| 靶点 |
URAT1/Urate transporter 1 (IC50 = 3.6 µM)
|
|---|---|
| 体外研究 (In Vitro) |
Dotinurad是一种新型的选择性尿酸盐重吸收抑制剂(SURI),在低剂量下对尿酸盐转运蛋白1 (URAT1,溶质载体家族22成员12 [SLC22A12])对尿酸盐的摄取有明显的抑制作用,URAT1定位于肾近端小管细胞的顶膜。[2]
Dotinurad抑制近端小管中的有机离子转运体,尤其是URAT1,但也可能与OATs相互作用。[1] |
| 体内研究 (In Vivo) |
本研究旨在阐明Dotinurad (FYU-981)的药代动力学(PK)谱。在大鼠、猴子和人类中,Dotinurad (FYU-981)的表观分布体积(分别为0.257、0.205和0.182 L/kg)和口服清除率(分别为0.054、0.037和0.013 L·h-1·kg-1)非常低,而血浆和腹腔浓度则维持在较高水平。此外,血浆蛋白结合率为99.4%,几乎没有物种差异。其主要代谢物为Dotinurad (FYU-981)葡萄糖醛酸(在人体内无特异性代谢物),未改变多丁醛酸的排泄百分比在所有被调查物种中都很低。Dotinurad (FYU-981)对细胞色素P450 (CYP)等代谢酶的抑制作用较弱,因此与该药相互作用的风险较低。综上所述,低剂量Dotinurad (FYU-981)具有良好的药理作用和理想的PK特性,其SURI为[2]。
在大鼠和猴子中,dotinurad和TRA给药后达到Cmax (Tmax)的时间相对较快(<1.83 h),而在人体内,由于14C-FYU-981是溶液给药,而dotinurad是片剂给药,因此,TRA的Tmax和Cmax分别比 dotinurad (FYU-981)更快和更高。大鼠、猴子和人对Dotinurad (FYU-981)的口服清除率(CL/F分别为0.054、0.037和0.013 L·h−1·kg−1)和表观Vd (Vd/F分别为0.257、0.205和0.182 L/kg)均极低。[2] |
| 酶活实验 |
14C-Dotinurad (FYU-981)血浆蛋白结合与血细胞分布比值[2]
在研究当天采集大鼠、猴和人的血浆和血液样本(n = 3)。将14C-Dotinurad (FYU-981)溶液(终浓度:1 μg/mL)分别加入血浆和血样中制备试验样品。为了测定血浆和血液中的放射性浓度,将每个测试样品的一份样品溶解在组织增溶剂SOLUENE-350中(只有血液测试样品用饱和过氧化苯甲酰的苯进行脱色),并与闪烁体HIONIC-FLUOR混合。剩余样品在37°C水浴中孵育5 min。等额血浆样品注入超离心装置,离心(1800×g, 37°C, 10 min)回收滤液。滤液用闪烁器混合。用液体闪烁计数器测量了处理后的等离子体试样和滤液的放射性。根据血浆和滤液中的放射性浓度计算血浆蛋白结合率。相反,血液测试样本是在毛细管中收集,以确定红细胞压积值(Ht)。剩余血样离心(8000×g, 4°C, 5 min)分离血浆。血浆的等分物溶解在组织增溶剂中,并用闪烁体混合。用LSC法测定了处理后的血液样品和分离后的血浆的放射性。根据全血和血浆中的Ht和放射性浓度计算出血细胞的放射性分布。 CYP抑制研究[2] 根据人与动物桥接研究组织(Human and Animal Bridging Research Organization, HAB)的方案,对多替努德的CYP抑制作用进行了评价。本研究评估的Dotinurad (FYU-981)抑制浓度分别为1、2.5、5、10、25、50和100 μM。修改了HAB方案中CYPs代谢物的分析方法和抑菌效果的计算方法。CYP1A2、CYP2B6、CYP2C19、CYP2D6、CYP2E1、CYP3A4的色谱柱为CAPCELL PAK C18 UG 120 (4.6 × 250 mm, 5 μm), CYP2C9的色谱柱为Mightysil RP-18GP (4.6 × 250 mm, 5 μm)。每个IC50由活性比(%)计算,即存在Dotinurad (FYU-981)时的活性除以不存在dotinurad时的活性。 |
| 细胞实验 |
14C-Dotinurad (FYU-981)在低温保存肝细胞中的体外代谢比较研究[2]
来自Sekisui XenoTech的雄性大鼠和猴子冷冻保存肝细胞和混合性别人冷冻保存肝细胞。采用Sekisui XenoTech公司生产的肝细胞分离试剂盒(K2000)制备肝细胞悬液。每个物种的肝细胞悬液(终浓度:1 × 106个细胞/mL)或Krebs-Henseleit Buffer (118 mM NaCl, 4.7 mM KCl, 2.5 mM CaCl2, 1.2 mM KH2PO4, 1.2 mM MgSO4, 25 mM NaHCO3, 6.3 mM HEPES和11 mM d-glucose, pH 7.4);对照组)加入24孔板,在CO2培养箱(37℃,5% CO2, 95%空气)中预孵育10 min。反应开始时,加入14C-Dotinurad (FYU-981)溶液(终浓度:10 μM),在CO2培养箱中孵育0和1 h。孵育后,在孵育混合物中加入与混合物体积相同的乙腈终止反应。终止后,搅拌并离心(1800×g, 4°C, 5 min)分离上清。收集的上清液用蒸发器蒸发至干燥。干燥后,将残渣超声溶解于n -甲基-2-吡咯烷二酮/初始流动相(1:1,v/v)中。将溶液离心(15000×g, 4°C, 5 min),得到的上清液注射到HPLC-放射性检测(RAD)中,装置由岛津10A高效液相色谱系统和625 TR流动闪烁分析仪组成。HPLC分析条件称为“样品分析”。 |
| 动物实验 |
The animal studies were conducted at SMD (all radioisotope and monkey studies) or FY (rat study). Male Sprague-Dawley (SD, Crj:CD[SD]IGS) rats, aged 6 weeks were purchased from Charles River Laboratories. After a 1-week acclimatization period, the animals were used for the study at 7 weeks old. Male cynomolgus monkeys, aged 3 years, were purchased from Hamri Co., Ltd. Dotinurad (FYU-981) (including 14C-FYU-981) was suspended in 0.5% methylcellulose and administered orally (p.o.) at a dose of 1 mg/kg to starved rats or monkeys.[2]
Dotinurad (FYU-981) concentration in rat, monkey, and human plasma were analyzed using a validated method at FY. The rat and monkey plasma samples were deproteinized, using methanol containing an internal standard (F12994), and analyzed using liquid chromatography-tandem mass spectrometry and ultraperformance-LC, respectively. The standard curve of dotinurad ranged between 1 and 300 ng/mL for rat plasma and 30–3000 ng/mL for monkey plasma. The human plasma samples were processed using solid-phase extraction in a 96-well plate format and analyzed using LC-MS/MS. The standard curve of dotinurad ranged between 1 and 1000 ng/mL for human plasma. Dotinurad and matrix constituents in human plasma were separated using an Inertsil ODS-3 (2.1 × 150 mm 3 μm) at 50 °C with a mobile phase of 5 mmol/L ammonium acetate (pH 4) in water and methanol (50:50, v/v). The total flow rate was set at 0.18 mL/min. Ionization was conducted in the turbo ion spray and negative ion modes. Dotinurad was analyzed as [M-H]- ions in the multiple reaction monitoring mode (transitions: dotinurad 356.0/159.9 and internal standard F12994 341.1/145.1).[2] |
