| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10 mM * 1 mL in DMSO |
|
||
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| Other Sizes |

| 靶点 |
Neprilysin (NEP) (IC₅₀ = 5 nM) [1,4]
- NEP Inhibition: Sacubitril (AHU-377) potently inhibited recombinant human NEP with an IC₅₀ of 5 nM, measured using a fluorescence resonance energy transfer (FRET) assay. The active metabolite LBQ657 showed comparable activity (IC₅₀ = 3 nM) [1,4] - Natriuretic Peptide Stabilization: In human plasma, Sacubitril (10 μM) increased the half-life of atrial natriuretic peptide (ANP) from 2.1 to 6.8 minutes, consistent with NEP inhibition [4] The compound sacubitril (AHU-377) is a neprilysin inhibitor that is composed of the molecular moieties of valsartan (an ARB) and sacubitril (AHU-377) in a 1:1 ratio. Sacubitril (AHU-377) undergoes enzymatic cleavage of the ethyl ester to generate the active enkephalinase-inhibiting metabolite LBQ657 [2]. There is no inhibition of collagen formation in fibroblasts or cardiomyocyte hypertrophy by the inactive NEPi precursor Sacubitril (AHU-377). Active NEPi LBQ657 did not appear to have any effect on cardiac fibroblasts. Conversely, LBQ657 inhibits cardiomyocyte hypertrophy to a moderate extent [3]. |
|---|---|
| 体外研究 (In Vitro) |
- NEP抑制活性:沙库巴曲(AHU-377)通过荧光共振能量转移(FRET)实验显示,对重组人NEP的IC₅₀为5 nM,其活性代谢产物LBQ657活性相当(IC₅₀ = 3 nM)[1,4]
- 利钠肽稳定作用:在人血浆中,沙库巴曲(10 μM)将心房利钠肽(ANP)的半衰期从2.1分钟延长至6.8分钟,证实其对NEP的抑制作用[4] 化合物 sacubitril (AHU-377) 是一种脑啡肽酶抑制剂,由缬沙坦(ARB)和 sacubitril (AHU-377) 分子部分以 1:1 的比例组成。 Sacubitril (AHU-377) 经过乙酯的酶裂解,生成活性脑啡肽酶抑制代谢物 LBQ657 [2]。无活性的 NEPi 前体 Sacubitril (AHU-377) 不会抑制成纤维细胞中的胶原蛋白形成或心肌细胞肥大。活性 NEPi LBQ657 似乎对心脏成纤维细胞没有任何影响。相反,LBQ657 会在一定程度上抑制心肌细胞肥大 [3]。 无活性的中性内肽酶抑制剂(NEPi)前体药物 AHU377 不抑制血管紧张素II(AngII)刺激的心脏成纤维细胞胶原积累,也不抑制心肌细胞肥大。 AHU377 的活性代谢物 LBQ657 能适度减弱AngII诱导的心肌细胞肥大,但对AngII诱导的心脏成纤维细胞胶原积累没有明显效果。 |
| 体内研究 (In Vivo) |
- 抗高血压作用:在高盐饮食诱导的Dahl-S高血压大鼠模型中,沙库巴曲(30–100 mg/kg口服)呈剂量依赖性降低收缩压22–35 mmHg。该效应可被NEP激活剂硫代芬(thiorphan)完全逆转[4]
- 心脏重塑预防:在心肌梗死后大鼠中,沙库巴曲(68 mg/kg/天口服)使左心室舒张末期内径减少7.6%,射血分数增加27.7%,显著改善心脏功能。这与心肌纤维化和肥厚减轻相关[3] - 尿钠排泄增强:在麻醉犬中,静脉注射沙库巴曲(1 mg/kg)使尿钠排泄量从17.3 ± 3.6 μequiv·kg⁻¹·min⁻¹增至199.5 ± 18.4 μequiv·kg⁻¹·min⁻¹,同时血浆环鸟苷酸(cGMP)水平升高3倍[4] ANF 使用媒介物治疗的狗的尿钠从 17.3±3.6 提高到 199.5±18.4 pequivkglmin。沙库巴曲 (AHU-377) 的作用在动物体内显着增强。静脉注射 Sacubitril (AHU-377) 的动物的尿量也同样增加 [1]。 Sacubitril(3、10 和 30 mg/kg,PO)预处理可使正常血压大鼠 ANP 诱导的血浆 cGMP 水平分别提高 2.4、3.3 和 4.0 倍(与媒介物相比,4 小时 AUC)[4]。在 Dahl-SS 大鼠中,sacubitril(30 和 100 mg/kg,PO)具有剂量依赖性抗高血压作用 [4]。 体内效应描述针对复方药物 LCZ696(包含缬沙坦和 AHU377)。在大鼠心肌梗死模型中,LCZ696治疗减轻了左心室重构和功能障碍,减少了心脏纤维化和肥大。 |
| 酶活实验 |
- NEP活性实验:将重组人NEP与沙库巴曲(0.1–100 nM)在含荧光底物Mca-RPPGFSAFK(Dnp)-OH的缓冲液中孵育30分钟(37°C)。通过检测λex/λem = 320/405 nm处的荧光强度变化,计算IC₅₀值[1,4]
|
| 细胞实验 |
体外培养的细胞性心脏肥大和纤维化[3]
