| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 1g |
|
||
| 2g |
|
||
| 5g |
|
||
| 10g |
|
||
| 50g | |||
| Other Sizes |

| 靶点 |
VDR/vitamin D receptor; PXR; FXR; Microbial Metabolite; Endogenous Metabolite
|
|---|---|
| 体外研究 (In Vitro) |
Lithocholic Acid 阻断 GW4064 和 CDCA 产生的 FXR 激活的 IC50 分别为 0.7 μM 和 1.4 μM [5]。在 HepG2 细胞中,10-30 μM 石胆酸可在 24 小时内抑制 100 nM GW4064 诱导的 BSEP 表达 [5]。 Lithocholic Acid (0-500 μM) 以剂量依赖性方式抑制神经母细胞瘤细胞生长(BE(2)-m17、SK-n-SH、SK-n-MCIXC 和 Lan-1)[3]。
|
| 体内研究 (In Vivo) |
Lithocholic acid (LCA) 是一种有效的胆汁淤积诱导剂,其作用机制和造模方法如下:
致病原理 • LCA 作为有毒次级胆汁酸,可通过改变肝细胞膜组分和胆汁分泌功能导致肝内胆汁淤积 • 其毒性作用表现为促进胆管上皮细胞损伤、炎症细胞浸润及胆汁酸代谢紊乱 • 通过激活FXR/PXR等核受体通路加剧胆汁淤积病理过程 动物模型构建方法 大鼠模型(急性) • 品系:Wistar雄性(250-300g) • 给药方案: o 剂量:0.2 μmol/100g o 途径:静脉注射(溶于7.5%牛血清白蛋白+0.45%生理盐水) o 处理时间:1小时后处死 小鼠模型(亚急性) • 品系:ICR雄性(5-7周龄) • 给药方案: o 剂量:150 mg/kg o 途径:口服灌胃(溶于玉米油) o 频次:每日2次,连续5次 o 处死时间:末次给药后12小时 检测指标 1. 血清生化: o 总胆红素(TBIL)、直接胆红素(DBIL)显著升高 o ALT/AST/ALP等肝酶活性增加 2. 组织病理: o 肝细胞空泡变性、胆管增生 o 汇管区炎症细胞浸润 o 毛细血管胆汁淤积 3. 功能变化: o 早期胆汁流量短暂增加,后期显著减少 o 胆汁酸(TBA)代谢紊乱 注意事项 • 静脉给药需严格控制浓度避免溶血 • 灌胃给药建议在光照周期固定时段进行以减少昼夜节律影响 需设置溶剂对照组(牛血清白蛋白/玉米油)排除载体干扰 当石胆酸以 0.6% 的比例添加到食物中连续 7 天时,会提高雄性 C57BL/6 小鼠肝脏中 TGFB1、TGFBR1 和 TGFBR2 mRNA 的水平,激活 SMAD3,并引起胆道损伤 [4]。腹腔注射石胆酸(125 mg/kg,每天两次,持续四天)的雄性 C57BL/6 小鼠会出现肝损伤,并且 AST、ALT 和 ALP 水平升高 [2]。 胆汁淤积性肝损伤是由α-异硫氰酸萘酯(ANIT)、3,5-二乙氧羰基-1,4-二氢吡啶(DDC)和Lithocholic acid(LCA)引起的。结果表明,三种小鼠胆汁淤积模型血浆中胆汁酸水平普遍升高,精氨酸水平降低。ANIT和LCA诱导的肝内PBC和PSC的血浆谷胱甘肽水平分别降低。但是,DDC诱导的肝外PSC中肝脏谷胱甘肽含量降低。ANIT和DDC模型中的血浆磷脂水平升高,而LCA模型中的磷脂水平降低。DDC模型肝脏原卟啉IX显著升高。这些代谢组学数据可能有助于区分三种胆汁淤积的代谢差异,从而有助于理解胆汁淤积性肝损伤的潜在机制。[2] 石胆酸/Lithocholic acid(LCA)诱导肝脏中TGFB1和受体TGFBR1和TGFBR2的表达。