诱导的神经毒性是由微管活性破坏引起的,它阻碍轴突运输并最终导致轴突变性[4]。
对Vincristine/长春花碱(一种新的长春新碱衍生物)和三种临床使用的长春花碱衍生物(长春花碱、长春新素和长春地辛)在稳态下抑制牛脑微管组装端的网状微管蛋白的能力进行了检测。尽管这四种衍生物的效力大致相似,但它们抑制微管蛋白的相对能力是可以区分的。Vinepidine和长春新碱是最有效的衍生物(Ki,分别为0.079+/-0.018(SD)微M和0.085+/-0.013微M),其次是长春地辛(Ki)(0.110+/-0.007微M)和长春碱(Ki为0.178+/-0.025微M)。与它们在体外抑制微管组装的相对能力相反,长春花碱及其衍生物长春地辛在抑制培养细胞增殖方面通常比长春新碱和长春皮定更有效。在B16黑色素瘤细胞中,长春碱的效力是最弱的衍生物长春皮定的九倍。在L细胞中,长春花碱在40 nM时完全抑制了生长,而长春新碱和长春地辛引起了约25%的抑制,而长春皮定没有活性。当B16黑色素瘤细胞在注射到小鼠体内之前用药物治疗时,长春地辛是四种体外衍生物中较弱的一种,可以最好地抑制肿瘤生长。结果表明,长春花衍生物之间的化学差异在较小程度上影响了衍生物在体外抑制微管组装的能力,导致药物抑制细胞生长的能力在数量级和幅度上存在显著差异。[1] 在猫迷走神经中,以0.01、0.05和0.1 mM的浓度,在体外研究了三种长春花生物碱(Vincristine/长春新碱、长春碱和去乙酰长春碱酰胺)诱导的轴突超微结构变化。在0.1 mM的浓度下,所有三种药物都诱导了微管的破坏、副晶体结构的出现和神经丝的增加。每种药物还观察到一种新型的副晶体,每个亚基都有一个电子致密的中心核。尽管这三种化合物都会影响无髓纤维(长春碱比其他两种更严重),但只有长春碱会显著损伤有髓纤维。长春新碱在引起这些体外超微结构变化方面更有效,这与长春新素是最具神经毒性的临床体内情况形成鲜明对比。这表明,除了长春花生物碱与微管或微管蛋白的直接相互作用外,临床神经毒性还与其他因素有关。[3] 单独或联合使用Vincristine/长春新碱和SAHA对人白血病MOLT-4细胞的细胞毒性作用[7] 采用3-[4,5-二甲基噻唑-2-基]-2,5-二苯基溴化四唑(MTT)法研究微管失稳剂长春新碱和HDACi-vorinostat(SAHA)对人ALL MOLT-4细胞的细胞毒性。我们首先测试了SAHA和长春新碱单独和联合使用的细胞毒性作用。如图1a所示,在高达500 nM的SAHA浓度下,没有明显的细胞毒性。然而,当浓度达到最高水平(1000 nM)时,SAHA在48小时内的IC50为840 nM。此外,长春新碱对人白血病MOLT-4细胞表现出细胞毒性,在48小时时IC50为3.3 nM(图1b)。为了确定SAHA和长春新碱之间是否发生相互作用,测量了联合检测的细胞毒性。与单独使用每种治疗相比,用500 nM SAHA和不同浓度长春新碱(0.3至3 nM)处理的细胞显著抑制了细胞存活(图1c)。 长春新碱/Vincristine联合蛛网膜下腔出血对人T细胞白血病细胞存活的影响[7] 为了进一步探索协同细胞毒性作用,我们确定了对细胞周期分布的影响。与SAHA相比,长春新碱治疗诱导细胞周期G2/M期增加。特别是,长春新碱加SAHA的组合在短期治疗(24小时)后导致细胞几乎完全停滞在G2/M期,并在长期治疗(48小时)后诱导细胞进入亚G1期(图2a)。图2b显示了统计结果。接下来,使用组合指数(CI)方法评估协同组合[25]。CI值>1.0、1.0和<1.0分别表示药物之间存在拮抗、相加或协同作用。在G2/M期,长春新碱(0.3、1和3 nM)联合500 nM SAHA的CI值分别为1.63、0.72和0.32,亚G1期的CI值则分别为0.97、0.77和0.28(图2c)。在其他T细胞白血病细胞系CCRF-CEM中也观察到了这种协同组合效应(图2d),而不是在急性髓系白血病细胞中(附加文件1:图S2)。此外,长春新碱(1或3 nM)与不同浓度的SAHA联合使用也显示出协同作用(附加文件2:图S1)。这些数据表明,长春新碱和SAHA协同诱导细胞停滞在G2/M期,随后进入亚G1期。 SAHA联合Vincristine/长春新碱对人白血病MOLT-4细胞有丝分裂阻滞的影响[7] 为了进一步阐明细胞周期进程G2/M期的协同作用机制,我们研究了SAHA联合长春新碱对微管蛋白极化变化和有丝分裂相关蛋白的影响。如图3a所示,在无细胞条件下SAHA治疗后,微管蛋白极化没有明显变化。然而,与长春新碱联合使用时,观察到微管解聚的显著诱导(图3a)。附加文件3:图S3显示了更全面的结果,包括各种长春新碱和SAHA单独的体外微管蛋白聚合试验。为了了解微管动力学对药物治疗后有丝分裂的影响,通过β-微管蛋白染色检测了人白血病MOLT-4细胞中的微管排列。如图3b(b)所示,SAHA处理后微管分布和细胞形态没有显著变化。此外,在低长春新碱浓度下,细胞在有丝分裂中期积累,纺锤体异常(图3b(c))。在这项研究中,发现具有双极和多极组织的纺锤体分布不均,这些纺锤体具有异常的长星状微管和染色体。然而,在高长春新碱浓度下,观察到微管解聚(图3b(d))。在本研究中,长春新碱和SAHA联合使用对异常纺锤体和染色体的影响比单独使用长春新素更为明显(图3b和附加文件4:图S4)。这些结果表明,SAHA由于抑制微管动力学而增强了长春新碱的作用。 SAHA联合Vincristine/长春新碱对人白血病MOLT-4细胞凋亡途径和HDAC活性的影响[7] 线粒体在内源性和外源性凋亡途径中都起着至关重要的作用。为了测试长春新碱/SAHA介导的凋亡途径是否与线粒体功能相关,评估了线粒体跨膜电位(Δψm)的变化。如图4a所示,单独使用SAHA或长春新碱治疗不足以影响线粒体膜电位;然而,与SAHA联合治疗会以时间依赖的方式增强这一现象。Bcl-2蛋白家族在控制线粒体凋亡途径中起着调节作用。数据显示,联合治疗比单独治疗更有效地下调了Bcl-2家族促生存成员的表达,如Bcl-2、Bcl-xl和Mcl-1(图4b)。 HDAC6抑制参与了Vincristine/长春新碱诱导的细胞凋亡[7] 之前的研究结果表明,HDAC6诱导微管蛋白乙酰化会影响微管的动力学和功能[9-12]。如图5a所示,SAHA,一种泛HDACi,诱导微管蛋白乙酰化;然而,它与长春新碱的组合没有协同作用。Tubastatin A是一种特异性HDAC6抑制剂[26],用于了解HDAC6在长春新碱/SAHA处理的细胞中的作用。为了评估长春新碱与图巴他汀A联合使用的潜在益处,我们测定了联合治疗的细胞毒性,并分析了联合治疗效果。然而,与单独使用图巴司汀A相比,长春新碱显著增强了图巴司坦A的细胞毒性(图5b)。此外,长春新碱(1和3 nM)与不同浓度的图巴他汀A联合诱导细胞在G2/M期积聚,随后进入亚G1期(图5c)。在G2/M期和亚G1期,长春新碱和图巴他汀联合用药的CI值<1(图5d)。长春新碱和图巴斯汀的联合治疗显示,MPM2和PARP的激活与蛋白质印迹分析的凋亡诱导一致(图5e)。通过观察长春新碱和ACY1215在CCRF-CEM细胞中的联合处理,长春新汀和HDAC6抑制剂的联合协同作用得到了进一步证实(图5f)。这些发现表明,SAHA治疗可能通过HDAC6抑制改变细胞中的微管动力学,即使这种作用不足以将细胞阻滞在G2/M期。然而,与长春新碱结合使用时,SAHA会引起极端的微管应激,从而导致细胞死亡,长春新汀也会对微管产生影响。 |