大鼠新生心肌细胞和成纤维细胞通过酶促胶原酶消化法从1至2天大的Sprague-Dawley大鼠幼崽中获得,并按照我们实验室的常规方法制备用于体外测定。22通过掺入3[H]亮氨酸的AngII刺激(100 nmol/L)新生心肌细胞60小时来评估心肌细胞肥大。通过在新生儿心脏成纤维细胞中掺入3[H]脯氨酸48小时来测定AngII刺激的(100nmol/L)胶原合成。在刺激前,将细胞与缬沙坦、AHU377、LBQ657或缬沙坦+LBQ657(ARNi)预孵育1小时。使用的剂量范围和NEPi与ARB的比率旨在尽可能复制临床使用的LCZ696的剂量。这些药物是瑞士巴塞尔诺华公司的一份厚礼。此外,就在AngII刺激之前,将不同浓度的外源性B型钠尿肽(BNP)加入细胞培养基中,以评估NP信号直接增强的效果。实验重复2-4次,每次一式三份。 通过酶解胶原法从1-2日龄Sprague-Dawley乳鼠心脏获取新生大鼠心脏成纤维细胞和心肌细胞。 为评估对心脏纤维化的影响,通过[3H]脯氨酸掺入法测定AngII(100 nmol/L)刺激的新生心脏成纤维细胞48小时的胶原合成。 为评估对心脏肥大的影响,通过[3H]亮氨酸掺入法测定AngII(100 nmol/L)刺激的新生心肌细胞60小时的肥大情况。 细胞在刺激前与缬沙坦、AHU377、LBQ657或缬沙坦+LBQ657预孵育1小时。 |
| 动物实验 |
One week after MI, adult male Sprague-Dawley rats were randomized to treatment for 4 weeks with LCZ696 (68 mg/kg body weight perorally; MI-ARNi, n=11) or vehicle (MI-vehicle, n=6). Five weeks after MI, MI-ARNi versus MI-vehicle demonstrated lower LV end-diastolic diameter (by echocardiography; 9.7±0.2 versus 10.5±0.3 mm), higher LV ejection fraction (60±2 versus 47±5%), diastolic wall strain (0.23±0.02 versus 0.13±0.02), and circular strain (-9.8±0.5 versus -7.3±0.5%; all P<0.05). LV pressure-volume loops confirmed improved LV function. Despite similar infarct size, MI-ARNi versus MI-vehicle had lower cardiac weights (P<0.01) and markedly reduced fibrosis in peri-infarct and remote myocardium. Angiotensin II-stimulated incorporation of 3[H]leucine in cardiac myocytes and 3[H]proline in cardiac fibroblast was used to evaluate hypertrophy and fibrosis, respectively. The neprilysin inhibitor component of LCZ696, LBQ657, inhibited hypertrophy but not fibrosis. The angiotensin receptor blocker component of LCZ696, valsartan inhibited both hypertrophy and fibrosis. Dual valsartan+LBQ augmented the inhibitory effects of valsartan and the highest doses completely abrogated angiotensin II-mediated effects.[3]
We determined the relationship between atrial natriuretic peptide (ANP) and blood pressure in anesthetized, normotensive rats. We studied the relationship between NEP inhibition and elevation of plasma cGMP evoked by ANP in the absence and presence of AHU-377, an ester prodrug of LBQ657 and a component of LCZ696. Finally, using telemetry, we assessed the antihypertensive effects of AHU-377 in conscious Dahl-SS and DOCA-salt models of hypertension [4]. Hypertension Model: Male Dahl-S rats (8 weeks old) were fed a high-salt diet (8% NaCl) for 4 weeks to induce hypertension. Sacubitril (30 or 100 mg/kg) was administered orally once daily for 2 weeks. Systolic blood pressure was measured weekly via tail-cuff plethysmography [4] - Myocardial Infarction Model: Sprague-Dawley rats underwent left coronary artery ligation. Starting 24 hours post-MI, Sacubitril (68 mg/kg/day) or vehicle was administered orally for 4 weeks. Cardiac function was assessed by echocardiography, and fibrosis was quantified by picrosirius red staining [3] Adult male Sprague-Dawley rats (6- to 8-week-old, 220–250 g) were subjected to myocardial infarction (MI) by left anterior descending coronary artery ligation. One week after MI, rats were randomized to 4 weeks of treatment with LCZ696 (68 mg/kg body weight orally, which delivers both valsartan and the prodrug AHU377) or vehicle. Cardiac function was assessed by echocardiography and invasive left ventricular catheterization 5 weeks after MI, before euthanasia and organ harvest. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Peak plasma concentrations of sacubitril and it's metabolite, LBQ657 are reached in 0.5 hours and 2 hours respectively. Food does not clinically affect the systemic exposure of sacubitril or LBQ657. The oral bioavailability of sacubitril is >60%. It should be noted that the valsartan found in this combination is more bioavailable than other market available valsartan. 52% to 68% of sacubitril (primarily as the active metabolite LBQ657) is excreted in urine. 37% to 48% of sacubitril (primarily as LBQ657) is excreted in feces 103 L Metabolism / Metabolites Sacubitril is metabolized to LBQ657 by esterases. A low concentration (<10%) of a hydroxyl metabolite has been identified in plasma. Biological Half-Life The half life of sacubitril is 1.1 to 3.6 hours, and the half life of it's metabolite LBQ657 is 9.9 to 11.1 hours. - Oral Absorption: Sacubitril showed rapid oral absorption in rats, with Tmax of 1.5–2 hours. Absolute bioavailability was 23%, and the active metabolite LBQ657 reached Cmax within 3 hours [4] - Metabolism: Sacubitril was rapidly hydrolyzed by esterases to LBQ657, which accounted for >90% of NEP inhibitory activity in plasma. LBQ657 had a terminal half-life of 12 hours [4] - Excretion: Approximately 83% of the dose was excreted in bile, with 17% eliminated in urine. Less than 10% of the parent drug was detected in urine [4] After oral intake, LCZ696 is metabolized into the active angiotensin receptor blocker valsartan and the inactive neprilysin inhibitor precursor AHU377. AHU377 is then further cleaved into the active neprilysin inhibitor LBQ657. |
| 毒性/毒理 (Toxicokinetics/TK) |
Hepatotoxicity
The large prospective, placebo-controlled trials of sacubitril-valsartan in patients with heart failure usually did not mention or list ALT elevations or severe hepatic adverse events or deaths. In the FDA clinical review of data from these trials, elevations in ALT or AST were said to arise in 1.3% of patients on sacubitril-valsartan but a similar portion of those on enalapril [1.0%], and all elevations were judged to be unrelated to therapy and likely due to congestive liver disease due to heart failure. A single case of jaundice with aminotransferase elevations occurred, but in a patient who had stopped combination therapy because of worsening renal dysfunction and who was experiencing acute decompensated heart failure. Since approval and more widespread use of sacubitril-valsartan there have been