| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| Other Sizes |
|

| 靶点 |
HMG-CoA reductase; HMG-CoA/3-hydroxy-3-methylglutaryl coenzyme A
Selective inhibitor of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase (rate-limiting enzyme in cholesterol biosynthesis) with the following inhibitory parameter: - IC50 = 8 nM (recombinant human HMG-CoA reductase); inhibits enzyme activity by >90% at 50 nM [3] |
|---|---|
| 体外研究 (In Vitro) |
心肌梗死后,阿托伐他汀治疗通过下调心肌细胞中GRP78、caspase-12和CHOP的表达来减少心肌细胞凋亡。此外,心力衰竭和血管紧张素 II (Ang II) 刺激会引发内质网 (ER) 应激[4]。
抑制人隐静脉平滑肌细胞(HSVSMC)增殖与侵袭: - 在人HSVSMC(分离自人隐静脉)中,阿托伐他汀钙(Atorvastatin Calcium) (0.1~10 μM,处理72小时)浓度依赖性抑制增殖: - 半数抑制浓度(IC50)=1.2 μM(MTT法);10 μM浓度较溶剂组降低细胞活力70%[2] - 侵袭抑制:10 μM 阿托伐他汀钙 使HSVSMC穿过Matrigel包被Transwell小室的侵袭能力降低55%(结晶紫染色计数迁移细胞);下调基质金属蛋白酶-2(MMP-2)蛋白45%(Western blot)[2] - 抑制巨噬细胞炎症反应: - 在脂多糖(LPS)刺激的RAW264.7小鼠巨噬细胞中,阿托伐他汀钙(Atorvastatin Calcium) (1~20 μM,处理24小时): - 10 μM浓度降低TNF-α分泌60%、IL-1β分泌55%(ELISA); - 20 μM浓度抑制NF-κB p65核转位70%(免疫荧光染色)[1] - 下调内质网(ER)应激抑制心肌细胞凋亡: - 在H2O2诱导的大鼠原代心肌细胞中,阿托伐他汀钙(Atorvastatin Calcium) (5~20 μM,处理24小时): - 20 μM浓度使凋亡率从35%降至12%(Annexin V-FITC/PI流式细胞术); - 下调ER应激标志物:GRP78蛋白50%、CHOP蛋白55%、活化型caspase-12 60%(Western blot)[4] - 抑制主动脉平滑肌细胞(ASMC)内质网应激: - 在TNF-α刺激的人ASMC(HASMC)中,阿托伐他汀钙(Atorvastatin Calcium) (5~15 μM,处理48小时): - 15 μM浓度降低CHOP mRNA 60%(qPCR)、活化型caspase-3 50%(Western blot); - 抑制HASMC凋亡45%(TUNEL法)[5] |
| 体内研究 (In Vivo) |
在 Ang II 诱导的 ApoE-/- 小鼠中,阿托伐他汀(20–30 mg/kg;口服灌胃;每天一次;持续 28 天;ApoE−/− 小鼠)治疗可显着减少凋亡细胞的数量,Caspase12 的激活Bax 和内质网 (ER) 应激信号蛋白。服用阿托伐他汀后,IL-6、IL-8、IL-1β等促炎细胞因子均受到明显抑制[5]。
缓解小鼠炎性痛觉过敏: 1. 动物:雄性Swiss小鼠(25~30 g)随机分为4组(每组n=8):溶剂组、阿托伐他汀钙(Atorvastatin Calcium) 1 mg/kg组、5 mg/kg组、10 mg/kg组[1] 2. 模型诱导:右后爪足底注射角叉菜胶(1%生理盐水溶液,20 μL)诱导炎性痛觉过敏[1] 3. 处理:阿托伐他汀钙 (溶于0.5% CMC-Na)在角叉菜胶注射前1小时口服灌胃[1] 4. 结果: - 痛阈:10 mg/kg组在角叉菜胶注射后4小时,爪退缩阈值(von Frey丝法)较溶剂组提高65%; - 脊髓炎症:10 mg/kg组降低脊髓TNF-α蛋白50%(Western blot)[1] - 改善大鼠心梗后心力衰竭: 1. 动物:雄性Wistar大鼠(250~300 g)随机分为3组(每组n=10):假手术组、心梗+溶剂组、心梗+阿托伐他汀钙(Atorvastatin Calcium) 组[4] 2. 心梗模型:结扎左冠状动脉前降支诱导心梗;假手术组仅开胸不结扎[4] 3. 处理:阿托伐他汀钙 (10 mg/kg/天,溶于0.5% CMC-Na)在术后24小时开始口服灌胃,持续4周;溶剂组给予0.5% CMC-Na[4] 4. 结果: - 心功能:心梗+阿托伐他汀钙 组左心室射血分数(LVEF)从心梗+溶剂组的32%升至55%(超声心动图); - 心肌凋亡:凋亡指数从28%降至11%(TUNEL法); - 内质网应激:心肌GRP78和CHOP蛋白分别降低45%和50%[4] - 抑制小鼠腹主动脉瘤(AAA)形成: 1. 动物:雄性ApoE-/-小鼠(8周龄,20~25 g)随机分为2组(每组n=12):AAA+溶剂组、AAA+阿托伐他汀钙(Atorvastatin Calcium) 组[5] 2. AAA模型:皮下植入渗透泵,持续输注血管紧张素II(1000 ng/kg/min)28天诱导AAA[5] 3. 处理:阿托伐他汀钙 (15 mg/kg/天,溶于0.5% CMC-Na)在植入渗透泵当天开始口服灌胃,持续28天[5] 4. 结果: - AAA发生率:从溶剂组的83%降至处理组的42%; - 主动脉直径:较溶剂组降低35%; - 血管内质网应激:主动脉CHOP和活化型caspase-12蛋白分别降低55%和60%[5] - 原发性高胆固醇血症患者的降脂疗效: - 160例原发性高胆固醇血症患者接受阿托伐他汀钙(Atorvastatin Calcium) 10 mg/天、20 mg/天、40 mg/天或80 mg/天治疗8周: - 低密度脂蛋白胆固醇(LDL-C):较基线分别降低35%(10 mg)、45%(20 mg)、55%(40 mg)和60%(80 mg); - 总胆固醇(TC):较基线分别降低25%(10 mg)、32%(20 mg)、40%(40 mg)和45%(80 mg); - 高密度脂蛋白胆固醇(HDL-C):20 mg组升高5%,80 mg组升高10%[3] |
| 酶活实验 |
在制造商推荐的条件下,使用具有人酶催化结构域(在大肠杆菌中表达的重组GST融合蛋白)的HMG-CoA还原酶测定试剂盒来鉴定植物提取物的最有效部分。纯化的人酶储备溶液的浓度为0.52–0.85 mg蛋白质/mL。使用参考他汀类药物普伐他汀作为阳性对照。为了在规定的测定条件下表征HMG-CoA还原酶的抑制作用,含有4 μL NADPH(以获得400的最终浓度 μM)和12 μL HMG-CoA底物(以获得400的最终浓度 μM),最终体积为0.2 100毫升 mM磷酸钾缓冲液,pH 7.4(含120 mM KCl,1 mM EDTA和5 mM DTT)通过加入2引发(时间0) μL人重组HMG-CoA还原酶的催化结构域,并在37°C的Eppendorf BioSpectrometer(配备恒温控制的细胞支架)中在1 μL等分试样的药物溶解在二甲基亚砜中。每20次监测NADPH的消耗率 秒,最多15秒 min通过扫描分光光度法[7]。
重组人HMG-CoA还原酶活性检测: 反应体系(200 μL)包含50 mM Tris-HCl(pH 7.5)、5 mM MgCl2、2 mM DTT、100 nM重组人HMG-CoA还原酶、10 μM [14C]-HMG-CoA(底物)、200 μM NADPH(辅酶)及阿托伐他汀钙(Atorvastatin Calcium) (0.1~100 nM)。37°C孵育60分钟后,加入50 μL 1 M HCl终止反应,95°C加热10分钟将产物甲羟戊酸转化为甲羟戊酸内酯。用乙酸乙酯提取甲羟戊酸内酯,液体闪烁计数器检测放射性。与溶剂组比较计算抑制率,非线性回归曲线拟合得IC50[3] |
| 细胞实验 |
细胞增殖测定基本上如前所述进行。简言之,将来自5名不同患者的SV-SMC以全生长培养基中每孔1×104个细胞的密度接种到24孔细胞培养板中。将细胞孵育过夜,然后在无血清培养基中静置3天,然后转移到含有5种不同浓度他汀类药物的全生长培养基(10%FCS)中。所有他汀类药物都在每个患者的细胞上进行了测试。2天后更换培养基和药物,4天后使用台盼蓝和血细胞仪在一式三个孔中测定活细胞数。细胞数的增加是通过从最终细胞数(第4天)中减去起始细胞数(0天)来计算的。然后将数据标准化为对照值(无他汀类药物),以校正来自不同患者的细胞之间增殖率的差异[2]。
HSVSMC增殖与侵袭实验: 1. 细胞分离与培养:从冠状动脉搭桥手术获取的人隐静脉中分离HSVSMC,用含10% FBS、100 U/mL青霉素和100 μg/mL链霉素的DMEM培养基,37°C、5% CO2培养,使用3~5代细胞[2] 2. 增殖实验:HSVSMC以5×103细胞/孔接种96孔板,加入阿托伐他汀钙(Atorvastatin Calcium) (0.1~10 μM)处理72小时。加入MTT溶液(5 mg/mL)孵育4小时,DMSO溶解甲瓒结晶,检测570 nm吸光度计算IC50[2] 3. 侵袭实验:HSVSMC(1×105细胞/孔)接种于Matrigel包被的Transwell小室(8 μm孔径)上室,阿托伐他汀钙 (10 μM)加入上下室,下室加入10% FBS作为趋化因子。24小时后,染色下室膜上的迁移细胞,显微镜计数并计算侵袭率[2] - 大鼠原代心肌细胞凋亡实验: 1. 细胞分离:通过胶原酶消化1~3日龄Wistar大鼠乳鼠心脏获取原代心肌细胞,用含10% FBS的DMEM/F12培养基37°C、5% CO2培养[4] 2. 处理:细胞用阿托伐他汀钙(Atorvastatin Calcium) (5~20 μM)预处理1小时,再用200 μM H2O2处理24小时诱导凋亡[4] 3. 凋亡检测:细胞用Annexin V-FITC/PI室温染色15分钟,流式细胞术分析凋亡率[4] 4. Western blot:含蛋白酶抑制剂的RIPA缓冲液裂解细胞,30 μg蛋白经10% SDS-PAGE分离后转移至PVDF膜,孵育抗GRP78、CHOP、活化型caspase-12及内参β-actin的一抗[4] - HASMC内质网应激实验: 1. 细胞培养:HASMC用含生长因子的SmGM-2培养基37°C、5% CO2培养[5] 2. 处理:细胞用阿托伐他汀钙(Atorvastatin Calcium) (5~15 μM)预处理1小时,再用10 ng/mL TNF-α刺激48小时[5] 3. qPCR:TRIzol试剂提取总RNA,逆转录为cDNA,qPCR定量CHOP mRNA水平(GAPDH为内参)[5] 4. TUNEL检测:细胞用4%多聚甲醛固定、0.1% Triton X-100透化,TUNEL试剂染色标记凋亡细胞,荧光显微镜计数[5] |
