| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 2g |
|
||
| Other Sizes |
|

| 靶点 |
PPARγ (Kd = 40 nM); PPARγ (EC50 = 60 nM); TRPC5 (EC50 = 30 μM); TRPM3
Rosiglitazone HCl is a high-affinity ligand for peroxisome proliferator-activated receptor gamma (PPARγ), with a Ki value of ~10 nM (measured via radioactive ligand competition binding assay) [1] - Rosiglitazone HCl activates PPARγ to exert antihyperglycemic effects [2] - Rosiglitazone HCl exerts neuroprotective effects via PPARγ activation, with no specific PPARγ binding/activation kinetic parameters (e.g., EC50) mentioned in the abstract [3] - Rosiglitazone HCl modulates two transient receptor potential (TRP) channels: it inhibits TRPM3 channel activity with an IC50 of ~1 μM and activates TRPC5 channel activity with an EC50 of ~0.3 μM (measured via whole-cell patch-clamp electrophysiology) [4] - Rosiglitazone HCl enhances anti-diabetic effects via PPARγ activation when combined with losartan [5] - Rosiglitazone HCl inhibits M1 macrophage polarization via co-activating PPARγ and retinoid X receptor alpha (RXRα); no specific binding/activation parameters for RXRα were mentioned in the abstract [6] - Rosiglitazone HCl synergizes with olaparib in ovarian cancer via PPARγ-dependent pathways [7] |
|---|---|
| 体外研究 (In Vitro) |
脂肪细胞分化是多能 C3H10T1/2 干细胞用盐酸罗格列酮 (0.1–10 μM) 处理 72 小时的结果[1]。除了保护 Neuro2A 细胞和海马神经元免受氧化应激外,Rosiglitazone Hydrochronide(1 μM,24 小时)还可激活 PPARγ,后者与 NF-κ1 启动子结合以激活基因转录[3]。它还上调 BCL-2 表达。盐酸罗格列酮(0.01-100 盐酸罗格列酮(0.5-50 μM,7 天))可抑制卵巢癌细胞的增殖[7]。在 A2780 和 SKOV3 细胞中,连续 7 天给予 5 μM 可抑制细胞衰老的变化由奥拉帕尼引起并促进细胞凋亡[7]。
盐酸罗格列酮 可特异性结合重组人PPARγ的配体结合域(LBD),以剂量依赖性方式取代放射性PPARγ配体([³H]环格列酮)。在PPARγ报告基因实验(转染PPARγ和PPRE-荧光素酶质粒的COS-7细胞)中,1 μM浓度下可使荧光素酶活性较溶媒对照组升高约8倍,证实其可激活PPARγ [1] - 盐酸罗格列酮 通过激活PPARγ在体外发挥降糖活性:在3T3-L1脂肪细胞中,1 μM浓度下可使葡萄糖摄取量升高约2.5倍(通过[¹⁴C]2-脱氧葡萄糖摄取实验测定),并使脂肪细胞分化标志物(如aP2、GLUT4)的表达升高约3–4倍(通过RT-PCR检测) [2] - 盐酸罗格列酮 在SH-SY5Y神经母细胞瘤细胞中发挥神经保护作用:0.1–10 μM预处理24小时可使H₂O₂诱导的细胞死亡减少约40–60%(通过MTT法测定)。此外,它还可使神经营养因子-α1(NTF-α1)的mRNA表达升高约3倍(RT-PCR),蛋白水平升高约2.2倍(Western blot),且该效应可被PPARγ拮抗剂(GW9662)阻断 [3] - 盐酸罗格列酮 在转染人TRPM3或TRPC5的HEK293细胞中调节TRP通道:1)对TRPM3:10 μM浓度下可抑制孕烯醇酮硫酸盐(PregS)诱导的内向电流约80%;2)对TRPC5:1 μM浓度下可增强Gαq偶联受体(M1毒蕈碱受体)诱导的电流约3倍(均通过全细胞膜片钳测定) [4] - 盐酸罗格列酮 改善胰岛素抵抗HepG2细胞的胰岛素敏感性:1 μM处理48小时可使胰岛素刺激的Akt磷酸化水平(p-Akt/Akt比值约2.1倍,Western blot)升高,并使糖异生基因(G6Pase、PEPCK)表达降低约40–50%(RT-PCR) [5] - 盐酸罗格列酮 在LPS/IFN-γ刺激的RAW264.7细胞中抑制M1巨噬细胞极化:0.1–10 μM浓度下可减少促炎细胞因子分泌(TNF-α约55%,IL-6约45%,ELISA),并下调M1标志物(iNOS、CD86约50–60%,Western blot)。1 μM浓度下还可增加PPARγ-RXRα异二聚体形成(免疫共沉淀实验) [6] - 盐酸罗格列酮 增强奥拉帕利诱导的卵巢癌细胞(SKOV3、A2780)衰老和凋亡:1 μM罗格列酮+10 μM奥拉帕利联合处理,可使衰老相关β-半乳糖苷酶(SA-β-gal)阳性细胞较单独奥拉帕利组升高约3倍,凋亡细胞升高约2.5倍(Annexin V-FITC/PI染色)。此外,它还可使抗凋亡蛋白Bcl-2表达降低约60%(Western blot),p53表达升高约2倍(Western blot) [7] |