此外,免疫组织化学显示,在石胆酸/LCA暴露后,门静脉周围的TGFβ表达增加,SMAD3缺失小鼠肝细胞中SMAD3磷酸化减少。血清代谢组学表明,LCA暴露后胆汁酸增加,溶血磷脂酰胆碱(LPC)减少。有趣的是,在Smad3缺失的小鼠中,代谢改变减弱了。在Smad3缺失的小鼠中,LCA诱导的溶血磷脂酰胆碱酰基转移酶4(LPCAT4)和有机溶质转运蛋白β(OSTβ)表达显著降低,而TGFβ诱导的原代小鼠肝细胞中LPCAT4和OSTβ表达显著降低。此外,SMAD3的引入增强了TGFβ诱导的人肝细胞癌细胞系HepG2中LPCAT4和OSTβ的表达。总之,考虑到Smad3缺失小鼠的血清ALP活性减弱,这是胆管细胞损伤的诊断指标,这些结果强烈支持TGFβ-Smad3信号传导介导肝脏炎症和胆管损伤后磷脂和胆汁酸代谢改变的观点[4] 暴露于石胆酸可提高肝脏中TGFβ和受体mRNA水平[4] 使用用合成AIN93G饮食(Cont)和添加0.6%LCA的AIN93G膳食(LCA)处理7天的C57BL/6小鼠,研究了石胆酸(LCA)暴露对TGFβ信号传导的影响。肝脏TGFB1、TGFBR1和TGFBR2 mRNA水平在LCA暴露后升高,尽管肝脏中TGFBR3 mRNA水平没有变化(图1)。这些结果表明,LCA暴露刺激了肝脏中的TGFβ信号传导。 Smad3缺失小鼠Lithocholic acid/LCA诱导的肝损伤减轻[4] TGFβ通过TGFβ受体激活SMAD3。因此,为了研究SMAD3是否参与了石胆酸/Lithocholic acid/LCA诱导的肝损伤,用对照饮食和LCA饮食治疗SMAD3缺失小鼠6天。LCA暴露后,Smad3缺失小鼠的肝脏质量小于LCA治疗的野生型小鼠(图2A)。此外,在Smad3缺失的小鼠中,LCA增加的血清ALP活性显著减弱,尽管血清ALT活性没有变化(图2B,C)。此外,在Smad3缺失小鼠中,肝脏组织学显示门静脉周围有轻度炎性细胞浸润,而在类似治疗的野生型小鼠中没有观察到这种情况(图2D)。免疫组织化学显示,与野生型小鼠相比,Smad3缺失小鼠门静脉周围的TGFβ蛋白表达较低(图2E),表明TGFβ对肝脏Smad3激活的刺激较低(补充图I)。此外,在SMAD3缺失小鼠的肝细胞核中观察到SMAD3磷酸化信号的显著衰减(图2E)。这些结果表明,TGFβ-SMAD3信号传导与LCA诱导的胆管损伤有关,并增加了TGFβ-SMARD3信号传导改变肝脏代谢的可能性。 暴露于石胆酸/Lithocholic acid/LCA后,野生型和Smad3缺失小鼠血清代谢组的差异[4] 为了检测血清代谢物,使用来自喂食石胆酸/Lithocholic acid/LCA或对照饮食的小鼠血清的UPLC-ESI-QTOFMS阴性模式数据进行PLS和贡献分析。PLS分析显示,LCA处理的野生型(图3A)和LCA治疗的Smad3缺失组之间存在分离,并用负荷图进行了进一步检查(图3B)。贡献分析显示,10个增强离子和10个衰减离子是引起分离的顶级离子。与野生型小鼠相比,Smad3缺失小鼠的溶血磷脂酰胆碱(LPC)和脂肪酸片段被确定为升高的离子(表1)。最低的离子来自胆汁盐(表2)。LCA喂养后,Smad3缺失小鼠的血清代谢组在LPC和胆汁盐方面与野生型小鼠有很大不同。 |
| 细胞实验 |
用Lithocholic acid/石胆酸/LCA、过氧化氢或z-DEVD-fmk[3]处理细胞