||
| 体内研究 (In Vivo) |
分别给予接受双侧皮下异种移植 Rh12 或 Rh18 的小鼠长春新碱(3 mg/kg,腹腔注射)会导致平均生长延迟超过 120 天和超过 52 天,并且重新填充分数为 0.06% 和 5%[5]。
长春新碱/Vincristine与SAHA联合治疗体内抗肿瘤活性[7] 为了评估长春新碱与SAHA的协同作用是否具有临床相关性,研究了这种联合治疗在携带已建立的MOLT-4肿瘤异种移植物的严重联合免疫缺陷小鼠中的抗肿瘤活性。一旦肿瘤可触及(约100mm3),将小鼠随机分为载体对照组和治疗组(每组n=6)。允许所有小鼠肿瘤达到2000mm3的终点体积,体内抗肿瘤疗效表示为肿瘤生长延迟(TGD;图6a)。单独用长春新碱(0.1mg/kg,每周一次)或SAHA(50mg/kg,每天一次)治疗的小鼠TGD没有改善。然而,时序分析显示,在MOLT-4异种移植物模型中,联合治疗显示出显著的抗肿瘤活性(P = 0.0389). 此外,Kaplan-Meier曲线显示了联合治疗组的抗肿瘤活性(长春新碱,0.025 mg/kg,每周一次;蛛网膜下腔出血,200 mg/kg,每日一次)(图6b)。值得注意的是,小鼠耐受了所有治疗,没有明显的毒性迹象;未观察到明显的体重差异或其他不良副作用(图6d和附加文件5:图S5)。为了将体内抗肿瘤作用与体外鉴定的机制相关联,通过蛋白质印迹分析评估了肿瘤内的生物标志物。与体外结果一致,联合治疗显著诱导了肿瘤中胱天蛋白酶3的激活和PARP的切割,表明细胞凋亡增加(图6e)。综上所述,这些发现表明,长春新碱和SAHA在体外和体内的联合使用显著增强了长春新素诱导的细胞死亡。 指尖和脚趾失去触觉是接受抗癌药物(如长春新碱)化疗的患者最早的感觉功能障碍之一。然而,这种化疗诱导的感觉功能障碍的机制尚不完全清楚。胡须毛囊是非灵长类哺乳动物的触觉器官,其功能与人类指尖相当。在这里,我们使用小鼠胡须毛囊作为模型系统,并应用压力夹紧单纤维记录技术来探索长春新碱治疗如何影响胡须毛囊中的机械感受器。我们发现,用长春新碱对小鼠进行体内治疗会损害胡须的触觉行为反应。胡须毛囊传入神经的压力夹紧单纤维记录显示,机械刺激诱发了三种类型的机械反应,即快速适应反应(RA)、缓慢适应1型反应(SA1)和缓慢适应2型反应(SA2)。长春新碱治疗显著降低了SA1反应,但对RA和SA2反应没有显著影响。我们的研究结果表明,长春新碱选择性地损害了SA1机械感受器,导致体内胡须触觉行为反应受损。[8] 测定了人横纹肌肉瘤(RMS)异种移植物、体内选择的RMS亚系对VCR抗性、体外选择的KB系(KB-ChR8-5)对秋水仙素抗性和结肠腺癌(GC3)对长春新碱(VCR)/Vincristine的肿瘤反应性。对VCR的敏感性与单次腹腔注射后肿瘤对VCR的长期保留有关,而在具有获得性或内在VCR耐药性的肿瘤中,药物的消除速度更快。在VCR给药后72小时内,药物滞留时间延长的敏感肿瘤也显示有丝分裂积聚水平升高。VCR敏感性、VCR滞留与VCR细胞毒性有丝分裂阻滞的拟议机制之间存在良好的相关性。已经开发了一个与所获得的数据一致的模型,可以解释一系列人类肿瘤异种移植物对VCR的反应性,而不管其来源组织如何[4]。 |
||
| 酶活实验 |
体外微管蛋白聚合试验[7]
为了在无细胞条件下测定指定药物的微管聚合,进行了CytoDYNAMIX Screen 03试剂盒。通用微管蛋白缓冲液、GTP储备(100 mM)和微管蛋白(10 mg/ml)均按照方案很好地制备。在检测前,将96孔板放入分光光度计中,在37°C下预热30分钟。然后制备冰微管蛋白聚合(TP)缓冲液,所有上述过程都需要在冰上进行。接下来,将药物(2μl)加入到每个含有85μl TP缓冲液的Eppendorf中。药物必须包括DMSO(对照组)、紫杉醇(10μΜ)和长春新碱/Vincristine(10μ。紫杉醇和长春新碱作为阳性对照。紫杉醇会诱导微管聚合;相比之下,长春新碱会使微管解聚。最后,将30μl微管蛋白加入Eppendorf中,并转移到预热的96孔板上。用分光光度计测量吸光度,并在340 nm和37°C下每1分钟记录一次,持续30分钟。 VCR/长春新碱/Vincristine的体外释放曲线CS-ALG@TPGS-PL-GA-VCR采用经典透析袋法对NP进行研究。简要地,CS-ALG@TPGS-PLGA-VCR将NP(4mg)重新悬浮在PBS(2mL,0.1%w/v Tween 80,pH 5.8或pH 7.4)中,以模拟癌症细胞质环境(pH 5.8)和生理环境(pH 7.4)。随后,将再悬浮液转移到透析袋中(截留分子量为3kDa;Millipore,Billerica,MA,USA),将其浸入PBS(20mL)中,并在37°C恒温水浴中以100rpm振荡培养。在指定的时间间隔内,取出5mL释放溶液,使用紫外分光光度计在298nm处检测VCR的浓度。同时,将等比例的新鲜PBS加入到释放介质中[6]。 线粒体膜电位[7] 罗丹明123用于评估线粒体膜电位。罗丹明123是一种阳离子荧光染料,定位于线粒体。线粒体膜电位的丧失与罗丹明123保留不足和荧光强度降低有关。细胞用Vincristine/长春新碱、SAHA或其组合处理指定时间。加入罗丹明123(终浓度10μM),在37°C的黑暗中孵育30分钟。然后,收获细胞并用PBS冲洗。通过FACScan流式细胞仪和CellQuest测量荧光强度。 |
||
| 细胞实验 |
细胞活力测定[7]
MTT法验证细胞活力。首先,将细胞以4×105个细胞/孔的密度接种在1 ml培养基中的24孔板中,然后用不同浓度的Vincristine/长春新碱或单独的SAHA或两者的组合处理24和48小时。用药物处理后,将每孔100μl MTT溶液(0.5 mg/ml的磷酸盐缓冲盐水(PBS))在黑暗中加入24孔板,并在37°C下孵育。活细胞的线粒体脱氢酶将MTT(黄色)还原为不溶性甲偶氮染料(紫色)。一小时后,将结晶甲赞染料溶解在提取缓冲液(0.1 M醋酸钠缓冲液,100μl/孔)中。通过ELISA阅读器在550nm处分光光度分析吸光度。 流式细胞术分析[7] 通过流式细胞术分析细胞周期直方图的演变,以检测DNA含量的变化。将细胞(1×106)接种在2ml新鲜培养基中的6孔板中,并在指定时间内用不同浓度的Vincristine/长春新碱、SAHA或其组合处理。然后,收集细胞,用PBS洗涤,在-20°C下用70%(v/v)冰冷乙醇固定30分钟。离心固定的细胞以去除乙醇,用PBS冲洗,重新悬浮在0.1 ml DNA提取缓冲液(0.2 M Na2HPO4-0.1 M柠檬酸缓冲液,pH 7.8)中20分钟,随后在室温下在黑暗中用500μl PI溶液(80μg/ml碘化丙啶、100μg/ml RNase A和1%Triton X-100的PBS溶液)染色20分钟。数据通过FACScan流式细胞仪和CellQuest软件(Becton Dickinson)进行分析。 免疫荧光分析[7] 通过免疫荧光技术检测微管的分布和形态。将盖玻片放置在24孔板中,并用聚-d-赖氨酸涂覆至少1天,以增强附着在盖玻片上的悬浮细胞。