at least two reports of acute liver injury attributed to its use. Both cases were relatively mild and resolved rapidly once the drug was stopped. Whether the injury was due to sacubitril or valsartan (or an interaction of both) was not clear. Valsartan, like other commonly used angiotensin receptor blockers, is known to be a rare cause of acute liver injury. The contribution of the underlying heart failure and possible congestive hepatopathy is also an issue. The reported cases did not have a liver biopsy and were not rechallenged with the drug which might have clarified the causality. Likelihood score: D (possible rare cause of clinically apparent liver injury, which may be due to valsartan rather than sacubitril). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Sacubitril is available in the United States only in combination with valsartan. Milk levels after the lowest dose of the combination are very low. If sacubitril milk levels of the highest dosage (4 times greater) are proportional to maternal dosage, they would still be quite low. Valsartan was undetectable at this dosage, so the combination product appears unlikely to affect the nursing infant. ◉ Effects in Breastfed Infants Two women taking sacubitril 24 mg and valsartan 26 mg (Entresto) did not observe any symptoms in their breastfed infants. Their extent of breastfeeding was not reported. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding Sacubitril and it's metabolite, LBQ657 are highly bound to plasma protein (94-97%). |
| 参考文献 |
|
| 其他信息 |
Pharmacodynamics
n a 7-day valsartan-controlled study in patients with reduced ejection fraction (HFrEF), administration of sacubitril + valsartan (Entresto) resulted in a significant non-sustained increase in natriuresis, increased urine cGMP, and decreased plasma MR-proANP and NT-proBNP compared to valsartan. In a 21-day study in HFrEF patients, it significantly increased urine ANP and cGMP and plasma cGMP, and decreased plasma NT-proBNP, aldosterone and endothelin-1. In clinical studies, this combination had no effect on QTc interval. - Mechanism of Action: Sacubitril acts as a prodrug that is converted to LBQ657, a selective NEP inhibitor. By blocking NEP, it prevents degradation of natriuretic peptides (ANP, BNP), leading to vasodilation, natriuresis, and inhibition of the renin-angiotensin-aldosterone system (RAAS) [1,4] - Therapeutic Use: Approved in combination with valsartan (LCZ696) for the treatment of heart failure with reduced ejection fraction (HFrEF), where it reduces cardiovascular mortality and hospitalization [3,4] - Clinical Pharmacology: In clinical trials, Sacubitril/valsartan (Entresto) significantly improved exercise capacity and quality of life in HFrEF patients, with a 20% lower risk of cardiovascular death compared to enalapril [4] AHU377 is the neprilysin inhibitor prodrug