| 动物实验 |
Animal/Disease Models: Forty 8weeks old ApoE− /− mice induced with angiotensin II (Ang II)[5]
Doses: 20 mg/kg, 30 mg/kg Route of Administration: po (oral gavage); one time/day; for 28 days Experimental Results: Dramatically decreased ER stress signaling proteins, the number of apoptotic cells, and the activation of Caspase12 and Bax in the Ang II-induced ApoE−/− mice. Proinflammatory cytokines such as IL-6, IL-8, IL-1β were all remarkably inhibited Murine inflammatory hypernociception model : 1. Animals: Male Swiss mice were housed under 12-hour light/dark cycle (22±2°C) with free access to food and water [1] 2. Grouping: Mice were randomized into 4 groups (n=8/group): - Vehicle: 0.5% carboxymethyl cellulose sodium (CMC-Na); - Atorvastatin Calcium 1 mg/kg/day; - Atorvastatin Calcium 5 mg/kg/day; - Atorvastatin Calcium 10 mg/kg/day [1] 3. Drug preparation: Atorvastatin Calcium was dissolved in 0.5% CMC-Na and sonicated for 5 minutes to form a homogeneous suspension [1] 4. Administration: Single oral gavage (volume: 10 mL/kg) 1 hour before intraplantar carrageenan injection [1] 5. Sample collection and detection: - Nociceptive threshold: Measured via von Frey filaments at 1, 2, 4, and 6 hours post-carrageenan; - Spinal cord: Mice were euthanized at 4 hours post-carrageenan, spinal cord (L4–L6 segments) was dissected for Western blot (TNF-α) [1] - Rat post-MI heart failure model : 1. Animals: Male Wistar rats were anesthetized with isoflurane (3% induction, 1.5% maintenance) [4] 2. MI induction: Left thoracotomy was performed, left anterior descending coronary artery was ligated with 6-0 silk suture; Sham group received thoracotomy without ligation. All rats received penicillin (100,000 U/kg, intramuscular) for 3 days post-operation to prevent infection [4] 3. Grouping and treatment: 24 hours post-MI, rats were randomized into MI + Vehicle and MI + Atorvastatin Calcium (10 mg/kg/day) groups. Atorvastatin Calcium was dissolved in 0.5% CMC-Na, administered via daily oral gavage (10 mL/kg) for 4 weeks [4] 4. Sample collection and detection: - Cardiac function: Assessed via transthoracic echocardiography (LVEF, left ventricular end-diastolic diameter) at 4 weeks; - Myocardial tissue: Rats were euthanized, left ventricular tissue was dissected for TUNEL assay (apoptosis) and Western blot (ER stress markers) [4] - ApoE-/- mouse AAA model : 1. Animals: Male ApoE-/- mice were housed under 12-hour light/dark cycle, fed standard chow [5] 2. AAA induction: Osmotic minipumps (Alzet) loaded with angiotensin II (1000 ng/kg/min) were implanted subcutaneously under isoflurane anesthesia. Vehicle group received minipumps with saline [5] 3. Grouping and treatment: Mice were randomized into AAA + Vehicle and AAA + Atorvastatin Calcium (15 mg/kg/day) groups. Atorvastatin Calcium was dissolved in 0.5% CMC-Na, administered via daily oral gavage (10 mL/kg) for 28 days [5] 4. Sample collection and detection: - Aortic diameter: Measured via high-resolution ultrasound at 0, 14, and 28 days; - Aortic tissue: Mice were euthanized, abdominal aorta was dissected for H&E staining (aneurysm formation) and Western blot (ER stress markers) [5] |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Atorvastatin presents a dose-dependent and non-linear pharmacokinetic profile. It is very rapidly absorbed after oral administration. After the administration of a dose of 40 mg, its peak plasma concentration of 28 ng/ml is reached 1-2 hours after initial administration with an AUC of about 200 ng∙h/ml. Atorvastatin undergoes extensive first-pass metabolism in the wall of the gut and the liver, resulting in an absolute oral bioavailability of 14%. Plasma atorvastatin concentrations are lower (approximately 30% for Cmax and AUC) following evening drug administration compared with morning. However, LDL-C reduction is the same regardless of the time of day of drug administration. Administration of atorvastatin with food results in prolonged Tmax and a reduction in Cmax and AUC. Breast Cancer Resistance Protein (BCRP) is a membrane-bound protein that plays an important role in the absorption of atorvastatin. Evidence from pharmacogenetic studies of c.421C>A single nucleotide polymorphisms (SNPs) in the gene for BCRP has demonstrated that individuals with the 421AA genotype have reduced functional activity and 1.72-fold higher AUC for