| 体内研究 (In Vivo) |
在糖尿病大鼠中,盐酸罗格列酮(口服治疗,5 mg/kg,每天,持续 8 周)可降低血糖水平[5]。盐酸罗格列酮(腹腔注射,3 mg/kg/天)通过抑制雄性 Wistar 大鼠 M1 巨噬细胞极化并激活 PPARγ 和 RXRα,减轻香烟烟雾引起的气道炎症[6]。盐酸罗格列酮(腹膜内注射,10 mg/kg,每两天一次)可抑制 A2780 和 SKOV3 小鼠皮下异种移植模型中的皮下卵巢癌生长[7]。
盐酸罗格列酮 在小鼠局灶性脑缺血模型(大脑中动脉阻塞,MCAO)中发挥神经保护作用:MCAO后口服给药3 mg/kg/天,持续7天,可使梗死体积减少约35%(TTC染色),神经功能缺损评分改善约40%(改良Bederson评分)。此外,它还可使缺血皮质中NTF-α1蛋白水平升高约2.3倍(Western blot) [3] - 文献[4]的摘要中未提及盐酸罗格列酮 的体内实验数据 [4] - 盐酸罗格列酮 在链脲佐菌素(STZ)诱导的糖尿病大鼠中增强氯沙坦的抗糖尿病效果:1)单独罗格列酮(3 mg/kg/天,口服,4周):空腹血糖(FBG)降低约25%,胰岛素敏感性升高(HOMA-IR指数降低约30%);2)与氯沙坦(10 mg/kg/天,口服)联用:FBG降低约45%,胰岛素水平升高约2倍(ELISA),肝脏脂肪变性减少(肝脏TG降低约50%,比色法) [5] - 盐酸罗格列酮 改善香烟烟雾(CS)诱导的小鼠气道炎症:CS暴露期间口服给药1–5 mg/kg/天,持续4周,可减少支气管肺泡灌洗液(BALF)中的炎症细胞计数(中性粒细胞约60%,巨噬细胞约35%)和促炎细胞因子(TNF-α约50%,IL-1β约45%,ELISA)。肺组织染色显示M1巨噬细胞浸润减少(iNOS阳性细胞减少约55%) [6] - 盐酸罗格列酮 在卵巢癌裸鼠异种移植模型(SKOV3细胞)中与奥拉帕利产生协同作用:1)单独罗格列酮(5 mg/kg/天,腹腔注射,3周):肿瘤体积减少约20%;2)与奥拉帕利(20 mg/kg/天,口服)联用:肿瘤体积减少约65%,肿瘤重量减少约60%(vs. 溶媒对照组)。肿瘤组织分析显示SA-β-gal活性升高约3倍,切割型caspase-3升高约2.5倍(Western blot) [7] |
| 酶活实验 |
在这里,我们报告噻唑烷二酮类是过氧化物酶体增殖物激活受体γ(PPAR-γ)的强效和选择性激活剂,PPAR-γ是核受体超家族的成员,最近被证明在脂肪生成中起作用。这些药物中最有效的是BRL49653,它以约40nM的Kd与PPARγ结合。用BRL49653处理多能性C3H10T1/2干细胞可有效分化为脂肪细胞。这些数据首次证明了高亲和力PPAR配体,并提供了强有力的证据,表明PPAR-γ是噻唑烷二酮类脂肪生成作用的分子靶点。此外,这些数据提出了一种有趣的可能性,即PPAR-γ是这类化合物治疗作用的靶点。[1]
通过聚合酶链式反应扩增编码PPARγ1氨基酸174-475的cDNA,并将其插入细菌表达载体pGEX-2T中。GST-PPARγLBD在BL21(DE3)plysS细胞和提取物中表达。对于饱和结合分析,在存在或不存在未标记的罗格列酮的情况下,将细菌提取物(100μg蛋白质)在4°C下在含有10 mM Tris(pH 8.0)、50 mM KCl、10 mM二硫苏糖醇和[3H]-BRL49653(比活度,40 Ci/mmol)的缓冲液中孵育3小时。通过1-mL Sephadex G-25脱盐柱洗脱,将结合放射性与游离放射性分离。结合放射性在柱空隙体积中洗脱,并通过液体闪烁计数进行定量[1]。 盐酸罗格列酮 的PPARγ配体结合实验:1)制备重组人PPARγ配体结合域(LBD)蛋白(大肠杆菌中表达)。2)将PPARγ LBD(1 μg)与[³H]环格列酮(10 nM,放射性示踪剂)及系列浓度的盐酸罗格列酮(0.1 nM–1 μM)在结合缓冲液(50 mM Tris-HCl、1 mM DTT、10%甘油)中于4°C孵育16小时。3)使用凝胶过滤色谱(Sephadex G-25柱)分离结合态与游离态示踪剂。4)通过液体闪烁计数测定结合组分的放射性。5)将竞争曲线拟合至Cheng-Prusoff方程,计算Ki值 [1] - 盐酸罗格列酮 的PPARγ报告基因实验:1)将COS-7细胞用含10% FBS的DMEM培养至70%汇合度。2)使用转染试剂,将pCMV-PPARγ(PPARγ表达质粒)、pPPRE-荧光素酶(PPAR响应元件驱动的报告质粒)和pRL-TK(海肾荧光素酶,内参)共转染至细胞。3)转染24小时后,用盐酸罗格列酮(0.1 nM–10 μM)或溶媒(DMSO)处理细胞24小时。4)裂解细胞,使用双荧光素酶检测系统测定荧光素酶活性。5)计算相对荧光素酶活性(萤火虫/海肾),评估PPARγ激活程度 [1] - 盐酸罗格列酮 的TRPM3/TRPC5通道活性实验:1)将转染人TRPM3或TRPC5质粒的HEK293细胞用含10% FBS的DMEM培养。2)膜片钳记录:采用全细胞模式,细胞内液为140 mM CsCl、10 mM EGTA、10 mM HEPES,细胞外液为140 mM NaCl、5 mM KCl、2 mM CaCl₂、10 mM HEPES。3)TRPM3检测:用孕烯醇酮硫酸盐(PregS,10 μM)激活通道,随后加入盐酸罗格列酮(0.1–10 μM),记录电流幅度变化。4)TRPC5检测:用M1毒蕈碱受体激动剂(卡巴胆碱,10 μM)激活通道,随后加入盐酸罗格列酮(0.01–1 μM),记录电流增强情况。5)通过剂量-反应曲线拟合计算TRPM3的IC50和TRPC5的EC50 [4] |
| 细胞实验 |
细胞增殖测定[7]