将细胞接种到24孔板中(8×105个细胞/孔),用Vincristine/长春新碱、SAHA或两种药物处理24小时。以下实验在室温下进行。用PBS中的8%多聚甲醛固定细胞15分钟。用PBS洗涤几次后,用PBS中0.1%Triton X-100透化细胞10分钟。然后,用PBS冲洗细胞10分钟三次。为了阻断,使用了PBS中3%的BSA。1小时后,用PBS洗涤细胞,用原代β-微管蛋白抗体(1:200)孵育2小时,用FITC偶联的抗小鼠IgG抗体(1:20)孵育两小时。将含有DAPI染色的载玻片滴在载玻片上,并将盖玻片回收到载玻片上。使用蔡司LSM 510 META共聚焦显微镜检测和捕获图像。 载药纳米颗粒的体外细胞毒性[6] 使用标准WST-1测定法评估游离药物、载药NP对A549细胞和A549/紫杉醇细胞的细胞毒性。简而言之,将A549细胞和A549/紫杉醇细胞以每孔5.0×104个细胞的密度接种到96孔板上,并在37°C、5%CO2气氛下用100μL DMEM培养基或RPMI 1640培养基培养过夜24小时。然后,去除原始培养基,将测试细胞分别与含有游离DOX、游离VCR/长春新碱/Vincristine、游离(DOX加VCR)的新鲜培养基一起孵育,CS-ALG@TPGS-PLGA-VCRNP,CS-ALG-DOX@TPGS-PLGANP,以及CS-ALG-DOX@TPGS-PLGA-VCR不同浓度的NP。孵育12小时和24小时后,向每个孔中加入10μL WST-1溶液并再培养4小时。然后,通过使用酶标仪测量450nm处的吸光度来确定细胞存活率。 微管和微丝成像分析[6] 将A549细胞或A549/紫杉醇细胞接种在6孔板(1×105个细胞/孔)的盖玻片上,并在37°C的5%CO2培养箱中孵育过夜以进行附着。然后,分别用TPGS-PLGA(0.2 mg/mL)NP、游离VCR/长春新碱(5μg/mL)和TPGS-PLGA-VCR NP(5μg/mL VCR负载NP)在37°C下洗涤细胞并培养给定时间。未经处理的细胞用作对照组。用PBS洗涤测试细胞,用Hoechst 33342(10mg/mL)处理20分钟。随后,在室温下用4%多聚甲醛固定细胞10分钟,用含0.1%吐温-20(PBST)的磷酸缓冲盐水中的1%BSA渗透1小时。 然后将细胞在4°C的暗室中暴露于微管蛋白跟踪器红色(1:250,稀释于含有1%BSA的PBST中,用于微管)或肌动蛋白跟踪器绿色(8单位/mL,稀释于含1%BSA的PBT中,用于微丝)20分钟。然后,去除含有微管蛋白跟踪器红色或肌动蛋白跟踪器绿色的原始培养基,用冰冷的PBS洗涤细胞。最后,在CLSM下观察细胞的微管或微丝。 细胞周期分析[6] 用细胞周期和凋亡分析试剂盒评估空NP、游离VCR/Vincristine/长春新碱和载药NP在A549/紫杉醇细胞上诱导的细胞周期。在37°C下,将细胞以每孔5×105个细胞的密度接种在6孔板上24小时,然后分别用含有TPGS-PLGA NP(0.2 mg/mL)、游离VCR(5μg/mL)和TPGS-PLGA-VCR NP(VCR剂量5μg/mL)的新鲜培养基处理。未经处理的细胞用作对照。孵育24小时后,通过胰蛋白酶消化和离心收集细胞。随后,将获得的细胞用70%冷乙醇固定,并在4°C下储存24小时。最终,再次离心细胞,用冷PBS洗涤两次,并在黑暗中用0.5mL 37°C的染色溶液染色30分钟。使用流式细胞仪系统 分析染色的细胞。每个实验进行三次。 |
||
| 动物实验 |
|
||
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
The liver is the major excretory organ in humans and animals. 80% of an injected dose of vincristine sulfate is excreted via feces. 10 - 20% is excreted via urine. Within 15 to 30 minutes after injection, over 90% of the drug is distributed from the blood into tissue, where it remains tightly, but not irreversibly, bound. Development of CNS leukemia in patients receiving vincristine and in hematological remission has been interpreted as evidence that ... /vincristine/ penetrates blood-brain barrier poorly. Vincristine ... can be infused into arterial blood supply of tumors in doses several times larger than those that can be admistered iv with comparable toxicity; thus either local uptake or destruction is very rapid. Vinca alkaloids appear to be excreted primarily by liver into bile. Urinary excretion ... over first few hr after injection was ... low in dogs and monkeys. In both ... the drug was distributed to most tissues, but highest concentrations ... found in lung, kidney, spleen, pancreas and liver. In monkeys, vincristine and its metabolites rapidly entered cerebrospinal fluid from plasma to form low concentrations of drug, which persisted for several days. Vincristine sulfate is unpredictably absorbed from the Gl tract. Following rapid iv injection of a 2 mg dose of vincristine in patients with normal renal and hepatic function, peak serum drug concentrations of approximately 0.19-0.89 uM occur immediately and the drug is rapidly cleared from serum. The area under the serum vincristine concentration