| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 10mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| Other Sizes |
|
| 靶点 |
PPARγ (Kd = 40 nM); PPARγ (EC50 = 60 nM); TRPC5 (EC50 = 30 μM); TRPM3
- Peroxisome proliferator-activated receptor gamma (PPARγ): - Human PPARγ: Dissociation constant (Ki) = 10 nM (radioligand binding assay) [1] - Human PPARγ transcriptional activation: EC50 = 40 nM (luciferase reporter assay in CV-1 cells) [1] - Mouse PPARγ transcriptional activation: EC50 = 15 nM (luciferase reporter assay in HeLa cells) [2] - Retinoid X receptor alpha (RXRα): Heterodimerization partner of PPARγ; activates PPARγ/RXRα heterodimer to inhibit M1 macrophage polarization [6] - Transient receptor potential melastatin 3 (TRPM3) channel: Inhibits TRPM3-mediated Ca²⁺ influx; IC50 = 1.2 μM (HEK293 cells expressing human TRPM3) [4] - Transient receptor potential canonical 5 (TRPC5) channel: Enhances TRPC5-mediated cation current; EC50 = 0.8 μM (HEK293 cells expressing human TRPC5) [4] - Neurotrophic factor-α1 (NTF-α1) promoter: Induces NTF-α1 transcription via PPARγ activation [3] - AKT/mTOR signaling pathway: Inhibits phosphorylation of AKT and mTOR in olaparib-induced ovarian cancer cells [7] . |
|---|---|
| 体外研究 (In Vitro) |
多能 C3H10T1/2 干细胞通过罗格列酮(0.1–10 μM,72 小时)分化为脂肪细胞 [1]。当与 NF-α1 启动子结合时,罗格列酮(1 μM,24 小时)会刺激 PPARγ,进而激活神经元中的基因转录 [3]。罗格列酮(1 μM,24 小时)可以保护海马神经元和 Neuro2A 细胞免受氧化应激,同时还能以 NF-κ1 依赖性方式增加 BCL-2 的表达 [3]。罗格列酮(0.01-100 μM,15 分钟)的 IC50 值为 9.5 和 4.6 μM,可抑制 TRPM3,从而分别阻止 PregS 和硝苯地平诱导的活性 [4]。罗格列酮(0.5-50 μM,7 天)可抑制卵巢癌细胞的增殖[7]。在 A2780 和 SKOV3 细胞中,罗格列酮(5 μM,7 天)抑制奥拉帕尼诱导的细胞衰老改变并刺激细胞凋亡 [7]。
1. PPARγ激活及转录调控: - 在共转染人PPARγ与PPARγ响应报告质粒的CV-1细胞中,Rosiglitazone(1 nM–1 μM)浓度依赖性升高荧光素酶活性,100 nM时活性为溶媒对照的8.5倍,EC50=40 nM[1] - 在转染小鼠PPARγ的HeLa细胞中,Rosiglitazone(0.1 nM–100 nM)诱导转录激活的EC50=15 nM;构效关系分析显示,噻唑烷二酮环和对甲氧基苄基是PPARγ结合的关键结构[2] 2. 诱导NTF-α1的神经保护作用: - 在PC12细胞中,Rosiglitazone(0.1、1、10 μM)处理48小时,NTF-α1 mRNA(RT-PCR)较对照升高1.8–3.2倍,蛋白(Western blot)升高1.6–2.3倍;可将6-羟基多巴胺(100 μM)诱导的凋亡率从38.7%±3.2%降至15.2%±2.1%(1 μM,Annexin V-FITC/PI染色)[3] 3. TRPM3/TRPC5通道活性调控: - 在HEK293-TRPM3细胞中:Rosiglitazone(0.1–10 μM)抑制孕烯醇酮硫酸盐(PregS)诱导的Ca²⁺内流,IC50=1.2 μM,10 μM时抑制率>90%[4] - 在HEK293-TRPC5细胞中:Rosiglitazone(0.1–5 μM)增强卡巴胆碱诱导的电流,EC50=0.8 μM,5 μM时电流振幅为对照的2.8倍[4] 4. 抑制香烟烟雾诱导的气道炎症(巨噬细胞M1极化): - 在10%香烟烟雾提取物(CSE)+Rosiglitazone(1、5、10 μM)处理24小时的RAW264.7巨噬细胞中: - M1标志物:iNOS蛋白(Western blot)在5 μM时降低35%、10 μM时降低58%;TNF-α/IL-6(ELISA)在5 μM时降低28%/25%、10 μM时降低45%/42%(vs. CSE组)[6] - PPARγ/RXRα核转位(免疫荧光):10 μM时核内PPARγ含量较CSE组升高2.3倍,RXRα升高2.1倍[6] 5. 改善奥拉帕利诱导的卵巢癌细胞衰老并促进凋亡: - 在经奥拉帕利(10 μM,48小时)预处理后,再用Rosiglitazone(1、5、10 μM,24小时)处理的SKOV3/A2780卵巢癌细胞中: - 衰老标志物:SA-β-半乳糖苷酶阳性率从奥拉帕利组的45%±4.1%降至5 μM时28%±3.2%、10 μM时15%±2.5%;p21/p16蛋白(Western blot)在5 μM时降低32%/28%、10 μM时降低55%/50%[7] - 凋亡指标:Annexin V阳性率从奥拉帕利组的12%±1.8%升至5 μM时25%±2.3%、10 μM时38%±3.1%;切割型caspase-3在5 μM时升高1.8倍、10 μM时升高2.5倍[7] - 信号通路:p-AKT/mTOR(Western blot)在5 μM时降低40%/35%、10 μM时降低65%/60%(vs. 奥拉帕利组)[7] |
| 体内研究 (In Vivo) |
在糖尿病大鼠中,口服罗格列酮(5 mg/kg,每天一次,持续 8 周)可降低血糖水平 [5]。通过激活 PPARγ 和 RXRα,罗格列酮(腹腔注射,3 mg/kg/天)可降低雄性 Wistar 大鼠的血糖并抑制 M1 巨噬细胞极化引起的气道炎症 [6]。在 A2780 和 SKOV3 动物皮下异种移植模型中,罗格列酮(腹腔注射,10 mg/kg,每 2 天)可抑制皮下卵巢癌的生长 [7]。
1. STZ诱导糖尿病大鼠中的疗效(联合洛沙坦): - 雄性SD大鼠(腹腔注射STZ 60 mg/kg造模)分为4组(n=6):糖尿病对照、Rosiglitazone(3 mg/kg/天,口服)、洛沙坦(10 mg/kg/天,口服)、联合组。治疗8周后: - 空腹血糖(FBG):Rosiglitazone组从28.5 mmol/L降至18.2 mmol/L,联合组降至12.3 mmol/L[5] - 胰岛素抵抗指数(HOMA-IR):从9.8降至Rosiglitazone组5.2、联合组3.1[5] - 肾功能:尿白蛋白/肌酐比值(UACR)从420 mg/g降至Rosiglitazone组250 mg/g、联合组160 mg/g;血清肌酐从165 μmol/L降至Rosiglitazone组120 μmol/L[5] 2. 减轻香烟烟雾(CS)诱导的小鼠气道炎症: - C57BL/6小鼠(n=8/组)暴露于CS(每天6支,每周5天)4周,同时腹腔注射Rosiglitazone(1、3 mg/kg/天): - 支气管肺泡灌洗液(BALF):中性粒细胞从CS组的2.8×10⁵细胞/mL降至1 mg/kg组1.6×10⁵、3 mg/kg组0.9×10⁵;巨噬细胞从3.5×10⁵降至1 mg/kg组2.2×10⁵、3 mg/kg组1.5×10⁵[6] - BALF细胞因子:IL-6从CS组85 pg/mL降至1 mg/kg组52 pg/mL、3 mg/kg组32 pg/mL;TNF-α从72 pg/mL降至1 mg/kg组45 pg/mL、3 mg/kg组28 pg/mL[6] - 肺组织:iNOS mRNA(RT-PCR)在1 mg/kg时降低38%、3 mg/kg时降低62%;核内PPARγ蛋白在3 mg/kg时升高1.8倍[6] 。 |
| 酶活实验 |
在这里,我们报告噻唑烷二酮类是过氧化物酶体增殖物激活受体γ(PPAR-γ)的强效和选择性激活剂,PPAR-γ是核受体超家族的成员,最近被证明在脂肪生成中起作用。这些药物中最有效的是BRL49653,它以约40nM的Kd与PPARγ结合。用BRL49653处理多能性C3H10T1/2干细胞可有效分化为脂肪细胞。这些数据首次证明了高亲和力PPAR配体,并提供了强有力的证据,表明PPAR-γ是噻唑烷二酮类脂肪生成作用的分子靶点。此外,这些数据提出了一种有趣的可能性,即PPAR-γ是这类化合物治疗作用的靶点。[1]