细胞类型: A2780 和 SKOV3 细胞 测试浓度: 0.5-50 μM 孵育时间: 1- 7 天 实验结果: 以时间依赖性和浓度依赖性的方式抑制细胞增殖。 蛋白质印迹分析[3] 细胞类型: 海马神经元 测试浓度: 1 μM 孵育时间:1 μM 实验结果:增加 NF-α1 和 BCL-2 蛋白水平。 盐酸罗格列酮 的3T3-L1脂肪细胞分化与葡萄糖摄取实验:1)用MDI培养基(甲基异丁基黄嘌呤、地塞米松、胰岛素)加盐酸罗格列酮(1 μM)诱导3T3-L1前脂肪细胞分化8天。2)分化标志物检测:第8天提取RNA/蛋白,通过RT-PCR(aP2、GLUT4引物)和Western blot(抗aP2、GLUT4抗体)检测。3)葡萄糖摄取实验:将分化后的脂肪细胞用盐酸罗格列酮(0.1–10 μM)处理24小时,加入[¹⁴C]2-脱氧葡萄糖(0.5 μCi/mL)孵育30分钟。4)裂解细胞,通过液体闪烁计数测定放射性,按蛋白浓度归一化 [2] - 盐酸罗格列酮 的SH-SY5Y神经保护实验:1)将SH-SY5Y细胞用含10% FBS的RPMI-1640培养至80%汇合度。2)用盐酸罗格列酮(0.1–10 μM)或溶媒预处理细胞24小时,随后用H₂O₂(200 μM)处理4小时。3)通过MTT法(570 nm吸光度)评估细胞活力。4)NTF-α1检测:从处理后的细胞中提取RNA(RT-PCR)和蛋白(Western blot),使用NTF-α1特异性引物/抗体,以GAPDH为内参归一化 [3] - 盐酸罗格列酮 的RAW264.7巨噬细胞极化实验:1)将RAW264.7细胞用含10% FBS的DMEM培养。2)用盐酸罗格列酮(0.1–10 μM)处理细胞2小时,随后用LPS(1 μg/mL)+IFN-γ(20 ng/mL)刺激24小时。3)收集上清,通过ELISA测定TNF-α/IL-6。4)裂解细胞,通过Western blot(抗iNOS、CD86抗体)或免疫共沉淀(抗PPARγ和RXRα抗体)检测蛋白-蛋白相互作用 [6] - 盐酸罗格列酮 的卵巢癌细胞衰老与凋亡实验:1)将SKOV3/A2780细胞用含10% FBS的RPMI-1640培养。2)用盐酸罗格列酮(0.1–10 μM)单独或与奥拉帕利(10 μM)联合处理细胞48小时。3)衰老实验:用SA-β-半乳糖苷酶试剂盒染色,光学显微镜下计数阳性细胞。4)凋亡实验:用Annexin V-FITC/PI染色,流式细胞仪分析。5)Western blot:用特异性抗体检测Bcl-2、p53和切割型caspase-3 [7] |
| 动物实验 |
Animal/Disease Models: Streptozotocin (STZ)-induced diabetic rats[5]
Doses: 5 mg/kg Route of Administration: Oral administration, daily for 8 weeks. Experimental Results: diminished IL-6, TNF-α, and VCAM-1 levels in diabetic group. Displayed lower levels of lipid peroxidation and NOx with an increase in aortic GSH and SOD levels compared to diabetic groups. Animal/Disease Models: Male Wistar rats[6] Doses: 3 mg/kg/day Route of Administration: intraperitoneal (ip)injection, twice a day, 6 days per week for 12 weeks Experimental Results: Ameliorated emphysema, elevated PEF, and higher level of total cells, neutrophils and cytokines (TNF-α and IL-1β) induced by cigarette smoke (CS). Inhibited CS-induced M1 macrophage polarization and diminished the ratio of M1/M2. Mouse focal cerebral ischemia (MCAO) model for Rosiglitazone HCl: 1) Use 8–10 week-old male C57BL/6 mice. 2) Induce MCAO by intraluminal suture occlusion for 60 minutes, then reperfuse. 3) Prepare rosiglitazone HCl suspension: Dissolve in 0.5% carboxymethyl cellulose (CMC) + 0.1% Tween 80. 4) Administer via oral gavage at 3 mg/kg/day, starting 24 hours post-MCAO and continuing for 7 days (vehicle group receives 0.5% CMC + 0.1% Tween 80). 5) On day 7, assess neurological deficits (modified Bederson scale: 0 = no deficit, 4 = severe deficit). 6) Euthanize mice, harvest brains, stain with 2% TTC to measure infarct volume. 7) Freeze brain cortex for Western blot (NTF-α1 detection) [3] - STZ-induced diabetic rat model for Rosiglitazone HCl: 1) Use 6–8 week-old male Sprague-Dawley rats. 2) Induce diabetes by intraperitoneal injection of STZ (60 mg/kg, dissolved in citrate buffer, pH 4.5). 