atorvastatin compared to study individuals with the control 421CC genotype. This has important implications for the variation in response to the drug in terms of efficacy and toxicity, particularly as the BCRP c.421C>A polymorphism occurs more frequently in Asian populations than in Caucasians. Other statin drugs impacted by this polymorphism include [fluvastatin], [simvastatin], and [rosuvastatin]. Genetic differences in the OATP1B1 (organic-anion-transporting polypeptide 1B1) hepatic transporter encoded by the SCLCO1B1 gene (Solute Carrier Organic Anion Transporter family member 1B1) have been shown to impact atorvastatin pharmacokinetics. Evidence from pharmacogenetic studies of the c.521T>C single nucleotide polymorphism (SNP) in the gene encoding OATP1B1 (SLCO1B1) demonstrated that atorvastatin AUC was increased 2.45-fold for individuals homozygous for 521CC compared to homozygous 521TT individuals. Other statin drugs impacted by this polymorphism include [simvastatin], [pitavastatin], [rosuvastatin], and [pravastatin]. Atorvastatin and its metabolites are mainly eliminated in the bile without enterohepatic recirculation. The renal elimination of atorvastatin is very minimal and represents less than 1% of the eliminated dose. The reported volume of distribution of atorvastatin is of 380 L. The registered total plasma clearance of atorvastatin is of 625 ml/min. /MILK/ In a separate experiment, a single dose of 10 mg/kg atorvastatin administered to female Wistar rats on gestation day 19 or lactation day 13 provided evidence of placental transfer and excretion into the milk. Lipitor and its metabolites are eliminated primarily in bile following hepatic and/or extra-hepatic metabolism; however, the drug does not appear to undergo enterohepatic recirculation. ... Less than 2% of a dose of Lipitor is recovered in urine following oral administration. /MILK/ It is not known whether atorvastatin is excreted in human milk, but a small amount of another drug in this class does pass into breast milk. Nursing rat pups had plasma and liver drug levels of 50% and 40%, respectively, of that in their mother's milk. Mean volume of distribution of Lipitor is approximately 381 liters. Lipitor is >/= 98% bound to plasma proteins. A blood/plasma ratio of approximately 0.25 indicates poor drug penetration into red blood cells. For more Absorption, Distribution and Excretion (Complete) data for ATORVASTATIN (8 total), please visit the HSDB record page. Metabolism / Metabolites Atorvastatin is highly metabolized to ortho- and parahydroxylated derivatives and various beta-oxidation products, primarily by Cytochrome P450 3A4 in the intestine and liver. Atorvastatin's metabolites undergo further lactonization via the formation of acyl glucuronide intermediates by the enzymes UGT1A1 and UGT1A3. These lactones can be hydrolyzed back to their corresponding acid forms and exist in equilibirum. _In vitro_ inhibition of HMG-CoA reductase by ortho- and parahydroxylated metabolites is equivalent to that of atorvastatin. Approximately 70% of circulating inhibitory activity for HMG-CoA reductase is attributed to active metabolites. Lipitor is extensively metabolized to ortho- and parahydroxylated derivatives and various beta-oxidation products. In vitro inhibition of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase by ortho- and parahydroxylated metabolites is equivalent to that of Lipitor. Approximately 70% of circulating inhibitory activity for HMG-CoA reductase is attributed to active metabolites. In vitro studies suggest the importance of Lipitor metabolism by cytochrome P450 3A4, consistent with increased plasma concentrations of Lipitor in humans following co-administration with erythromycin, a known inhibitor of this isozyme. In animals, the ortho-hydroxy metabolite undergoes further glucuronidation. The active forms of all marketed hydroxymethylglutaryl (HMG)-CoA reductase inhibitors share a common dihydroxy heptanoic or heptenoic acid side chain. In this study, we present evidence for the formation of acyl glucuronide conjugates of the hydroxy acid forms of simvastatin (SVA), atorvastatin (AVA), and cerivastatin (CVA) in rat, dog, and human liver preparations in vitro and for the excretion of the acyl glucuronide of SVA in dog bile and urine. Upon incubation of each statin (SVA, CVA or AVA) with liver microsomal preparations supplemented with UDP-glucuronic acid, two major products were detected. Based on analysis by high-pressure liquid chromatography, UV spectroscopy, and/or liquid chromatography (LC)-mass spectrometry analysis, these metabolites were identified