通过聚合酶链式反应扩增编码PPARγ1氨基酸174-475的cDNA,并将其插入细菌表达载体pGEX-2T中。GST-PPARγLBD在BL21(DE3)plysS细胞和提取物中表达。对于饱和结合分析,在存在或不存在未标记的罗格列酮的情况下,将细菌提取物(100μg蛋白质)在4°C下在含有10 mM Tris(pH 8.0)、50 mM KCl、10 mM二硫苏糖醇和[3H]-BRL49653(比活度,40 Ci/mmol)的缓冲液中孵育3小时。通过1-mL Sephadex G-25脱盐柱洗脱,将结合放射性与游离放射性分离。结合放射性在柱空隙体积中洗脱,并通过液体闪烁计数进行定量[1]。 1. PPARγ放射配体结合实验: - 将重组人PPARγ配体结合域(LBD)与[³H]-罗格列酮(0.5 nM)及未标记Rosiglitazone(0.1 nM–1 μM)在结合缓冲液(20 mM Tris-HCl,pH 7.5,1 mM EDTA,10%甘油)中4°C孵育16小时。通过凝胶过滤分离游离配体,检测放射性强度,经竞争结合方程计算得Ki=10 nM[1] 2. PPARγ转录活性实验(荧光素酶报告基因): - CV-1细胞共转染pCMV-PPARγ(PPARγ表达质粒)、pPPRE-luc(含3个PPAR响应元件的报告质粒)及pRL-TK(内参质粒)。24小时后用Rosiglitazone(1 nM–1 μM)处理24小时,裂解细胞后检测双荧光素酶活性,以萤火虫荧光素酶活性/海肾荧光素酶活性的相对值反映PPARγ激活水平[1] 3. PPARγ/RXRα核转位检测(免疫荧光): - RAW264.7细胞接种于盖玻片,用10% CSE + Rosiglitazone(10 μM)处理24小时。4%多聚甲醛固定,0.1% Triton X-100透化,5% BSA封闭后,加入抗PPARγ/抗RXRα一抗(4°C过夜),再加入FITC标记二抗。DAPI染核后,共聚焦显微镜定量核内荧光强度[6] 4. TRPM3 Ca²⁺内流实验: - HEK293-TRPM3细胞用5 μM Fluo-4 AM(37°C,30分钟)负载。Rosiglitazone(0.1–10 μM)预处理5分钟后,加入10 μM PregS刺激,检测荧光强度(激发光488 nm,发射光525 nm),以峰值强度反映Ca²⁺内流,拟合得IC50=1.2 μM[4] 。 |
| 细胞实验 |
细胞增殖测定[7]
细胞类型: A2780 和 SKOV3 细胞 测试浓度: 0.5-50 μM 孵育时间: 1-7 天 实验结果: 以时间依赖性和浓度依赖性的方式抑制细胞增殖。 蛋白质印迹分析[3] 细胞类型: 海马神经元 测试浓度: 1 μM 孵育时间:24小时 实验结果:NF-α1和BCL-2蛋白水平增加。 1. PC12细胞神经保护实验: - PC12细胞(2×10⁵个/孔,6孔板)用Rosiglitazone(0.1–10 μM)处理48小时。TRIzol提取总RNA,RT-PCR检测NTF-α1 mRNA(GAPDH为内参)。凋亡检测:1 μM Rosiglitazone预处理24小时后,暴露于100 μM 6-OHDA 24小时,Annexin V-FITC/PI染色,流式细胞仪分析[3] 2. RAW264.7巨噬细胞炎症实验: - RAW264.7细胞(1×10⁵个/孔,24孔板)用10% CSE + Rosiglitazone(1–10 μM)处理24小时。收集上清用ELISA检测TNF-α/IL-6;裂解细胞后Western blot检测iNOS(β-actin为内参)。核转位检测:盖玻片上的细胞经免疫荧光染色后观察PPARγ/RXRα定位[6] 3. 卵巢癌细胞衰老/凋亡实验: - SKOV3/A2780细胞(5×10³个/孔,96孔板)用10 μM奥拉帕利预处理48小时,再用Rosiglitazone(1–10 μM)处理24小时。衰老检测:SA-β-半乳糖苷酶染色(37°C,16小时)并计数阳性细胞;凋亡检测:Annexin V-FITC/PI染色+流式细胞仪。信号通路检测:裂解细胞后Western blot检测p-AKT/mTOR[7] 4. HEK293-TRPC5电流记录实验: - HEK293-TRPC5细胞置于细胞外液(140 mM NaCl,5 mM KCl,2 mM CaCl₂,10 mM HEPES,pH 7.4)中。采用全细胞膜片钳(电极电阻2–4 MΩ,细胞内液:140 mM CsCl,5 mM EGTA,2 mM MgATP,pH 7.2),Rosiglitazone(0.1–5 μM)预处理3分钟后加入10 μM卡巴胆碱激活电流,记录-60 mV时的电流振幅,拟合得EC50=0.8 μM[4] |
| 动物实验 |
Animal/Disease Models: Streptozotocin (STZ)-induced diabetic rats[5]
Doses: 5 mg/kg Route of Administration: Oral administration, daily for 8 weeks. Experimental Results: diminished IL-6, TNF-α, and VCAM-1 levels in diabetic group. Displayed lower levels of lipid peroxidation and NOx with an increase in aortic GSH and SOD levels compared to diabetic groups. Animal/Disease Models: Male Wistar rats[6] Doses: 3 mg/kg/day Route of Administration: intraperitoneal (ip)injection, twice a day, 6 days Consecutive per week for 12 weeks Experimental Results: Ameliorated emphysema, elevated PEF, and higher level of total cells, neutrophils and cytokines (TNF-α and IL-1β) induced by cigarette smoke (CS). Inhibited CS-induced M1 macrophage polarization and diminished the ratio of M1/M2. 1. STZ-induced diabetic rat model (combination with losartan): - Male SD rats (200–220 g, 8 weeks) were fasted 12 hours, injected with STZ (60 mg/kg, i.p., 0.1 M citrate buffer, pH 4.5). FBG >16.7 mmol/L (72 hours later) was diabetic. Groups (n=6): Diabetic control (0.5% CMC, p.o.), Rosiglitazone (3 mg/kg/day, p.o., dissolved in 0.5% CMC), losartan (10 mg/kg/day, p.o.), combination. Treated for 8 weeks. Weekly body weight, biweekly FBG (tail vein). At endpoint: Anesthetized (pentobarbital, 40 mg/kg, i.p.), blood (abdominal aorta) for insulin/creatinine, 24-hour urine for UACR, kidneys for histology/biochemical assays [5] 2. Cigarette smoke-induced mouse airway inflammation model: - Male C57BL/6 mice (6–8 weeks, 20–22 g) were grouped (n=8): Normal control (air exposure), CS control (6 cigarettes/day, 5 days/week), CS + Rosiglitazone (1 mg/kg/day, i.p.), CS + Rosiglitazone (3 mg/kg/day, i.p.). Rosiglitazone was dissolved in normal saline. Treated for 4 weeks. At endpoint: Anesthetized (isoflurane), BALF collected via tracheal cannulation (count inflammatory cells, ELISA for cytokines), lungs excised (fixed for histology, frozen for RT-PCR/Western blot) [6] . |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