time curve has been shown to be increased following continuous iv infusion compared with rapid iv injection of the drug when comparable doses are administered. Distribution of vincristine and its metabolites (and/or decomposition products) into human body tissues and fluids has not been fully characterized, but the drug is rapidly and apparently widely distributed following iv administration. Drug that is distributed into tissues is tightly but reversibly bound. Vincristine and its metabolites (and/or decomposition products) are rapidly and extensively distributed into bile, with peak biliary concentrations occurring within 2-4 hr after rapid iv injection of the drug. Vincristine and its metabolites (and/or decomposition products) cross the blood brain barrier poorly following rapid iv injection and generally do not appear in the CSF in cytotoxic concentrations. For more Absorption, Distribution and Excretion (Complete) data for VINCRISTINE (6 total), please visit the HSDB record page. Metabolism / Metabolites Hepatic. Cytochrome P450 isoenzymes of the CYP3A subfamily facilitate the metabolism of vincristine. After iv administration of ... (3)H vincristine, 69% of radioactivity was recovered in feces and 12% in urine over 72 hr period. Approx half ... was in form of metabolites, whose UV spectrum suggested that vincristine dimer was intact. Patients with biliary fistula showed extensive biliary excretion of intact drug (46.5%) & of metabolites (53.5%). Observations suggest that biliary-fecal route ... predominate in excretion ... . The metabolic fate of vincristine has not been clearly determined; the drug appears to be extensively metabolized, probably in the liver, but the extent of metabolism is not clear since the drug also apparently undergoes decomposition in vivo. Hepatic. Cytochrome P450 isoenzymes of the CYP3A subfamily facilitate the metabolism of vincristine. Route of Elimination: The liver is the major excretory organ in humans and animals. 80% of an injected dose of vincristine sulfate is excreted via feces. 10 - 20% is excreted via urine. Half Life: When intravenously injected into cancer patients, a triphasic serum decay patten was observed. The initial, middle, and terminal half-lives are 5 minutes, 2.3 hours, 85 hours respectively. The range of the terminal half-life is humans is 19 - 155 hours. Biological Half-Life When intravenously injected into cancer patients, a triphasic serum decay patten was observed. The initial, middle, and terminal half-lives are 5 minutes, 2.3 hours, 85 hours respectively. The range of the terminal half-life is humans is 19 - 155 hours. After iv administration of ... (3)H vincristine, triphasic decay was observed, with half-lives of 0.85, 7.4 and 164 min ... Following rapid iv injection of vincristine, serum concentrations of the drug appear to decline in a triphasic manner. The terminal elimination half-life of vincristine has ranged from 19-155 hr. |
||
| 毒性/毒理 (Toxicokinetics/TK) |
Effects During Pregnancy and Lactation