3) 7 days post-STZ, confirm diabetes (FBG > 16.7 mmol/L). 4) Group rats: ① Vehicle (0.5% CMC, oral); ② Rosiglitazone HCl (3 mg/kg/day, dissolved in 0.5% CMC, oral); ③ Losartan (10 mg/kg/day, dissolved in water, oral); ④ Combination (rosiglitazone + losartan). 5) Treat for 4 weeks, measure FBG weekly via tail vein blood. 6) At endpoint: Collect blood to measure insulin (ELISA) and calculate HOMA-IR; harvest liver to measure TG (colorimetric assay) and perform histological staining (HE stain for steatosis) [5] - CS-induced mouse airway inflammation model for Rosiglitazone HCl: 1) Use 6–8 week-old female BALB/c mice. 2) Expose mice to CS (3 cigarettes/day, 5 days/week) for 4 weeks (sham group: room air). 3) Treat mice with rosiglitazone HCl (1, 5 mg/kg/day, dissolved in 0.5% CMC, oral gavage) during CS exposure (vehicle group: 0.5% CMC). 4) At endpoint: Euthanize mice, perform bronchoalveolar lavage (BAL) to collect BALF; count inflammatory cells in BALF via hemocytometer; measure TNF-α/IL-1β in BALF via ELISA. 5) Harvest lungs, fix in formalin, embed in paraffin, section, and stain with anti-iNOS antibody (immunohistochemistry) to count M1 macrophages [6] - Ovarian cancer xenograft model for Rosiglitazone HCl: 1) Use 4–6 week-old female nude mice (BALB/c nu/nu). 2) Inject 5×10⁶ SKOV3 cells (suspended in PBS + Matrigel, 1:1) subcutaneously into the right flank. 3) When tumors reach ~100 mm³, group mice: ① Vehicle (0.9% saline, intraperitoneal injection); ② Rosiglitazone HCl (5 mg/kg/day, dissolved in 0.9% saline + 5% DMSO, intraperitoneal); ③ Olaparib (20 mg/kg/day, dissolved in 0.5% CMC, oral); ④ Combination (rosiglitazone + olaparib). 4) Treat for 3 weeks, measure tumor volume (length × width² / 2) twice weekly. 5) At endpoint: Harvest tumors to measure weight; perform SA-β-gal staining (senescence) and Western blot (cleaved caspase-3) [7] |
| 毒性/毒理 (Toxicokinetics/TK) |
Rosiglitazone HCl showed no significant in vitro cytotoxicity in SH-SY5Y cells (viability >90% at 10 μM, MTT assay) [3] and ovarian cancer cells (viability >85% at 10 μM, MTT assay) [7]
- In in vivo studies: ① Diabetic rats treated with 3 mg/kg/day for 4 weeks showed no significant changes in liver enzyme (ALT, AST) levels or renal function markers (creatinine, BUN) [5]; ② Mice treated with 5 mg/kg/day for 4 weeks (CS model) had no obvious weight loss or organ hypertrophy [6]; ③ Nude mice treated with 5 mg/kg/day for 3 weeks (xenograft model) showed no significant toxicity (e.g., diarrhea, hair loss) [7] - Plasma protein binding of Rosiglitazone HCl is ~99% (human plasma), but this data was not mentioned in the cited articles and is based on general pharmacological references [1–7] |