首先在100%二甲基亚砜(DMSO)中制备不同浓度的Lithocholic acid/LCA储备溶液。为了治疗培养的人NB、人BC和大鼠GL细胞,然后将这些储备溶液稀释至指定的LCA终浓度(DMSO的终浓度始终保持在1%),稀释液为DMEM和Ham的F-12营养混合物的1:1混合物,补充了10%FBS(适用于SK-n-MCIXC和BE(2)-m17细胞),EMEM补充了10%的FBS(适用于SK-n-SH细胞),DMEM补充了10%BCS(适用于Lan-1细胞)。为了用LCA治疗人类原代神经元,将在100%DMSO中制备的不同浓度的LCA储备溶液在含有0.225%碳酸氢钠、1 mM丙酮酸钠、2 mM L-谷氨酰胺、0.1%葡萄糖和5%FBS的EMEM中稀释至LCA的指定终浓度(DMSO的终浓度始终保持在1%)。为了用LCA治疗培养的癌症细胞或原代神经元,将它们在所示最终浓度的LCA存在下孵育48小时;对照细胞仅用空的DMSO载体处理。对于用过氧化氢处理的细胞,其30%的储备溶液在无菌H2O中稀释,并在用LCA或空DMSO载体预处理24小时后直接加入细胞培养物中;然后将细胞孵育24小时。在涉及用z-DEVD-fmk进行细胞处理的实验中,这种半胱氨酸天冬氨酸蛋白酶-3抑制剂与LCA或空的DMSO载体同时添加至终浓度为5μM。 细胞活力测定[3] 使用基于MTT(3-(4,5-二甲基噻唑-2-基)-2,5-二苯基溴化四唑)的CellTiter 96非放射性细胞增殖测定法测量暴露于Lithocholic acid/LCA的培养物中活细胞的数量。在该试验中,只有活的、代谢活跃的细胞能够还原MTT的黄色四唑盐,形成紫色甲赞产物。通过加入洗涤剂使这种不溶性产物溶解。然后使用96孔板读数器在570nm波长下用分光光度法检测所得的细胞内紫色甲赞。使用630nm的波长校正信号以考虑细胞碎片。用荧光染料Hoechst在培养基中以4μM的终浓度显示暴露于LCA和/或过氧化氢和/或z-DEVD-fmk的细胞中的染色质,并使用荧光显微镜进行观察。对于每种细胞培养物,计算携带完整、非碎片化核(含非浓缩染色质)的活非凋亡细胞的百分比。死亡的凋亡细胞携带含有浓缩染色质的碎裂核,这是凋亡死亡的标志性事件。 荧光显微镜观察线粒体和测量线粒体膜电位[3] 使用培养基中浓度为125 nM的MitoTracker Red CMXRos对用Lithocholic acid/LCA处理的细胞的线粒体形态进行可视化。使用荧光显微镜观察细胞,并计算显示线粒体碎片的细胞百分比。使用四甲基罗丹明乙酯(TMRE)(一种细胞渗透性阳离子荧光染料)测量线粒体膜电位(∆Ψ)。线粒体对TMRE的可逆隔离程度与∆Ψ的值成正比。将细胞与50 nM TMRE孵育20分钟,并使用荧光显微镜直接观察。计算了显示可检测水平∆Ψ的TMRE阳性细胞的百分比。 瞬时转染试验[5] 转染前24小时,将HepG2细胞以3.2×104个细胞/孔的密度接种在含有10%FBS的DMEM中。根据制造商的说明,使用FuGENE6转染试剂在无血清Opti-MEM I培养基中用转染混合物转染细胞。通常,每个孔的转染混合物含有0.405μl FuGENE6、3 ng pcDNA3.1-GAL4-hFXR(LBD)表达载体、3 ng pc DNA3.1-hRXRα表达构建体、60 ng pUAS(5X)-tk LUC报告载体和60 ng pCMV-lacZ作为转染效率的内部对照。细胞在37°C、10%CO2的气氛中在转染混合物中孵育4小时。然后将细胞在含有5%木炭剥离FBS的新鲜DMEM中孵育约40-48小时,可添加或不添加不同浓度的配体。根据制造商的指示,使用报告裂解缓冲液生产细胞裂解物。在ML3000光度计中使用萤光素酶测定缓冲液测定细胞提取物中的萤光素酶活性。如前所述,使用β-d-吡喃半乳糖苷测定β-半乳糖苷酶活性。每个孔的萤光素酶活性分别归一化为β-半乳糖苷酶活性。当检测Lithocholic acid/LCA的拮抗活性时,在100 nm GW4064的存在下,将细胞与越来越高浓度的LCA一起孵育。 |
| 动物实验 |
Animal/Disease Models: Male mice (C57BL/6)[4].