◉ Summary of Use during Lactation Most sources consider breastfeeding to be contraindicated during maternal antineoplastic drug therapy. It is probably impractical to resume breastfeeding after vincristine therapy because of the drug's long half-life. Chemotherapy may adversely affect the normal microbiome and chemical makeup of breastmilk. ◉ Effects in Breastfed Infants In a 4-month-old, neutropenia was probably caused by cyclophosphamide in a mother 9 days after the last of 6 weekly doses of 800 mg cyclophosphamide intravenously, 2 mg vincristine intravenously and daily doses of 30 mg of prednisolone orally. Neutropenia persisted at least 12 days and was accompanied by a brief episode of diarrhea. The contribution of vincristine to the neutropenia cannot be determined. A woman was diagnosed with B-cell lymphoma at 27 weeks of pregnancy. Labor was induced at 34 4/7 weeks and treatment was begun with a standard regimen of rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone in unspecified doses on a 21-day cycle, starting on day 2 postpartum. She pumped and discarded her milk and fed her infant donor milk for the first 10 days of each cycle and then breastfed her infant for the remaining 10 days before the next treatment cycle. The 10-day period of breastfeeding abstinence was determined by using about 3 half-lives of vincristine. After completion of 4 cycles of chemotherapy, her infant was reportedly healthy and developing without any complications. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding ~75% |
||
| 参考文献 | |||
| 其他信息 |
Vincristine Sulfate can cause developmental toxicity according to state or federal government labeling requirements.
Vincristine sulfate appears as an anticancer drug. White to slightly yellow, amorphous or crystalline powder. Sensitive to light. Odorless. pH (0.1% solution) 3.5 - 4.5. (NTP, 1992) Vincristine Sulfate is the sulfate salt of a natural alkaloid isolated from the plant Catharanthus roseus (Vinca rosea L.) with antimitotic and antineoplastic activities. Vincristine binds irreversibly to microtubules and spindle proteins in S phase of the cell cycle and interferes with the formation of the mitotic spindle, thereby arresting tumor cells in metaphase. This agent also depolymerizes microtubules and may also interfere with amino acid, cyclic AMP, and glutathione metabolism; calmodulin-dependent Ca(2+)-activated ATPase activity; cellular respiration; and nucleic acid and lipid biosynthesis. Vincristine Sulfate Liposome is a sphingomyelin/cholesterol liposomal formulation of vincristine sulfate with potential antineoplastic activity. Vincristine, a vinca alkaloid isolated from the plant Vinca rosea, irreversibly binds to and stabilizes tubulin, thereby interrupting microtubule assembly/disassembly dynamics, thereby preventing the formation of the mitotic spindle and leading to cell cycle arrest in metaphase. Liposomal encapsulation prolongs bioavailability of vincristine, increases its delivery to tumor tissues and reduces its toxicity profile. Compared to standard liposomal delivery, sphingosomal drug delivery further increases circulation time of serum drug and enhances drug accumulation