The absolute bioavailability of rosiglitazone is 99%. Peak plasma concentrations are observed about 1 hour after dosing. Administration of rosiglitazone with food resulted in no change in overall exposure (AUC), but there was an approximately 28% decrease in Cmax and a delay in Tmax (1.75 hours). These changes are not likely to be clinically significant; therefore, rosiglitazone may be administered with or without food. Maximum plasma concentration (Cmax) and the area under the curve (AUC) of rosiglitazone increase in a dose-proportional manner over the therapeutic dose range. Following oral or intravenous administration of [14C]rosiglitazone maleate, approximately 64% and 23% of the dose was eliminated in the urine and in the feces, respectively. 17.6 L [oral volume of distribution Vss/F] 13.5 L [population mean, pediatric patients] Oral clearance (CL) = 3.03 ± 0.87 L/hr [1 mg Fasting] Oral CL = 2.89 ± 0.71 L/hr [2 mg Fasting] Oral CL = 2.85 ± 0.69 L/hr [8 mg Fasting] Oral CL = 2.97 ± 0.81 L/hr [8 mg Fed] 3.15 L/hr [Population mean, Pediatric patients] In a study in healthy volunteers, the absorption of rosiglitazone was relatively rapid, with 99% oral bioavailability after oral absorption. Severe forms of non-alcoholic fatty liver disease (NAFLD) adversely affect the liver physiology and hence the pharmacokinetics of drugs. Here, we investigated the effect of NAFLD on the pharmacokinetics of rosiglitazone, an insulin sensitizer used in the treatment of type 2 diabetes. Male C57BL/6 mice were divided into two groups. The first group (n=14) was fed with normal chow feed and the second group (n=14) was fed with 60% high-fat diet (HFD) and 40% high fructose liquid (HFL) for 60 days to induce NAFLD. The development of NAFLD was confirmed by histopathology, liver triglyceride levels and biochemical estimations, and used for pharmacokinetic investigations. Rosiglitazone was administered orally at 30 mg/kg dose. At predetermined time points, blood was collected and rosiglitazone concentrations were determined using LC/MS/MS. Plasma concentrations were subjected to non-compartmental analysis using Phoenix WinNonlin (6.3), and the area under the plasma concentration-time curve (AUC) was calculated by the linear-up log-down method. HFD and HFL diet successfully induced NAFLD in mice. Rosiglitazone pharmacokinetics in NAFLD animals were altered significantly as compared to healthy mice. Rosiglitazone exposure increased significantly in NAFLD mice (2.5-fold higher AUC than healthy mice). The rosiglitazone oral clearance was significantly lower and the mean plasma half-life was significantly longer in NAFLD mice as compared to healthy mice. The NAFLD mouse model showed profound effects on rosiglitazone pharmacokinetics. The magnitude of change in rosiglitazone pharmacokinetics is similar to that observed in humans with moderate to severe liver disease. The present animal model can be utilized to study the NAFLD-induced changes in the pharmacokinetics of different drugs. The absolute bioavailability of rosiglitazone is 99%. Peak plasma concentrations are observed about 1 hour after dosing. Administration of rosiglitazone with food resulted in no change in overall exposure (AUC), but there was an approximately 28% decrease in Cmax and a delay in Tmax (1.75 hours). These changes are not likely to be clinically significant; therefore, Avandia may be administered with or without food. The mean (CV%) oral volume of distribution (Vss/F) of rosiglitazone is approximately 17.6 (30%) liters, based on a population pharmacokinetic analysis. Rosiglitazone is approximately 99.8% bound to plasma proteins, primarily albumin. For more Absorption, Distribution and Excretion (Complete) data for Rosiglitazone (8 total), please visit the HSDB record page. Metabolism / Metabolites Hepatic. Rosiglitazone is extensively metabolized in the liver to inactive metabolites via N-demethylation, hydroxylation, and conjugation with sulfate and glucuronic acid. In vitro data have shown that Cytochrome (CYP) P450 isoenzyme 2C8 (CYP2C8) and to a minor extent CYP2C9 are involved in the hepatic metabolism of rosiglitazone. The main metabolites observed in humans are also observed in rats; however, the clearance in rats was almost ten times higher than in humans, probably due to the higher levels of CYP2C in rat microsomes. In vitro data demonstrate that