Doses: 0.6% LCA-supplement diet, with the AIN93G diet as a control Route of Administration: in diet, for 6 days Experimental Results: Induced liver injury. Activated TGFβ-SMAD3 signaling. Increased serum ALP activities. Animal/Disease Models: Male mice (C57BL/6)[2]. Doses: 125 mg/kg, dissolved in corn oil Route of Administration: ip, twice a day for four days Experimental Results: Induced liver injury, generated necrosis and neutrophilic -granulocytic infiltrate (H&E staining). Increased AST, ALT and ALP level. Animals studies [2] Male C57BL/6 mice (6–8 weeks old) were housed under temperature and humidity-controlled conditions with a 12 h light/12 h dark cycle. Thirty mice were randomly divided into six groups: (1) control of ANIT (ANIT-C); (2) ANIT; (3) control of DDC (DDC-C); (4) DDC; (5) control of Lithocholic acid/LCA (LCA-C); (6) LCA. ANIT dissolved in corn oil was given at a single dose of 75 mg/kg by gavage and mice were sacrificed 48 h after treatment (Fang et al., 2017; Tang et al., 2016). The administration of DDC was slightly modified on the previous reports (Dai et al., 2017; Fickert et al., 2007). DDC dissolved in corn oil was given at an oral dose 100 mg/kg for seven consecutive days, and mice were euthanized 24 h after the last dose of DDC. LCA dissolved in corn oil was intraperitoneal administered at dose of 125 mg/kg twice a day for four days consecutively (Beilke et al., 2009; Owen et al., 2010) and sacrificed 24 h after the last dose of LCA. The mice treated with corn oil were used as the control groups. All the mice were sacrificed by CO2 inhalation. Subsequently, mice plasma and liver samples were collected for biochemical assay, histopathology and metabolomic analysis. Biochemical assay included ALT, AST and ALP. Part of liver tissue were stained with hematoxylin and eosin (H&E) for histopathology using the method described previously (Hu et al., 2018) and the others were stored at −80 °C. Animals and diets [4] Male mice (C57BL/6), MAD homolog 3 (Smad3)-null mice, and background-matched wild-type mice were housed in temperature- and light-controlled rooms and given water and pelleted NIH-31 chow ad libitum. For the Lithocholic acid/LCA studies, mice were given 0.6% LCA-supplement diet with the AIN93G diet as a control. Three wild-type and three Smad3-null mice were fed the control diet, and five wild-type and four Smad3-null mice were given the LCA diet. |
| 药代性质 (ADME/PK) |
Metabolism / Metabolites
LITHOCHOLIC ACID (24)C(14) IS CONVERTED BY RAT LIVER HOMOGENATE INTO 3ALPHA-6BETA-DIHYDROXY-5BETA-CHOLANIC ACID, 7SIGMA-HYDROXYLATION OCCURS, HYDROXYLATION CONJUGATION WITH TAURINE & FORMATION OF 3-SULFATE ESTER CAN BE DEMONSTRATED. LABELED LITHOCHOLATE WAS INJECTED INTO GALLSTONE PATIENTS & HEALTHY VOLUNTEERS, MAJORITY OF RADIOACTIVITY IN BILE (50-60%) WAS PRESENT AS SULFATED CONJUGATES. DEGREE OF SULFATION WAS GREATER FOR GLYCINE THAN TAURINE CONJUGATES, WHICH SUGGESTED PREFERENTIAL SULFATION OF GLYCINE CONJUGATES. Lithocholic Acid has known human metabolites that include 6alpha-Hydroxylithocholic acid. |
| 毒性/毒理 (Toxicokinetics/TK) |
Interactions