at tumor sites, thereby leading to a further increase in efficacy. An antitumor alkaloid isolated from VINCA ROSEA. (Merck, 11th ed.) See also: Vincristine (has active moiety). Vinblastine or colchicine, administered intraperitoneally to B6D2F1 mice with advanced subcutaneous colon 38 tumours, induced substantial tumour growth delays with progressive development of haemorrhagic necrosis beginning within 8 hours of treatment. Two multidrug-resistant P388 leukaemia sublines, refractory to vinblastine and vincristine when grown as intraperitoneal ascites, were sensitive to necrosis induction when grown as subcutaneous tumours. Vascular labelling with two fluorescent markers indicated that vincristine substantially reduced tumour blood flow within 4 hours after treatment. The effects of vinblastine, vincristine and colchicine were similar to those of tumour necrosis factor alpha in that: (a) similar tumour necrosis and blood flow changes were induced, (b) coadministration of the serotonin antagonist cyproheptidine prevented tumour necrosis and (c) plasma nitrate levels were elevated, indicative of the stimulation of oxidation of L-arginine to nitric oxide. The results suggest that vinca alkaloids and colchicine act on solid tumours by host cell-mediated vascular effects as well as by direct tubulin-mediated cytotoxicity.[5] Combination chemotherapy in clinical practice has been generally accepted as a feasible strategy for overcoming multidrug resistance (MDR). Here, we designed and successfully prepared a co-delivery system named S-D1@L-D2 NPs, where denoted some smaller nanoparticles (NPs) carrying a drug doxorubicin (DOX) were loaded into a larger NP containing another drug (vincristine [VCR]) via water-in-oil-in-water double-emulsion solvent diffusion-evaporation method. Chitosan-alginate nanoparticles carrying DOX (CS-ALG-DOX NPs) with a smaller diameter of about 20 nm formed S-D1 NPs; vitamin E D-α-tocopheryl polyethylene glycol 1000 succinate-modified poly(lactic-co-glycolic acid) nanoparticles carrying VCR (TPGS-PLGA-VCR NPs) with a larger diameter of about 200 nm constituted L-D2 NPs. Some CS-ALG-DOX NPs loaded into TPGS-PLGA-VCR NPs formed CS-ALG-DOX@TPGS-PLGA-VCR NPs. Under the acidic environment of cytosol and endosome or lysosome in MDR cell, CS-ALG-DOX@TPGS-PLGA-VCR NPs released VCR and CS-ALG-DOX NPs. VCR could arrest cell cycles at metaphase by inhibiting microtubule polymerization in the cytoplasm. After CS-ALG-DOX NPs escaped from endosome, they entered the nucleus through the nuclear pore and released DOX in the intra-nuclear alkaline environment, which interacted with DNA to stop the replication of MDR cells. These results indicated that S-D1@L-D2 NPs was a co-delivery system of intracellular precision release loaded drugs with pH-sensitive characteristics. S-D1@L-D2 NPs could obviously enhance the in vitro cytotoxicity and the in vivo anticancer efficiency of co-delivery drugs, while reducing their adverse effects. Overall, S-D1@L-D2 NPs can be considered an innovative platform for the co-delivery drugs of clinical combination