component of the first-in-class angiotensin receptor neprilysin inhibitor (ARNi) LCZ696 (later named sacubitril/valsartan). AHU377 itself is inactive and requires enzymatic cleavage to form the active neprilysin inhibitor LBQ657. The dual action of LCZ696 (combining RAAS blockade via valsartan and neprilysin inhibition via LBQ657) aims to augment beneficial natriuretic peptide effects while blocking harmful angiotensin II effects. Clinical trials (PARADIGM-HF, PARAMOUNT) evaluating LCZ696 showed promising efficacy in heart failure. |
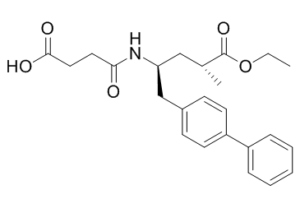
| 分子式 |
C24H29NO5
|
|---|---|
| 分子量 |
411.49076
|
| 精确质量 |
411.204
|
| CAS号 |
149709-62-6
|
| 相关CAS号 |
Sacubitril hemicalcium salt;1369773-39-6;Sacubitril-d4 hemicalcium salt;(2S,4S)-Sacubitril;149709-63-7;2R,4R-Sacubitril;766480-48-2;2R,4S-Sacubitril;761373-05-1;(Z)2S,4R-Sacubitril;Sacubitril sodium;149690-05-1;Sacubitril-d4;1884269-07-1;2S,4R-Sacubitril;2307668-79-5
|
| PubChem CID |
9811834
|
| 外观&性状 |
White to light yellow solid
|
| 密度 |
1.2±0.1 g/cm3
|
| 沸点 |
656.9±55.0 °C at 760 mmHg
|
| 闪点 |
351.1±31.5 °C
|
| 蒸汽压 |
0.0±2.1 mmHg at 25°C
|
| 折射率 |
1.549
|
| LogP |
3.96
|
| tPSA |
96.19
|
| 氢键供体(HBD)数目 |
2
|
| 氢键受体(HBA)数目 |
5
|
| 可旋转键数目(RBC) |
12
|
| 重原子数目 |
30
|
| 分子复杂度/Complexity |
550
|
| 定义原子立体中心数目 |
2
|
| SMILES |
O=C(CCC(O)=O)N[C@H](CC1=CC=C(C2=CC=CC=C2)C=C1)C[C@@H](C)C(OCC)=O
|
| InChi Key |
PYNXFZCZUAOOQC-UTKZUKDTSA-N
|
| InChi Code |
InChI=1S/C24H29NO5/c1-3-30-24(29)17(2)15-21(25-22(26)13-14-23(27)28)16-18-9-11-20(12-10-18)19-7-5-4-6-8-19/h4-12,17,21H,3,13-16H2,1-2H3,(H,25,26)(H,27,28)/t17-,21+/m1/s1
|
| 化学名 |
4-[[(2S,4R)-5-ethoxy-4-methyl-5-oxo-1-(4-phenylphenyl)pentan-2-yl]amino]-4-oxobutanoic acid
|
| 别名 |
LCZ696; AHU377; LCZ 696; AHU 377; LCZ696; AHU-377; Entresto
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : ~75 mg/mL (~182.26 mM)
H2O : ~0.67 mg/mL (~1.63 mM) |
|---|---|
| 溶解度 (体内实验) |
配方 1 中的溶解度: ≥ 2.5 mg/mL (6.08 mM) (饱和度未知) in 10% DMSO + 40% PEG300 + 5% Tween80 + 45% Saline (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。
例如,若需制备1 mL的工作液,可将100 μL 25.0 mg/mL澄清DMSO储备液加入到400 μL PEG300中,混匀;然后向上述溶液中加入50 μL Tween-80,混匀;加入450 μL生理盐水定容至1 mL。 *生理盐水的制备:将 0.9 g 氯化钠溶解在 100 mL ddH₂O中,得到澄清溶液。 配方 2 中的溶解度: ≥ 2.5 mg/mL (6.08 mM) (饱和度未知) in 10% DMSO + 90% (20% SBE-β-CD in Saline) (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 例如,若需制备1 mL的工作液,可将 100 μL 25.0 mg/mL澄清DMSO储备液加入900 μL 20% SBE-β-CD生理盐水溶液中,混匀。 *20% SBE-β-CD 生理盐水溶液的制备(4°C,1 周):将 2 g SBE-β-CD 溶解于 10 mL 生理盐水中,得到澄清溶液。 View More
配方 3 中的溶解度: ≥ 2.5 mg/mL (6.08 mM) (饱和度未知) in 10% DMSO + 90% Corn Oil (这些助溶剂从左到右依次添加,逐一添加), 澄清溶液。 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.4302 mL | 12.1510 mL | 24.3019 mL | |
| 5 mM | 0.4860 mL | 2.4302 mL | 4.8604 mL | |
| 10 mM | 0.2430 mL | 1.2151 mL | 2.4302 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。