SKIN TUMOR INHIBITION DECR IN FOLLOWING ORDER OF ACIDS: CHENODEOXYCHOLIC, LITHOCHOLIC, DEOXYCHOLIC, & CHOLIC. 16ALPHA-CYANOPREGNENOLONE (5 MG IP TWICE DAILY FOR 2 DAYS) INCR IN VITRO RAT LIVER MICROSOMAL 6BETA- & 7ALPHA-HYDROXYLATION OF LITHOCHOLIC ACID BY FACTORS OF 2 & 3-4 RESPECTIVELY. THIS MAY ACCOUNT FOR PREVENTION OF LITHOCHOLIC ACID-INDUCED CHOLELITHIASIS. LITHOCHOLIC ACID (24)C(14) IS CONVERTED BY RAT LIVER HOMOGENATE INTO 3ALPHA-6BETA-DIHYDROXY-5BETA-CHOLANIC ACID. ADDN OF ETHANOL TO ENZYMATIC SYSTEM RESULTS IN INHIBITION OF FORMATION OF 3ALPHA, 6BETA-DIHYDROXY-5BETA-CHOLANIC ACID. SODIUM LITHOCHOLATE INCR MNNG (N-METHYL-N'-NITRO-N-NITROSOGUANIDINE) INDUCED COLON TUMOR INCIDENCE IN BOTH GERM-FREE & CONVENTIONAL RATS (F344). /SODIUM LITHOCHOLATE/ LCA was also tested as a promoter of N-Nitrobis(2-hydroxypropyl)amine (BHP) induced carcinogenesis. Two groups of 5 to 6-wk-old hamsters (number not stated) were given 500 mg/kg BHP subcutaneously once per week for 5 weeks, and group 3 was given no further treatment; group 4 was given 0.5% LCA in feed for 30 weeks, all animals were autopsied at 35 weeks. There was no difference in food consumption or body weight between these 2 groups. There were no differences in number on liver lesions (group 3: 15/15 hyperplastic nodules, 2/15 hepatocellular carcinoma, 1/15 cholangiocarcinoma; group 4: 22/22 hyperplastic nodules, 3/22 hepatocellular carcinoma, 3/22 cholangiocarcinoma). However, there was a significant difference in the pancreatic tumors: group 3 had 4/15 gross tumors, 5/15 carcinomas, 4/15 adenomas while group 4 had 13/22 gross tumors, 15/22 carcinomas (P<.04) and 2/22 adenomas. Under the conditions of this experiment, LCA was not carcinogenic when administered alone, but was an effective promoter of BHP pancreatic carcinogenesis. mouse LD50 oral 3900 mg/kg Progress Report for Contract No. NIH-NCI-E-C-72-3252, Submitted to the National Cancer Institute by Litton Bionetics, Inc., NCI-E-C-72-3252(1973) |
| 参考文献 |
|
| 其他信息 |
Hexagonal leaflets (from alcohols) or prisms (from acetic acid) or white powder. (NTP, 1992)
Lithocholic acid is a monohydroxy-5beta-cholanic acid with a alpha-hydroxy substituent at position 3. It is a bile acid obtained from chenodeoxycholic acid by bacterial action. It has a role as a human metabolite, a mouse metabolite and a geroprotector. It is a bile acid, a monohydroxy-5beta-cholanic acid and a C24-steroid. It is a conjugate acid of a lithocholate. Lithocholic acid has been reported in Homo sapiens with data available. A bile acid formed from chenodeoxycholate by bacterial action, usually conjugated with glycine or taurine. It acts as a detergent to solubilize fats for absorption and is itself absorbed. It is used as cholagogue and choleretic. As described above that bile ducts obstruction are the pathological feature of PBC and PSC, several bile acids were commonly increased in three chemical-induced cholestatic models, including TCDCA, T-α/β-MCA and TH/UDCA. In addition to the elevated bile acids in three cholestasis models, the level of arginine was decreased. ANIT and DDC models disrupted the lipids metabolism, which resulted in the increase of LPCs and carnitines levels in both plasma and liver. Different from ANIT and LCA models, liver GSH was decreased in DCC-induced liver damage (Fig. S3). DDC model induced the accumulation of PPIX in the liver, while the level of PPIX was decreased in ANIT and LCA models. Considering that PPIX was converted to heme for oxygen transfer in vivo, the decreased PPIX in ANIT and LCA models might be an adaptive response for improvement of cell damage. Taken together, these changes may partly illustrate the differences of three types of cholestatic liver damage, contributing to the understanding of potential mechanism from different types of cholestasis. The data presented herein establish the benefits of metabolomics approach in biomarker discovery for cholestatic liver injury.