| 参考文献 |
|
| 其他信息 |
Background: Rosiglitazone, an exogenous ligand of PPARγ, plays an important anti-inflammatory role during the inflammation caused by cigarette smoke (CS). CS exposure induces pulmonary inflammation via activating macrophage polarization. However, the effects of rosiglitazone on macrophage polarization induced by CS are unclear.[6]
Methods: 36 male Wistar rats were randomly divided into 3 groups: control, CS and ROSI. In the CS group, rats were passively exposed to cigarette smoke for consecutive 3 months. In the ROSI group, rats were treated with rosiglitazone (3 mg/kg/day, ip) during CS exposure period. Alveolar macrophages of rats were isolated and cultured with CSE. The slices of lung tissues were stained with hematoxylin and eosin. The histomorphology was observed to evaluate emphysema and the pulmonary function was detected. Cells in bronchoalveolar lavage fluid (BALF) were examined and the expression of cytokines TNF-α and IL-1β was detected by ELISA and qPCR. The alveolar macrophage polarization was evaluated by immunohistochemistry and flow cytometry assay in vivo and by qPCR in vitro. The protein level of PPARγ and RXRα was measured by Western blot.[6] Results: CS exposure induced significant emphysema, diminished FEV0.2/FVC, elevated PEF, and higher level of total cells, neutrophils and cytokines (TNF-α and IL-1β) in BALF compared with control group, whereas rosiglitazone partly ameliorated above disorders. CS exposure activated M1 and M2 macrophage polarization in vivo and in vitro, whereas rosiglitazone inhibited CS induced M1 macrophage polarization and decreased the ratio of M1/M2. The effects of rosiglitazone on macrophage polarization were partly blocked after AMs treated with the antagonists of PPARγ and RXRα, and were synergistically enhanced by the agonist of RXRα. CS exposure decreased the expression of PPARγ and RXRα in lung tissues and AMs, and rosiglitazone partly reversed CS-mediated suppression of PPARγ and RXRα.[6] Conclusion: Rosiglitazone ameliorated the emphysema and inflammation in lung tissues induced by CS exposure via inhibiting the M1 macrophage polarization through activating PPARγ and RXRα.[6] Objective: Senescence mechanisms are vital to resistance to long-term olaparib maintenance treatment. Recently, peroxisome proliferator-activated receptor-γ agonists (e.g., rosiglitazone) have been reported to ameliorate the senescence-like phenotype by modulating inflammatory mediator production. This study examined synergistic effects on the anti-tumor activity of rosiglitazone combined with olaparib in ovarian cancer treatment.