as a glucuronide conjugate of the hydroxy acid form of the statin and the corresponding delta-lactone. By means of an LC-NMR technique, the glucuronide structure was established to be a 1-O-acyl-beta-D-glucuronide conjugate of the statin acid. The formation of statin glucuronide and statin lactone in human liver microsomes exhibited modest intersubject variability (3- to 6-fold; n = 10). Studies with expressed UDP glucuronosyltransferases (UGTs) revealed that both UGT1A1 and UGT1A3 were capable of forming the glucuronide conjugates and the corresponding lactones for all three statins. Kinetic studies of statin glucuronidation and lactonization in liver microsomes revealed marked species differences in intrinsic clearance (CL(int)) values for SVA (but not for AVA or CVA), with the highest CL(int) observed in dogs, followed by rats and humans. Of the statins studied, SVA underwent glucuronidation and lactonization in human liver microsomes, with the lowest CL(int) (0.4 uL/min/mg of protein for SVA versus approximately 3 uL/min/mg of protein for AVA and CVA). Consistent with the present in vitro findings, substantial levels of the glucuronide conjugate (approximately 20% of dose) and the lactone form of SVA [simvastatin (SV); approximately 10% of dose] were detected in bile following i.v. administration of [(14)C]SVA to dogs. The acyl glucuronide conjugate of SVA, upon isolation from an in vitro incubation, underwent spontaneous cyclization to SV. Since the rate of this lactonization was high under conditions of physiological pH, the present results suggest that the statin lactones detected previously in bile and/or plasma following administration of SVA to animals or of AVA or CVA to animals and humans, might originate, at least in part, from the corresponding acyl glucuronide conjugates. Thus, acyl glucuronide formation, which seems to be a common metabolic pathway for the hydroxy acid forms of statins, may play an important, albeit previously unrecognized, role in the conversion of active HMG-CoA reductase inhibitors to their latent delta-lactone forms. The genetic variation underlying atorvastatin (ATV) pharmacokinetics was evaluated in a Mexican population. Aims of this study were: 1) to reveal the frequency of 87 polymorphisms in 36 genes related to drug metabolism in healthy Mexican volunteers, 2) to evaluate the impact of these polymorphisms on ATV pharmacokinetics, 3) to classify the ATV metabolic phenotypes of healthy volunteers, and 4) to investigate a possible association between genotypes and metabolizer phenotypes. A pharmacokinetic study of ATV (single 80-mg dose) was conducted in 60 healthy male volunteers. ATV plasma concentrations were measured by high-performance liquid chromatography mass spectrometry. Pharmacokinetic parameters were calculated by the non-compartmental method. The polymorphisms were determined with the PHARMAchip microarray and the TaqMan probes genotyping assay. Three metabolic phenotypes were found in our population: slow, normal, and rapid. Six gene polymorphisms were found to have a significant effect on ATV pharmacokinetics: MTHFR (rs1801133), DRD3 (rs6280), GSTM3 (rs1799735), TNFa (rs1800629), MDR1 (rs1045642), and SLCO1B1 (rs4149056). The combination of MTHFR, DRD3 and MDR1 polymorphisms associated with a slow ATV metabolizer phenotype. Atorvastatin has known human metabolites that include 7-[2-(4-Fluorophenyl)-4-[(4-hydroxyphenyl)carbamoyl]-3-phenyl-5-propan-2-ylpyrrol-1-yl]-3,5-dihydroxyheptanoic acid and 7-[2-(4-Fluorophenyl)-4-[(2-hydroxyphenyl)carbamoyl]-3-phenyl-5-propan-2-ylpyrrol-1-yl]-3,5-dihydroxyheptanoic acid. Atorvastatin is extensively metabolized to ortho- and parahydroxylated derivatives and various beta-oxidation products. In vitro inhibition of HMG-CoA reductase by ortho- and parahydroxylated metabolites is equivalent to that of atorvastatin. Approximately 70% of circulating inhibitory activity for HMG-CoA reductase is attributed to active metabolites. CYP3A4 is also involved in the metabolism of atorvastatin. Biological Half-Life The half-life of atorvastatin is 14 hours while the half-life of its metabolites can reach up to 30 hours. /MILK/ ...After administration to lactating rats, radioactivity in milk reached the maximum of 17.1 ng eq./mL at 6.0 hr and thereafter declined with a half-life of 7.8 hr. Mean plasma elimination half-life of Lipitor in humans is approximately 14 hours, but the half-life of inhibitory activity for HMG-CoA reductase is 20 to 30 hours due to the contribution of active metabolites. Oral absorption : - Healthy volunteers: Single oral dose of