[2] Aging is one of the major risk factors of cancer. The onset of cancer can be postponed by pharmacological and dietary anti-aging interventions. We recently found in yeast cellular models of aging that lithocholic acid (LCA) extends longevity. Here we show that, at concentrations that are not cytotoxic to primary cultures of human neurons, LCA kills the neuroblastoma (NB) cell lines BE(2)-m17, SK-n-SH, SK-n-MCIXC and Lan-1. In BE(2)-m17, SK-n-SH and SK-n-MCIXC cells, the LCA anti-tumor effect is due to apoptotic cell death. In contrast, the LCA-triggered death of Lan-1 cells is not caused by apoptosis. While low concentrations of LCA sensitize BE(2)-m17 and SK-n-MCIXC cells to hydrogen peroxide-induced apoptotic cell death controlled by mitochondria, these LCA concentrations make primary cultures of human neurons resistant to such a form of cell death. LCA kills BE(2)-m17 and SK-n-MCIXC cell lines by triggering not only the intrinsic (mitochondrial) apoptotic cell death pathway driven by mitochondrial outer membrane permeabilization and initiator caspase-9 activation, but also the extrinsic (death receptor) pathway of apoptosis involving activation of the initiator caspase-8. Based on these data, we propose a mechanism underlying a potent and selective anti-tumor effect of LCA in cultured human NB cells. Moreover, our finding that LCA kills cultured human breast cancer and rat glioma cells implies that it has a broad anti-tumor effect on cancer cells derived from different tissues and organisms.[3] Bile salt export pump (BSEP) is a major bile acid transporter in the liver. Mutations in BSEP result in progressive intrahepatic cholestasis, a severe liver disease that impairs bile flow and causes irreversible liver damage. BSEP is a target for inhibition and down-regulation by drugs and abnormal bile salt metabolites, and such inhibition and down-regulation may result in bile acid retention and intrahepatic cholestasis. In this study, we quantitatively analyzed the regulation of BSEP expression by FXR ligands in primary human hepatocytes and HepG2 cells. We demonstrate that BSEP expression is dramatically regulated by ligands of the nuclear receptor farnesoid X receptor (FXR). Both the endogenous FXR agonist chenodeoxycholate (CDCA) and synthetic FXR ligand GW4064 effectively increased BSEP mRNA in both cell types. This up-regulation was readily detectable at as early as 3 h, and the ligand potency for BSEP regulation correlates with the intrinsic activity on FXR. These results suggest BSEP as a direct target of FXR and support the recent report that the BSEP promoter is transactivated by FXR. In contrast to CDCA and GW4064, lithocholate (LCA), a hydrophobic bile acid and a potent inducer of cholestasis, strongly decreased BSEP expression. Previous studies did not identify LCA as an FXR antagonist ligand in cells, but we show here that LCA is an FXR antagonist with partial agonist activity in cells. In an in vitro co-activator association assay, LCA decreased CDCA- and GW4064-induced FXR activation with an IC(50) of 1 microm. In HepG2 cells, LCA also effectively antagonized GW4064-enhanced FXR transactivation. These data suggest that the toxic and cholestatic effect of LCA in animals may result from its down-regulation of BSEP through FXR. Taken together, these observations indicate that FXR plays an important role in BSEP gene expression and that FXR ligands may be potential therapeutic drugs for intrahepatic cholestasis.