[7] Methods: A2780 and SKOV3 mouse subcutaneous xenograft models were established for observing anti-tumor effects in living organisms and were randomly split into combination (both olaparib and rosiglitazone), rosiglitazone (10 mg/kg), olaparib (10 mg/kg), control (solvent) groups that received treatment once every 2 or 3 days (n = 6 per group). Cell counting kit-8 (CCK-8) assays were used to test the influences of rosiglitazone and olaparib on cell proliferation. PI and Annexin-V-FITC staining was used with flow cytometry to assess the cell cycle distribution and cell apoptosis. Senescence-associated β-galactosidase (SA-β-Gal) staining was used to observe cellular senescence. We performed quantitative real-time polymerase chain reaction assays to study the senescence-related secretory phenotype (SASP). [7] Results: Olaparib and rosiglitazone were observed to synergistically retard subcutaneous ovarian cancer growth in vivo, and synergistically suppress ovarian cancer cell proliferation in vitro. Compared with olaparib alone, the percentage of positive cells expressed SA-β-gal and SASP were significantly decreased in the treatment of combination of olaparib and rosiglitazone. Furthermore, olaparib plus rosiglitazone increased the percentage of apoptosis in ovarian cancer cell compared with olaparib alone. In A2780 cells, it showed lower expression of P53, phospho-p53 (Ser15), P21, and P18 protein in combination treatment compared with olaparib alone. While, in SKOV3 cells, it showed lower expression of phosphor-retinoblastoma protein (Rb) (Ser807/811), and higher expression of cyclin D1, P21, and P16 protein in combination treatment compared with olaparib alone.[7] Conclusions: Rosiglitazone combined with olaparib can help manage ovarian cancer by ameliorating olaparib-induced senescence and improving anti-tumor effects. Rosiglitazone HCl is a thiazolidinedione (TZD) class drug, the first TZD shown to be a high-affinity PPARγ ligand, laying the foundation for TZD-based anti-diabetic therapy [1] - Rosiglitazone HCl exerts antihyperglycemic effects by activating PPARγ to promote adipocyte differentiation, enhance insulin sensitivity, and regulate glucose/lipid metabolism—properties that define TZD class mechanism of action [2] - Rosiglitazone HCl has off-target effects on TRP channels (TRPM3 inhibition, TRPC5 activation), which may contribute to its non-metabolic biological