Atorvastatin Calcium 40 mg showed oral bioavailability (F) = 14% (low due to first-pass metabolism in liver); time to reach maximum concentration (Tmax) = 1–2 hours; maximum plasma concentration (Cmax) = 22 ng/mL [3] - Metabolism : - Hepatic metabolism: Primarily metabolized by cytochrome P450 (CYP) 3A4 to active metabolites (e.g., ortho-hydroxy atorvastatin, para-hydroxy atorvastatin), which contribute ~70% of HMG-CoA reductase inhibitory activity [3] - Elimination : - Elimination half-life (t1/2) = 14 hours (includes active metabolites); - Excretion: 90% of the dose excreted via feces (70% as metabolites, 20% as unchanged drug), 10% via urine [3] - Distribution : - Volume of distribution (Vd) = 381 L (healthy volunteers, oral 40 mg); - High liver concentration: Liver/plasma concentration ratio = 300:1 (2 hours post-dose) [3] |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
IDENTIFICATION AND USE: Atorvastatin is anticholesteremic agent and hydroxymethylglutaryl-CoA reductase inhibitor. HUMAN EXPOSURE AND TOXICITY: Cases of fatal and nonfatal hepatic failure have been reported rarely in patients receiving statins, including atorvastatin. Rhabdomyolysis with acute renal failure secondary to myoglobinuria also has been reported rarely in patients receiving statins, including atorvastatin. Lipid lowering drugs offer no benefit during pregnancy because cholesterol and cholesterol derivatives are needed for normal fetal development. Atherosclerosis is a chronic process, and discontinuation of lipid-lowering drugs during pregnancy should have little impact on long-term outcomes of primary hypercholesterolemia therapy. The occurrence of neuropsychiatric reactions is associated with statin treatment. They include behavioral alterations; cognitive and memory impairments; sleep disturbance; and sexual dysfunction. ANIMAL STUDIES: In a 2-year carcinogenicity study in rats at dose levels of 10, 30, and 100 mg/kg/day, 2 rare tumors were found in muscle in high-dose females: in one, there was a rhabdomyosarcoma, and in another, there was a fibrosarcoma. Atorvastatin caused no adverse effects on semen parameters, or reproductive organ histopathology in dogs given doses of 10, 40, or 120 mg/kg for two years. Male rats given 100 mg/kg/day for 11 weeks prior to mating had decreased sperm motility, spermatid head concentration, and increased abnormal sperm. Studies in rats performed at doses up to 175 mg/kg produced no changes in fertility. There was aplasia and aspermia in the epididymis of 2 of 10 rats treated with 100 mg/kg/day of atorvastatin for 3 months; testis weights were significantly lower at 30 and 100 mg/kg and epididymal weight was lower at 100 mg/kg. In a study in rats given 20, 100, or 225 mg/kg/day, from gestation day 7 through to lactation day 21 (weaning), there was decreased pup survival at birth, neonate, weaning, and maturity in pups of mothers dosed with 225 mg/kg/day. Body weight was decreased on days 4 and 21 in pups of mothers dosed at 100 mg/kg/day; pup body weight was decreased at birth and at days 4, 21, and 91 at 225 mg/kg/day. Pup development was delayed. In vitro, atorvastatin was not mutagenic or clastogenic in the following tests with and without metabolic activation: the Ames test with Salmonella typhimurium and Escherichia coli, the HGPRT forward mutation assay in Chinese hamster lung cells, and the chromosomal aberration assay in Chinese hamster lung cells. Atorvastatin was negative in the in vivo mouse micronucleus test. Atorvastatin selectively and competitively inhibits the hepatic enzyme HMG-CoA reductase. As HMG-CoA reductase is responsible for converting HMG-CoA to mevalonate in the cholesterol biosynthesis pathway, this results in a subsequent decrease in hepatic cholesterol levels. Decreased hepatic cholesterol levels stimulates upregulation of hepatic LDL-C receptors which increases hepatic uptake of LDL-C and reduces serum LDL-C concentrations. Toxicity Data Generally well-tolerated. Side effects may include myalgia, constipation, asthenia, abdominal pain, and nausea. Other possible side effects include myotoxicity (myopathy, myositis, rhabdomyolysis) and hepatotoxicity. To avoid toxicity in Asian patients, lower doses should be considered. Interactions Concomitant use of atorvastatin with efavirenz may result in reductions in plasma concentrations of atorvastatin. Following concomitant use of atorvastatin (10 mg daily for 3 days) and efavirenz (600 mg once daily for 14 days), atorvastatin peak plasma concentration and AUC were decreased by 1 and 41%, respectively. Concomitant use of atorvastatin (80 mg once