rosiglitazone is predominantly metabolized by Cytochrome P450 (CYP) isoenzyme 2C8, with CYP2C9 contributing as a minor pathway. Rosiglitazone is extensively metabolized with no unchanged drug excreted in the urine. The major routes of metabolism were N-demethylation and hydroxylation, followed by conjugation with sulfate and glucuronic acid. All the circulating metabolites are considerably less potent than parent and, therefore, are not expected to contribute to the insulin-sensitizing activity of rosiglitazone. Rosiglitazone has known human metabolites that include N-Desmethylrosiglitazone, ortho-hydroxyrosiglitazone, and para-hydroxyrosiglitazone. Biological Half-Life 3-4 hours (single oral dose, independent of dose) The elimination half-life of rosiglitazone was 3-4 hours and was independent of dose. The time to Cmax and the elimination half-life for two metabolites in plasma were significantly longer than for rosiglitazone itself (4-6 hours versus 0.5-1 hours, and about 5 days versus 3-7 hours). The plasma half life of (14)C-related material ranged from 103 to 158 hours. |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
IDENTIFICATION AND USE: Rosiglitazone is a solid. It is used as an antidiabetic agent as an adjunct to diet and exercise to improve glycemic control in patients with type 2 diabetes mellitus. HUMAN STUDIES: Thiazolidinediones, including rosiglitazone, alone or in combination with other antidiabetic agents, can cause fluid retention and may lead to or exacerbate congestive heart failure (CHF). Use of thiazolidinediones is associated with an approximately twofold increased risk of CHF. No evidence of hepatotoxicity has been noted with rosiglitazone in clinical studies to date, including a long-term (4-6 years) study in patients with recently diagnosed type 2 diabetes mellitus. However, hepatitis, elevations in hepatic enzymes to at least 3 times the upper limit of normal, and liver failure with or without fatalities have been reported during postmarketing experience with rosiglitazone. Rosiglitazone was not mutagenic or clastogenic in the in vitro chromosome aberration test in human lymphocytes. ANIMAL STUDIES: Rosiglitazone was not carcinogenic in the mouse. There was an increase in incidence of adipose hyperplasia in the mouse at doses >/= 1.5 mg/kg/day. Heart weights were increased in mice (3 mg/kg/day), rats (5 mg/kg/day), and dogs (2 mg/kg/day) with rosiglitazone treatments. Effects in juvenile rats were consistent with those seen in adults. Morphometric measurement indicated that there was hypertrophy in cardiac ventricular tissues, which may be due to increased heart work as a result of plasma volume expansion. Rosiglitazone had no effects on mating or fertility of male rats given up to 40 mg/kg/day. In juvenile rats dosed from 27 days of age through to sexual maturity (at up to 40 mg/kg/day), there was no effect on male reproductive performance, or on estrous cyclicity, mating performance, or pregnancy incidence in females. Rosiglitazone was not mutagenic or clastogenic in the in vitro bacterial assays for gene mutation, the in vivo mouse micronucleus test, and the in vivo/in vitro rat UDS assay. There was a small (about 2-fold) increase in mutation in the in vitro mouse lymphoma assay in the presence of metabolic activation. Hepatotoxicity In contrast to troglitazone, rosiglitazone is not associated with an increased frequency of aminotransferase elevations during therapy. In clinical trials, ALT elevations above 3 times the ULN occurred in only 0.25% of patients on rosiglitazone, compared to 0.25% of placebo recipients (and 1.9% of troglitazone recipients in similar studies). In addition, clinically apparent liver injury attributed to rosiglitazone is very rare, fewer than a dozen cases having been described in the literature despite extensive use of this agent. The liver injury usually arises between 1 and 12 weeks after starting therapy (thus, a shorter latency than typically occurs with troglitazone) and all patterns of serum enzyme elevations have been described including hepatocellular, cholestatic and mixed. Allergic phenomena are rare and autoantibodies have not been typically present. Fatal instances have been reported usually in cases with a hepatocellular pattern of injury. In most instances, recovery is complete within 1 to 2 months. Likelihood score: C (probable rare cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation No information is available on the clinical use of rosiglitazone during breastfeeding. Rosiglitazone is over 99% protein bound in plasma, so it is unlikely to pass into breastmilk in clinically important amounts. The manufacturer recommends avoiding breastfeeding during rosiglitazone use, so pioglitazone might be a better choice of the drugs in this class for nursing mothers. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding 99.8% bound to plasma proteins, primarily albumin. Interactions An inhibitor of CYP2C8 (e.g., gemfibrozil) may increase the AUC of rosiglitazone and an inducer of CYP2C8 (e.g., rifampin) may decrease the AUC of rosiglitazone. Therefore, if an inhibitor or an inducer of CYP2C8 is started or stopped during treatment with rosiglitazone, changes in diabetes treatment may be needed based upon clinical response. /The authors/ investigated the possible effect of ketoconazole on the pharmacokinetics of rosiglitazone in humans. Ten healthy Korean male volunteers were treated twice daily for 5 days with 200 mg ketoconazole or with placebo, using a randomized, open-label, two-way crossover study. On day 5, a single dose of 8 mg rosiglitazone was administered orally, and plasma rosiglitazone concentrations were measured. Ketoconazole increased the mean area under the plasma concentration-time curve for rosiglitazone by 47%[P = 0.0003; 95% confidence interval (CI) 23, 70] and the mean elimination half-life from 3.55 to 5.50 hr (P = 0.0003; 95% CI in difference 1.1, 2.4). The peak plasma concentration of rosiglitazone was increased by ketoconazole treatment by 17% (P = 0.03; 95% CI 5, 29). The apparent oral clearance of rosiglitazone decreased by 28% after ketoconazole treatment (P = 0.0005; 95% CI 18, 38). This study revealed that ketoconazole affected the disposition of rosiglitazone in humans, probably by the inhibition of CYP2C8 and CYP2C9, leading to increasing rosiglitazone concentrations that could increase the efficacy of rosiglitazone or its adverse events. Endothelial dysfunction is implicated in the initiation and progression of atherosclerosis. Whether atorvastatin combined with rosiglitazone has synergistic effects on endothelial function improvement in the setting of dyslipidemia is unknown. Dyslipidemia rat model was produced with high-fat and high-cholesterol diet administration. Thereafter, atorvastatin, rosiglitazone or atorvastatin combined with rosiglitazone were prescribed for 2 weeks. At baseline, 6 weeks of dyslipidemia model production, and 2 weeks of medical intervention, fasting blood was drawn for parameters of interest evaluation. At the end, myocardium was used for 15-deoxy-delta-12,14-PGJ2 (15-d-PGJ2) assessment. Initially, there was no significant difference of parameters between sham and dyslipidemia groups. With 6 weeks' high-fat and high-cholesterol diet administration, as compared to sham group, serum levels of triglyceride (TG), total cholesterol (TC) and low density lipoprotein-cholesterol (LDL-C) were significantly increased. Additionally, nitric oxide (NO) production was reduced and serum levels of malondialdehyde (MDA), C-reactive protein (CRP) and asymmetric dimethylarginine (ADMA) were profoundly elevated in dyslipidemia group. After 2 weeks' medical intervention, lipid profile was slightly improved in atorvastatin and combined groups as compared to control group. Nevertheless, in comparison to control group, NO production was profoundly increased and serum levels of MDA, CRP and ADMA were significantly decreased with atorvastatin or rosiglitazone therapy. 