chemotherapy for the treatment of MDR tumor. [6] Background Combination therapy is a key strategy for minimizing drug resistance, a common problem in cancer therapy. The microtubule-depolymerizing agent vincristine is widely used in the treatment of acute leukemia. In order to decrease toxicity and chemoresistance of vincristine, this study will investigate the effects of combination vincristine and vorinostat (suberoylanilide hydroxamic acid (SAHA)), a pan-histone deacetylase inhibitor, on human acute T cell lymphoblastic leukemia cells. Methods Cell viability experiments were determined by 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide (MTT) assay, and cell cycle distributions as well as mitochondria membrane potential were analyzed by flow cytometry. In vitro tubulin polymerization assay was used to test tubulin assembly, and immunofluorescence analysis was performed to detect microtubule distribution and morphology. In vivo effect of the combination was evaluated by a MOLT-4 xenograft model. Statistical analysis was assessed by Bonferroni’s t test. Results Cell viability showed that the combination of vincristine and SAHA exhibited greater cytotoxicity with an IC50 value of 0.88 nM, compared to each drug alone, 3.3 and 840 nM. This combination synergically induced G2/M arrest, followed by an increase in cell number at the sub-G1 phase and caspase activation. Moreover, the results of vincristine combined with an HDAC6 inhibitor (tubastatin A), which acetylated α-tubulin, were consistent with the effects of vincristine/SAHA co-treatment, thus suggesting that SAHA may alter microtubule dynamics through HDAC6 inhibition. Conclusion These findings indicate that the combination of vincristine and SAHA on T cell leukemic cells resulted in a change in microtubule dynamics contributing to M phase arrest followed by induction of the apoptotic pathway. These data suggest that the combination effect of vincristine/SAHA could have an important preclinical basis for future clinical trial testing.[7] In our study, SA1 mechanoreceptors were impaired by acutely exposing dissociated whisker hair follicles to vincristine in vitro. On the other hand, whisker tactile behavioral responses were impaired days after the in vivo vincristine treatment regimen. The delayed impairment of the sensory behavioral responses could be due to slow accumulation of vincristine in whisker hair follicles during the in vivo vincristine treatment. In addition, SA1 mechanoreceptors or Merkel discs are located deep in hair follicles and shielded by a layer of glassy membranes, which may not favor the diffusion of vincristine into Merkel disc regions during the in vivo vincristine treatment. Alternatively, whisker tactile responses may be compensated by RA and SA2 when the impairment of SA1 mechanoreceptors by vincristine was not very severe in the early stage of the in vivo vincristine treatment. Although the in vivo vincristine treatment regimen used in the present study did not impair RA and SA2 mechanoreceptors, it will be interesting to examine whether a prolonged in vivo vincristine treatment may eventually impair these two mechanoreceptors as well. It will also be interesting to examine whether and how long the vincristine-induced impairment of mechanoreceptors can be recovered following the termination of a vincristine treatment regimen.[8] |