daily for 14 days) and digoxin (0.25 mg once daily for 20 days) resulted in 20 and 15% increases in digoxin peak plasma concentration and AUC, respectively. Therefore, patients receiving such concomitant therapy should be monitored appropriately. Concomitant use of atorvastatin and azole antifungals (e.g., itraconazole) increases the risk of myopathy or rhabdomyolysis. Following concomitant use of atorvastatin (40 mg as a single dose) and itraconazole (200 mg once daily for 4 days), atorvastatin peak plasma concentration and area under the plasma concentration-time curve (AUC) were increased by 20% and 3.3-fold, respectively. Clinicians considering concomitant use of atorvastatin and itraconazole or other azole antifungals should weigh the benefits and risks of such concomitant therapy. During concomitant therapy with itraconazole, the lowest necessary dosage of atorvastatin should be employed, and dosage of atorvastatin should not exceed 20 mg daily. Patients receiving concomitant therapy with atorvastatin and azole antifungals should be monitored for manifestations of muscle pain, tenderness, or weakness, particularly during the initial months of therapy and following an increase in dosage of either drug. Concomitant use of atorvastatin and cyclosporine increases the risk of myopathy or rhabdomyolysis. Following concomitant use of atorvastatin (10 mg daily for 28 days) and cyclosporine (5.2 mg/kg daily), atorvastatin peak plasma concentration and AUC were increased by 10.7- and 8.7-fold, respectively. Concomitant use of atorvastatin and cyclosporine should be avoided. For more Interactions (Complete) data for ATORVASTATIN (27 total), please visit the HSDB record page. In vitro cytotoxicity: - HSVSMCs, rat primary myocardial cells, and HASMCs: Atorvastatin Calcium (up to 20 μM, 72-hour treatment) showed no significant cytotoxicity to non-stimulated normal cells (viability >90%, MTT assay) [2][4][5] - In vivo safety: - Post-MI rats (10 mg/kg/day, 4 weeks): No significant changes in body weight (<5% vs. Sham); serum ALT, AST, BUN, and creatinine within normal ranges [4] - ApoE-/- mice (15 mg/kg/day, 28 days): No clinical signs of toxicity (lethargy, diarrhea); liver/renal histopathology showed no abnormal damage [5] - Human patients (80 mg/day, 8 weeks): Mild, reversible ALT elevation (>3× upper limit of normal) in 2.5% of patients; no rhabdomyolysis or severe renal adverse events [3] - Plasma protein binding : - Human plasma: Protein binding rate = 98% (equilibrium dialysis, 37°C, pH 7.4) [3] |
| 参考文献 | |
| 其他信息 |
Therapeutic Uses
Anticholesteremic Agents; Hydroxymethylglutaryl-CoA Reductase Inhibitors In adult patients without clinically evident coronary heart disease, but with multiple risk factors for coronary heart disease such as age, smoking, hypertension, low HDL-C, or a family history of early coronary heart disease, Lipitor is indicated to: Reduce the risk of myocardial infarction; Reduce the risk of stroke; Reduce the risk for revascularization procedures and angina. /Included in US product label/ In patients with type 2 diabetes, and without clinically evident coronary heart disease, but with multiple risk factors for coronary heart disease such as retinopathy, albuminuria, smoking, or hypertension, Lipitor is indicated to: Reduce the risk of myocardial infarction; Reduce the risk of stroke. /Included in US product label/ In patients with clinically evident coronary heart disease, Lipitor is indicated to: Reduce the risk of non-fatal myocardial infarction; Reduce the risk of fatal and non-fatal stroke; Reduce the risk for revascularization procedures; Reduce the risk of hospitalization for congestive heart failure (CHF); Reduce the risk of angina. /Included in US product label/ For more Therapeutic Uses (Complete) data for ATORVASTATIN (15 total), please visit the HSDB record page. Drug Warnings Lipitor is contraindicated in women who are or may become pregnant. Serum cholesterol and triglycerides increase during normal pregnancy. Lipid lowering drugs offer no benefit during pregnancy because cholesterol and cholesterol derivatives are needed for normal fetal development. Atherosclerosis is a chronic process, and discontinuation of lipid-lowering drugs during pregnancy should have little impact on long-term outcomes of primary hypercholesterolemia therapy. Statins may cause fetal harm when administered to a pregnant woman. Lipitor should be administered to women of childbearing potential only when such patients are highly unlikely to conceive and have been informed of the potential hazards. If the woman becomes pregnant while