15-d-PGJ2 expression of myocardium was also significantly elevated with atorvastatin or rosiglitazone treatment. Notably, these effects were further enhanced with combined therapy, suggesting that atorvastatin and rosiglitazone had synergistic effects on endothelial protection, and inflammation and oxidation amelioration. Atorvastatin and rosiglitazone therapy had synergistic effects on endothelium protection as well as amelioration of oxidative stress and inflammatory reaction in rats with dyslipidemia. Avandia (2 mg twice daily) taken concomitantly with glyburide (3.75 to 10 mg/day) for 7 days did not alter the mean steady-state 24-hour plasma glucose concentrations in diabetic patients stabilized on glyburide therapy. Repeat doses of Avandia (8 mg once daily) for 8 days in healthy adult Caucasian subjects caused a decrease in glyburide AUC and Cmax of approximately 30%. In Japanese subjects, glyburide AUC and Cmax slightly increased following coadministration of Avandia. Rifampin administration (600 mg once a day), an inducer of CYP2C8, for 6 days is reported to decrease rosiglitazone AUC by 66%, compared with the administration of rosiglitazone (8 mg) alone. 1. In vitro cytotoxicity: - In PC12/HEK293/RAW264.7 cells: Rosiglitazone up to 20 μM had no significant cytotoxicity (MTT assay: viability >90% vs. control) [3,4,6] - In SKOV3/A2780 cells: Rosiglitazone up to 10 μM alone had no cytotoxicity (viability >85%), but enhanced olaparib-induced apoptosis [7] 2. In vivo toxicity: - In diabetic rats (3 mg/kg/day Rosiglitazone, 8 weeks): No body weight loss (gain 5%–8% vs. diabetic control 4%–6%), serum ALT/AST (35–50 U/L/80–100 U/L) within normal range, no liver/kidney histopathological lesions [5] - In CS-exposed mice (3 mg/kg/day Rosiglitazone, 4 weeks): No mortality, body weight (22–24 g vs. CS control 21–23 g) unchanged, serum BUN/Cr (renal function) normal [6] ; |
| 参考文献 |
|
| 其他信息 |
Therapeutic Uses
Antidiabetic agent /CLINICAL TRIALS/ ClinicalTrials.gov is a registry and results database of publicly and privately supported clinical studies of human participants conducted around the world. The Web site is maintained by the National Library of Medicine (NLM) and the National Institutes of Health (NIH). Each ClinicalTrials.gov record presents summary information about a study protocol and includes the following: Disease or condition; Intervention (for example, the medical product, behavior, or procedure being studied); Title, description, and design of the study; Requirements for participation (eligibility criteria); Locations where the study is being conducted; Contact information for the study locations; and Links to relevant information on other health Web sites, such as NLM's MedlinePlus for patient health information and PubMed for citations and abstracts for scholarly articles in the field of medicine. Rosiglitazone is included in the database. Rosiglitazone is used as monotherapy or in combination with a sulfonylurea, metformin hydrochloride, or a sulfonylurea and metformin as an adjunct to diet and exercise to improve glycemic control in patients with type 2 diabetes mellitus. Rosiglitazone in fixed combination with metformin hydrochloride is used as an adjunct to diet and exercise to improve glycemic control in patients with type 2 diabetes mellitus. Rosiglitazone also is used in fixed combination with glimepiride as an adjunct to diet and exercise for the management of type 2 diabetes mellitus. /Included in US product label/ /EXPL THER/ 1-Methyl-4-phenylpyridinium ion (MPP(+)), an inhibitor of mitochondrial complex I, has been widely used as a neurotoxin because it elicits a severe Parkinson's disease-like syndrome with elevation of intracellular reactive oxygen species (ROS) level and apoptotic death. Rosiglitazone, a peroxisome proliferator-activated receptor (PPAR)-gamma agonist, has been known to show various non-hypoglycemic effects, including anti-inflammatory, anti-atherogenic, and anti-apoptotic. In the present study, /the authors/ investigated the protective effects of rosiglitazone on MPP(+) induced cytotoxicity in human neuroblastoma SH-SY5Y cells, as well as underlying mechanism. /Their/ results suggested that the protective effects of rosiglitazone on MPP(+) induced apoptosis may be ascribed to its anti-oxidative properties, anti-apoptotic activity via inducing expression of SOD and catalase and regulating the expression of Bcl-2 and Bax. These data indicated that rosiglitazone might provide a valuable therapeutic strategy for the treatment of progressive neurodegenerative disease such as Parkinson's disease. Drug