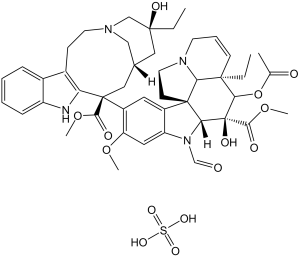
| 分子式 |
C46H58N4O14S
|
|---|---|
| 分子量 |
923.04
|
| 精确质量 |
922.367
|
| 元素分析 |
C, 66.97; H, 6.84; N, 6.79; O, 19.39
|
| CAS号 |
2068-78-2
|
| 相关CAS号 |
57-22-7; 2068-78-2 (sulfate); Vincristine-d3-ester sulfate;1217854-24-4;Vincristine-d3 sulfate;1246817-10-6;Vincristine-d6 sulfate
|
| PubChem CID |
249332
|
| 外观&性状 |
White to off-white solid powder
|
| 沸点 |
273-281 °C
|
| 熔点 |
300 °C
|
| LogP |
4.522
|
| tPSA |
254.15
|
| 氢键供体(HBD)数目 |
5
|
| 氢键受体(HBA)数目 |
16
|
| 可旋转键数目(RBC) |
10
|
| 重原子数目 |
65
|
| 分子复杂度/Complexity |
1830
|
| 定义原子立体中心数目 |
9
|
| SMILES |
CC[C@@]1(C[C@@H]2C[C@@](C3=C(CCN(C2)C1)C4=CC=CC=C4N3)(C5=C(C=C6C(=C5)[C@]78CCN9[C@H]7[C@@](C=CC9)([C@H]([C@@]([C@@H]8N6C=O)(C(=O)OC)O)OC(=O)C)CC)OC)C(=O)OC)O.OS(=O)(=O)O
|
| InChi Key |
AQTQHPDCURKLKT-JKDPCDLQSA-N
|
| InChi Code |
InChI=1S/C46H56N4O10.H2O4S/c1-7-42(55)22-28-23-45(40(53)58-5,36-30(14-18-48(24-28)25-42)29-12-9-10-13-33(29)47-36)32-20-31-34(21-35(32)57-4)50(26-51)38-44(31)16-19-49-17-11-15-43(8-2,37(44)49)39(60-27(3)52)46(38,56)41(54)59-6;1-5(2,3)4/h9-13,15,20-21,26,28,37-39,47,55-56H,7-8,14,16-19,22-25H2,1-6H3;(H2,1,2,3,4)/t28-,37+,38-,39-,42+,43-,44-,45+,46+;/m1./s1
|
| 化学名 |
(3aR,3a1R,4R,5S,5aR,10bR)-methyl 4-acetoxy-3a-ethyl-9-((3S,5S,7S,9S)-5-ethyl-5-hydroxy-9-(methoxycarbonyl)-2,4,5,6,7,8,9,10-octahydro-1H-3,7-methano[1]azacycloundecino[5,4-b]indol-9-yl)-6-formyl-5-hydroxy-8-methoxy-3a,3a1,4,5,5a,6,11,12-octahydro-1H-indolizino[8,1-cd]carbazole-5-carboxylate sulfate.
|
| 别名 |
Leurocristine; NSC-67574 sulfate; 22-Oxovincaleukoblastine sulfate; leurocristine sulfate; NSC67574; NSC 67574; Vincristine sulfate; 2068-78-2; Kyocristine; Vincristine sulphate; Vincrisul; Oncovin; Novopharm; Leurocristine sulfate; Vincasar PFS; Oncovin; VCR
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中(例如氮气保护),避免吸湿/受潮和光照。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.08 mg/mL (2.25 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 20.8 mg/mL澄清DMSO储备液加入400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.08 mg/mL (2.25 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 20.8 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.08 mg/mL (2.25 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 配方 4 中的溶解度: Saline:30 mg/mL 配方 5 中的溶解度: 100 mg/mL (108.34 mM) in PBS (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液; 超声助溶 (<60°C). 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.0834 mL | 5.4169 mL | 10.8338 mL | |
| 5 mM | 0.2167 mL | 1.0834 mL | 2.1668 mL | |
| 10 mM | 0.1083 mL | 0.5417 mL | 1.0834 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
Testing CC-486 (Oral Azacitidine) Plus the Standard Drug Therapy in Patients 75 Years or Older With Newly Diagnosed Diffuse Large B Cell Lymphoma
CTID: NCT04799275
Phase: Phase 2/Phase 3 Status: Recruiting
Date: 2024-11-27