taking Lipitor, it should be discontinued immediately and the patient advised again as to the potential hazards to the fetus and the lack of known clinical benefit with continued use during pregnancy. It is not known whether atorvastatin is excreted in human milk, but a small amount of another drug in this class does pass into breast milk. Nursing rat pups had plasma and liver drug levels of 50% and 40%, respectively, of that in their mother's milk. Animal breast milk drug levels may not accurately reflect human breast milk levels. Because another drug in this class passes into human milk and because statins have a potential to cause serious adverse reactions in nursing infants, women requiring Lipitor treatment should be advised not to nurse their infants. Myopathy (defined as muscle aches or weakness in conjunction with increases in creatine kinase [CK, creatine phosphokinase, CPK] concentrations exceeding 10 times the upper limit of normal [ULN]) has been reported occasionally in patients receiving statins, including atorvastatin. Rhabdomyolysis with acute renal failure secondary to myoglobinuria also has been reported rarely in patients receiving statins, including atorvastatin. For more Drug Warnings (Complete) data for ATORVASTATIN (33 total), please visit the HSDB record page. Pharmacodynamics Atorvastatin is an oral antilipemic agent that reversibly inhibits HMG-CoA reductase. It lowers total cholesterol, low-density lipoprotein-cholesterol (LDL-C), apolipoprotein B (apo B), non-high density lipoprotein-cholesterol (non-HDL-C), and triglyceride (TG) plasma concentrations while increasing HDL-C concentrations. High LDL-C, low HDL-C and high TG concentrations in the plasma are associated with increased risk of atherosclerosis and cardiovascular disease. The total cholesterol to HDL-C ratio is a strong predictor of coronary artery disease, and high ratios are associated with a higher risk of disease. Increased levels of HDL-C are associated with lower cardiovascular risk. By decreasing LDL-C and TG and increasing HDL-C, atorvastatin reduces the risk of cardiovascular morbidity and mortality. Elevated cholesterol levels (and high low-density lipoprotein (LDL) levels in particular) are an important risk factor for the development of CVD. Clinical studies have shown that atorvastatin reduces LDL-C and total cholesterol by 36-53%. In patients with dysbetalipoproteinemia, atorvastatin reduced the levels of intermediate-density lipoprotein cholesterol. It has also been suggested that atorvastatin can limit the extent of angiogenesis, which can be useful in the treatment of chronic subdural hematoma. Myopathy/Rhabdomyolysis Atorvastatin, like other HMG-CoA reductase inhibitors, is associated with a risk of drug-induced myopathy characterized by muscle pain, tenderness, or weakness in conjunction with elevated levels of creatine kinase (CK). Myopathy often manifests as rhabdomyolysis with or without acute renal failure secondary to myoglobinuria. The risk of statin-induced myopathy is dose-related, and the symptoms of myopathy are typically resolved upon drug discontinuation. Results from observational studies suggest that 10-15% of people taking statins may experience muscle aches at some point during treatment. Liver Dysfunction Statins, like some other lipid-lowering therapies, have been associated with biochemical abnormalities of liver function. Persistent elevations (> 3 times the upper limit of normal [ULN] occurring on two or more occasions) in serum transaminases occurred in 0.7% of patients who received atorvastatin in clinical trials. This effect appears to be dose-related. Endocrine Effects Statins are associated with a risk of increased serum HbA1c and glucose levels. An _in vitro_ study demonstrated a dose-dependent cytotoxic effect on human pancreatic islet β cells following treatment with atorvastatin. Moreover, insulin secretion rates decreased relative to control. HMG-CoA reductase inhibitors interfere with cholesterol synthesis and may theoretically interfere with the production of adrenal and/or gonadal steroids. Clinical studies with atorvastatin and other HMG-CoA reductase inhibitors have suggested that these agents do not affect plasma cortisol concentrations, basal plasma testosterone concentration, or adrenal reserve. However, the effect of statins on male fertility has not been fully investigated. The effects of statins on the pituitary-gonadal axis in premenopausal women are unknown. Cardiovascular Significant decreases in circulating ubiquinone levels in patients treated with atorvastatin and other statins have been