Warnings /BOXED WARNING/ WARNING: CONGESTIVE HEART FAILURE. Thiazolidinediones, including rosiglitazone, cause or exacerbate congestive heart failure in some patients. After initiation of Avandia, and after dose increases, observe patients carefully for signs and symptoms of heart failure (including excessive, rapid weight gain; dyspnea; and/or edema). If these signs and symptoms develop, the heart failure should be managed according to current standards of care. Furthermore, discontinuation or dose reduction of Avandia must be considered. Avandia is not recommended in patients with symptomatic heart failure. Initiation of Avandia in patients with established NYHA Class III or IV heart failure is contraindicated. Thiazolidinediones, including rosiglitazone, alone or in combination with other antidiabetic agents, can cause fluid retention and may lead to or exacerbate congestive heart failure (CHF). Use of thiazolidinediones is associated with an approximately twofold increased risk of CHF. Patients should be observed for signs and symptoms of CHF (e.g., dyspnea, rapid weight gain, edema, unexplained cough or fatigue), especially during initiation of therapy and dosage titration. If signs and symptoms of CHF develop, the disorder should be managed according to current standards of care. In addition, a decrease in the dosage of rosiglitazone or discontinuance of the drug should be considered. Thiazolidinedione use is associated with bone loss and fractures in women and possibly in men with type 2 diabetes mellitus. In long-term comparative clinical trials in patients with type 2 diabetes mellitus, the incidence of bone fracture was increased in patients (particularly women) receiving rosiglitazone versus comparator agents (glyburide and/or metformin). Such effects were noted after the first year of treatment and persisted throughout the study. The majority of fractures observed in patients taking thiazolidinediones were in a distal upper limb (i.e., forearm, hand, wrist) or distal lower limb (i.e., foot, ankle, fibula, tibia). In an observational study in the United Kingdom in men and women (mean age: 60.7 years) with diabetes mellitus, use of pioglitazone or rosiglitazone for approximately 12-18 months (as estimated from prescription records) was associated with a twofold to threefold increase in fractures, particularly of the hip and wrist. The overall risk of fracture was similar among men and women and was independent of body mass index, comorbid conditions, diabetic complications, duration of diabetes mellitus, and use of other oral antidiabetic drugs.145 Risk of fractures should be considered when initiating or continuing thiazolidinedione therapy in female patients with type 2 diabetes mellitus. Bone health should be assessed and maintained according to current standards of care. Although increased risk of fracture may also apply to men, the risk appears to be higher among women than men. Because rosiglitazone requires endogenous insulin for activity, it should not be used in patients with type 1 diabetes mellitus or diabetic ketoacidosis. For more Drug Warnings (Complete) data for Rosiglitazone (19 total), please visit the HSDB record page. Pharmacodynamics When rosiglitazone is used as monotherapy, it is associated with increases in total cholesterol, LDL, and HDL. It is also associated with decreases in free fatty acids. Increases in LDL occurred primarily during the first 1 to 2 months of therapy with AVANDIA and LDL levels remained elevated above baseline throughout the trials. In contrast, HDL continued to rise over time. As a result, the LDL/HDL ratio peaked after 2 months of therapy and then appeared to decrease over time. 1. Mechanism of action: - Antidiabetic: Activates PPARγ to promote adipocyte differentiation, enhance insulin sensitivity in muscle/liver, reduce insulin resistance [1,2,5] - Neuroprotective: PPARγ-mediated NTF-α1 transcription inhibits neuronal apoptosis [3] - Anti-airway inflammation: Activates PPARγ/RXRα heterodimer to suppress M1 macrophage polarization (reduces iNOS/TNF-α/IL-6) [6] - Anticancer adjuvant: Inhibits AKT/mTOR pathway via PPARγ, reverses olaparib-induced ovarian cancer cell senescence, promotes