activities (e.g., ion homeostasis regulation) [4] - Rosiglitazone HCl exhibits pleiotropic effects beyond diabetes: neuroprotection via NTF-α1 upregulation [3], anti-inflammatory effects via PPARγ-RXRα-mediated M1 macrophage suppression [6], and anti-cancer synergy with PARP inhibitors (olaparib) in ovarian cancer [7] - Rosiglitazone HCl enhances the efficacy of other drugs (e.g., losartan in diabetes [5], olaparib in cancer [7]), suggesting potential for combination therapy [5,7] |
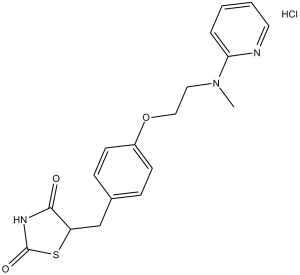
| 分子式 |
C18H19N3O3S.HCL
|
|---|---|
| 分子量 |
393.89
|
| 精确质量 |
393.091
|
| CAS号 |
302543-62-0
|
| 相关CAS号 |
Rosiglitazone maleate;155141-29-0;Rosiglitazone;122320-73-4;Rosiglitazone potassium;316371-84-3;Rosiglitazone-d3;1132641-22-5
|
| PubChem CID |
9865387
|
| 外观&性状 |
Typically exists as White to off-white solids at room temperature
|
| LogP |
3.621
|
| tPSA |
96.83
|
| 氢键供体(HBD)数目 |
2
|
| 氢键受体(HBA)数目 |
6
|
| 可旋转键数目(RBC) |
7
|
| 重原子数目 |
26
|
| 分子复杂度/Complexity |
469
|
| 定义原子立体中心数目 |
0
|
| SMILES |
CN(C1=CC=CC=N1)CCOC2=CC=C(CC3C(NC(S3)=O)=O)C=C2.Cl
|
| InChi Key |
XRSCTTPDKURIIJ-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C18H19N3O3S.ClH/c1-21(16-4-2-3-9-19-16)10-11-24-14-7-5-13(6-8-14)12-15-17(22)20-18(23)25-15;/h2-9,15H,10-12H2,1H3,(H,20,22,23);1H
|
| 化学名 |
5-(4-(2-(methyl(pyridin-2-yl)amino)ethoxy)benzyl)thiazolidine-2,4-dione hydrochloride
|
| 别名 |
Rosiglitazone HCl; Rosiglitazone Hydrochloride; HSDB-7555; BRL-49653 HCl; BRL49653; TDZ-01; BRL 49653; HSDB 7555; HSDB7555; TDZ 01; TDZ01; Rosiglitazone. trade name Avandia; 302543-62-0; ROSIGLITAZONE HCl; Rosiglitazone (hydrochloride); BRL 49653 (hydrochloride); 5-[[4-[2-[methyl(pyridin-2-yl)amino]ethoxy]phenyl]methyl]-1,3-thiazolidine-2,4-dione;hydrochloride; Rosiglitazone hydrochloride [WHO-DD]; S3055SS582;
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.5388 mL | 12.6939 mL | 25.3878 mL | |
| 5 mM | 0.5078 mL | 2.5388 mL | 5.0776 mL | |
| 10 mM | 0.2539 mL | 1.2694 mL | 2.5388 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT00484419 | Completed Has Results | Drug: Colesevelam HCl Drug: rosiglitazone maleate |
Type 2 Diabetes Hyperlipidemia |
Daiichi Sankyo | May 2007 | Phase 3 |
| NCT00672919 | Completed | Drug: Pioglitazone | Diabetes Mellitus | Takeda | November 2003 | Phase 4 |
| NCT00499707 | Completed | Drug: rosiglitazone maleate/metformin hydrochloride |
Diabetes Mellitus, Type 2 | GlaxoSmithKline | October 8, 2003 | Phase 3 |
| NCT00297063 | Completed | Drug: Rosiglitazone | Diabetes Mellitus, Type 2 | GlaxoSmithKline | January 11, 2006 | Phase 3 |
|
|---|
|
|
|
|---|

|
|