[5] LCA was recently identified as a PXR/SXR agonist ligand. PXR is thought to be the second bile acid receptor and plays a critical role in liver detoxification (27, 28). However, there is no evidence supporting the involvement of PXR in BSEP gene regulation. Indeed, the PXR-specific ligand rifampicin did not regulate BSEP expression, suggesting that PXR is not involved in BSEP regulation and further supporting the conclusion that the down-regulation of BSEP by LCA is mediated through the antagonist activity on FXR. BSEP expression is critically important for liver protection. The identification of FXR as an important regulator of BSEP not only provides a molecular mechanism for FXR-mediated BSEP gene regulation but also suggests a potential for FXR ligands as therapeutic drugs for intrahepatic cholestasis and lipid disorders.[5] |
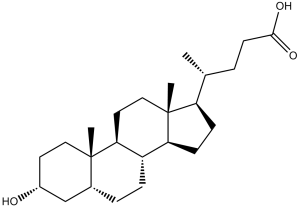
| 分子式 |
C24H40O3
|
|
|---|---|---|
| 分子量 |
376.57
|
|
| 精确质量 |
376.297
|
|
| 元素分析 |
C, 76.55; H, 10.71; O, 12.75
|
|
| CAS号 |
434-13-9
|
|
| 相关CAS号 |
Allolithocholic acid;2276-94-0;Isoallolithocholic acid;2276-93-9;Isolithocholic acid;1534-35-6;Lithocholic acid-d4;83701-16-0;Lithocholic acid-d5;52840-06-9
|
|
| PubChem CID |
9903
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| 密度 |
1.1±0.1 g/cm3
|
|
| 沸点 |
511.0±23.0 °C at 760 mmHg
|
|
| 熔点 |
183-188 °C(lit.)
|
|
| 闪点 |
276.9±19.1 °C
|
|
| 蒸汽压 |
0.0±3.0 mmHg at 25°C
|
|
| 折射率 |
1.528
|
|
| LogP |
6.7
|
|
| tPSA |
57.53
|
|
| 氢键供体(HBD)数目 |
2
|
|
| 氢键受体(HBA)数目 |
3
|
|
| 可旋转键数目(RBC) |
4
|
|
| 重原子数目 |
27
|
|
| 分子复杂度/Complexity |
574
|
|
| 定义原子立体中心数目 |
9
|
|
| SMILES |
C[C@H](CCC(=O)O)[C@H]1CC[C@@H]2[C@@]1(CC[C@H]3[C@H]2CC[C@H]4[C@@]3(CC[C@H](C4)O)C)C
|
|
| InChi Key |
SMEROWZSTRWXGI-HVATVPOCSA-N
|
|
| InChi Code |
InChI=1S/C24H40O3/c1-15(4-9-22(26)27)19-7-8-20-18-6-5-16-14-17(25)10-12-23(16,2)21(18)11-13-24(19,20)3/h15-21,25H,4-14H2,1-3H3,(H,26,27)/t15-,16-,17-,18+,19-,20+,21+,23+,24-/m1/s1
|
|
| 化学名 |
3alpha-Hydroxy-5beta-cholan-24-oic acid
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.08 mg/mL (5.52 mM) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 20.8 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.08 mg/mL (5.52 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 20.8 mg/mL 澄清 DMSO 储备液加入到 900 μL 玉米油中并混合均匀。 View More
配方 3 中的溶解度: ≥ 1 mg/mL (2.66 mM) (饱和度未知) in 10% EtOH + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 配方 4 中的溶解度: ≥ 1 mg/mL (2.66 mM) (饱和度未知) in 10% EtOH + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将100μL 10.0mg/mL澄清EtOH储备液加入到900μL 20%SBE-β-CD生理盐水中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 配方 5 中的溶解度: ≥ 1 mg/mL (2.66 mM) (饱和度未知) in 10% EtOH + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加),澄清溶液。 例如,若需制备1 mL的工作液,可将100 μL 10.0 mg/mL 澄清 EtOH 储备液添加到 900 μL 玉米油中并充分混合。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.6555 mL | 13.2777 mL | 26.5555 mL | |
| 5 mM | 0.5311 mL | 2.6555 mL | 5.3111 mL | |
| 10 mM | 0.2656 mL | 1.3278 mL | 2.6555 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。