apoptosis [7] - Ion channel regulation: Contrasting effects on TRPM3 (inhibition) and TRPC5 (activation) via non-PPARγ mechanisms [4] 2. Structure-activity relationship (SAR): - The thiazolidinedione ring of Rosiglitazone is essential for PPARγ binding—removal abolishes agonism. The p-methoxybenzyl group enhances binding affinity; methyl substitution increases EC50 by 5-fold [2] 3. Therapeutic potential: - Indicated for type 2 diabetes mellitus (T2DM), especially insulin-resistant patients; combination with losartan improves diabetic nephropathy [5] - Potential for chronic obstructive pulmonary disease (COPD) via reducing CS-induced airway inflammation [6] - Adjuvant for ovarian cancer treatment (enhances olaparib efficacy by reversing senescence) [7] - Neurodegenerative disease potential (Parkinson’s disease) via neuroprotection [3] ; |
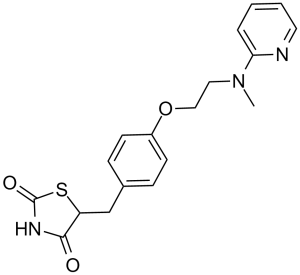
| 分子式 |
C18H19N3O3S
|
|---|---|
| 分子量 |
357.43
|
| 精确质量 |
357.114
|
| 元素分析 |
C, 60.49; H, 5.36; N, 11.76; O, 13.43; S, 8.97
|
| CAS号 |
122320-73-4
|
| 相关CAS号 |
Rosiglitazone maleate;155141-29-0;Rosiglitazone hydrochloride;302543-62-0;Rosiglitazone potassium;316371-84-3;Rosiglitazone-d3;1132641-22-5
|
| PubChem CID |
77999
|
| 外观&性状 |
Colorless crystals from methanol
|
| 密度 |
1.3±0.1 g/cm3
|
| 沸点 |
585.0±35.0 °C at 760 mmHg
|
| 熔点 |
153-155ºC
|
| 闪点 |
307.6±25.9 °C
|
| 蒸汽压 |
0.0±1.6 mmHg at 25°C
|
| 折射率 |
1.642
|
| LogP |
2.56
|
| tPSA |
96.83
|
| 氢键供体(HBD)数目 |
1
|
| 氢键受体(HBA)数目 |
6
|
| 可旋转键数目(RBC) |
7
|
| 重原子数目 |
25
|
| 分子复杂度/Complexity |
469
|
| 定义原子立体中心数目 |
0
|
| SMILES |
S1C(N([H])C(C1([H])C([H])([H])C1C([H])=C([H])C(=C([H])C=1[H])OC([H])([H])C([H])([H])N(C([H])([H])[H])C1=C([H])C([H])=C([H])C([H])=N1)=O)=O
|
| InChi Key |
YASAKCUCGLMORW-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C18H19N3O3S/c1-21(16-4-2-3-9-19-16)10-11-24-14-7-5-13(6-8-14)12-15-17(22)20-18(23)25-15/h2-9,15H,10-12H2,1H3,(H,20,22,23)
|
| 化学名 |
5-(4-(2-(methyl(pyridin-2-yl)amino)ethoxy)benzyl)thiazolidine-2,4-dione
|
| 别名 |
HSDB7555; TDZ 01; HSDB 7555; HSDB-7555; BRL 49653; BRL49653; BRL-49653; TDZ-01; TDZ01; Rosiglitazone. trade name Avandia; rosiglitazone; 122320-73-4; Avandia; Rosiglizole; 5-(4-(2-(Methyl(pyridin-2-yl)amino)ethoxy)benzyl)thiazolidine-2,4-dione; Brl-49653; Brl 49653; Rezult; .
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: 2.5 mg/mL (6.99 mM) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 悬浮液;超声助溶。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL 澄清 DMSO 储备液加入900 μL 玉米油中,混合均匀。 配方 2 中的溶解度: ≥ 2.5 mg/mL (6.99 mM) (饱和度未知) in 5% DMSO + 40% PEG300 + 5% Tween80 + 50% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (6.99 mM) (饱和度未知) in 5% DMSO + 95% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 配方 4 中的溶解度: ≥ 2.08 mg/mL (5.82 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将100 μL 20.8 mg/mL澄清的DMSO储备液加入400 μL PEG300中,混匀;再向上述溶液中加入50 μL Tween-80,混匀;然后加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 5 中的溶解度: ≥ 2.08 mg/mL (5.82 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将100μL 20.8mg/mL澄清的DMSO储备液加入到900μL 20%SBE-β-CD生理盐水中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 配方 6 中的溶解度: 4% DMSO+30% PEG 300+5% Tween 80+ddH2O: 5mg/mL 配方 7 中的溶解度: 10 mg/mL (27.98 mM) in 0.5% CMC-Na/saline water (这些助溶剂从左到右依次添加,逐一添加), 悬浊液; 超声助溶。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.7978 mL | 13.9888 mL | 27.9775 mL | |
| 5 mM | 0.5596 mL | 2.7978 mL | 5.5955 mL | |
| 10 mM | 0.2798 mL | 1.3989 mL | 2.7978 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT01100619 | Completed | Drug: rosiglitazone Drug: XL184 |
Papillary Thyroid Cancer Follicular Thyroid Cancer |
Exelixis | April 2010 | Phase 1 |
| NCT01706211 | Completed | Drug: BRL 49653C Drug: Placebo |
Diabetes Mellitus Non Insulin Dependent Oral Agent Therapy |
National Taiwan University Hospital | October 1998 | Phase 3 |
| NCT02694874 | Completed | Drug: Rosiglitazone Drug: Placebo |
Malaria | Centro de Investigacao em Saude de Manhica |
February 2016 | Not Applicable |
| NCT00785213 | Completed Has Results | Drug: Rosiglitazone 4 mg Tablets Drug: Quinine Sulfate 324 mg Capsules |
Healthy | Mutual Pharmaceutical Company, Inc. | September 2008 | Phase 1 |
 |
|---|
|
|
|
|---|
|
|