observed. The clinical significance of a potential long-term statin-induced deficiency of ubiquinone has not been established. It has been reported that a decrease in myocardial ubiquinone levels could lead to impaired cardiac function in patients with borderline congestive heart failure. Lipoprotein A In some patients, the beneficial effect of lowered total cholesterol and LDL-C levels may be partly blunted by the concomitant increase in Lp(a) lipoprotein concentrations. Present knowledge suggests the importance of high Lp(a) levels as an emerging risk factor for coronary heart disease. Further studies have demonstrated statins affect Lp(a) levels differently in patients with dyslipidemia depending on their apo(a) phenotype; statins increase Lp(a) levels exclusively in patients with the low molecular weight apo(a) phenotype. Atorvastatin Calcium is a synthetic, lipophilic HMG-CoA reductase inhibitor (statin), clinically approved for the treatment of primary/secondary hypercholesterolemia, and prevention of atherosclerotic cardiovascular diseases (ASCVD) such as myocardial infarction, stroke, and unstable angina [3] - Pleiotropic mechanisms beyond lipid lowering: - Anti-inflammatory: Inhibits NF-κB activation and pro-inflammatory cytokine (TNF-α, IL-1β) secretion, alleviating inflammatory hypernociception and vascular inflammation [1][2] - Anti-apoptotic: Downregulates ER stress (reduces GRP78, CHOP) to inhibit myocardial cell apoptosis, improving post-MI heart function [4] - Anti-aneurysmal: Suppresses ER stress-mediated vascular smooth muscle cell apoptosis, reducing AAA incidence and aortic dilation [5] - Clinical advantage: Exhibits potent LDL-C-lowering efficacy (up to 60% reduction at 80 mg/day) compared to other statins (e.g., lovastatin, fluvastatin), making it suitable for patients with severe hypercholesterolemia [3] - Pharmacokinetic note: Its long half-life (14 hours) allows for once-daily administration, improving patient compliance [3] |
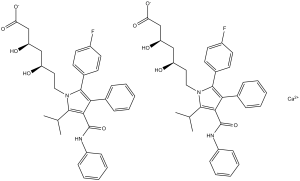
| 分子式 |
2(C33H34FN2O5).CA
|
|---|---|
| 分子量 |
1155.34
|
| 精确质量 |
1154.453
|
| CAS号 |
134523-03-8
|
| 相关CAS号 |
Atorvastatin;134523-00-5;Atorvastatin hemicalcium trihydrate;344920-08-7; Atorvastatin hemicalcium salt;134523-03-8;(3S,5S)-Atorvastatin;501121-34-2;Atorvastatin-d5 hemicalcium;222412-82-0;(rel)-Atorvastatin;110862-48-1;Atorvastatin hemicalcium trihydrate;344920-08-7;Atorvastatin-d5 sodium;222412-87-5; 609843-23-4 (lysine); 344423-98-9 (calcium trihydrate); 1035609-19-8 (magnesium trihydrate); 134523-00-5 (free acid); 1072903-92-4 (strontium) ; 134523-01-6 (sodium); 874114-41-7 (magnesium);
|
| PubChem CID |
60823
|
| 外观&性状 |
White to off-white solid powder
|
| 熔点 |
176-178°C
|
| LogP |
5
|
| tPSA |
112
|
| 氢键供体(HBD)数目 |
4
|
| 氢键受体(HBA)数目 |
6
|
| 可旋转键数目(RBC) |
12
|
| 重原子数目 |
41
|
| 分子复杂度/Complexity |
822
|
| 定义原子立体中心数目 |
2
|
| SMILES |
CC(C)C1=C(C(=C(N1CC[C@H](C[C@H](CC(=O)O)O)O)C2=CC=C(C=C2)F)C3=CC=CC=C3)C(=O)NC4=CC=CC=C4
|
| InChi Key |
XUKUURHRXDUEBC-KAYWLYCHSA-N
|
| InChi Code |
InChI=1S/C33H35FN2O5/c1-21(2)31-30(33(41)35-25-11-7-4-8-12-25)29(22-9-5-3-6-10-22)32(23-13-15-24(34)16-14-23)36(31)18-17-26(37)19-27(38)20-28(39)40/h3-16,21,26-27,37-38H,17-20H2,1-2H3,(H,35,41)(H,39,40)/t26-,27-/m1/s1
|
| 化学名 |
(3R,5R)-7-[2-(4-fluorophenyl)-3-phenyl-4-(phenylcarbamoyl)-5-propan-2-ylpyrrol-1-yl]-3,5-dihydroxyheptanoic acid
|
| 别名 |
Atorvastatin; CI 981; atorvastatin calcium trihydrate; atorvastatin, CI-981; CI981; Atorvastatin hemicalcium; calcium salt; trade name:liptonorm
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (4.33 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (4.33 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL 澄清 DMSO 储备液添加到 900 μL 玉米油中并混合均匀。 View More
配方 3 中的溶解度: 5% DMSO+castor oil:23 mg/mL 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 0.8655 mL | 4.3277 mL | 8.6555 mL | |
| 5 mM | 0.1731 mL | 0.8655 mL | 1.7311 mL | |
| 10 mM | 0.0866 mL | 0.4328 mL | 0.8655 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT05464628 | Completed | Drug: Atorvastatin Drug: ASC42 |
Healthy | Gannex Pharma Co., Ltd. | August 8, 2022 | Phase 1 |
| NCT01645410 | Completed | Drug: Atorvastatin Calcium Tablets, 40 mg |
Healthy | Dr. Reddy's Laboratories Limited | March 2009 | Phase 1 |
| NCT03247400 | Completed | Drug: 1% atorvastatin calcium salt ointment |
Non-segmental Vitiligo | Nicolaus Copernicus University | December 1, 2016 | Phase 1 Phase 2 |
| NCT01555632 | Withdrawn | Drug: atorvastatin calcium Drug: placebo |
Recurrent Prostate Cancer Stage I Prostate Cancer |
University of Nebraska | March 2012 | Not Applicable |