| 药代性质 (ADME/PK) |
Plasma protein binding ratio and blood cell distribution[2]
Table 1 shows that the plasma protein binding percentage and blood cell distribution of dotinurad were similar in all the investigated species. There was no species difference in these parameters. Metabolism[2] The results of the in vitro comparative metabolism study of 14C-FYU-981 in cryopreserved hepatocytes are presented in Table 3. The production ratios of glucuronide (7.3, 3.8, and 3.5%) and sulfate (3.8, 3.6 and 1.8%) metabolites of 14C-FYU-981 were high in rat, monkey, and human hepatocytes. The level of 14C-FYU-981 in human hepatocytes was slightly higher than that in rat hepatocytes, suggesting that the CL of 14C-FYU-981 was lower in human than it was in rat hepatocytes. The percentage of detected metabolites in samples collected after administration of 14C-FYU-981 to rats, monkeys, and humans are presented in Table 4. In rat, monkey, and human plasma, the parent compound was detected as a major component, accounting for 81.9, 92.0, and 80.9% radioactivity, respectively. Levels of the methyl DCHB, sulfate, and 6-hydroxy metabolites were comparably high in the plasma samples of all tested species. In rat and human samples, levels of the methyl DCHB metabolite were the highest (2.8 and 5.1%, respectively), whereas the sulfate metabolite level was highest (1.5%) in monkeys. In rat urine, the percentage of 14C-FYU-981 was 2.2% and the sulfate of DCHB was detected as a major metabolite, accounting for 21.9%, followed by DCHB (12.2%) and a sulfate (11.7%). In monkey and human urine, 14C-FYU-981 was detected at 5.0 and 1.3%, respectively and the glucuronide was a major metabolite (37.0 and 51.8%, respectively), followed by the sulfate (26.7 and 23.4%, respectively). In feces, the levels of the 6-hydroxy, DCHB, and sulfonate metabolites and the parent compound were higher than those of other metabolites. The recovery of radioactivity from rat, monkey, and human fecal samples were 79.9, 78.8, and 67.5%, respectively. These values were slightly low. However, the radioactivity that could not be recovered was less than 4.6% as a percent of dose. The metabolite profile of the monkey was more similar to the human profile than it was to the rat profile. Excretion[2] Fig. 3 shows the mean cumulative excretion of radioactivity into the urine, feces, and expired air and the total recovery. The urinary radioactivity levels were 68.7, 83.7, and 86.4% of the dose in rats, monkeys, and humans, respectively, whereas the corresponding levels in the feces were 22.7, 6.7, and 7.9% of the dose, respectively, for up to 168 h in both samples. In the rat, monkey, and human samples, the excreted percentage radioactivity in expired air was 4.2, 7.8, and 5.0% of the dose for up to 96 h and the total recovered radioactivity was satisfactory at 95.5, 98.2, and 99.4%, respectively. The major route of excretion was the urine, and after accounting for the metabolite profile, the radioactivity was mainly excreted as the sulfate of DCHB in rats and as the glucuronide in monkeys and humans. CYP inhibition study[2] Table 5 shows the result of evaluation of the inhibitory effect of dotinurad on major CYP isoforms (CYP1A2, 2A6, 2B6, 2C9, 2C19, 2D6, 2E1, and 3A4) in human liver microsomes. Dotinurad inhibited CYP2C9 with an inhibitory constant (Ki) value of 10.4 μmol/L. According to DDI guidelines [13], the R value calculated from the Ki and unbound Cmax after 7-day repeated administration of 4 mg dotinurad (7.0 nmol/L: unpublished data) was 1.00. Therefore, it was predicted that the risk of DDI via CYP inhibition was low. |
| 参考文献 | |
| 其他信息 |
Dotinurad is under investigation in clinical trial NCT03372200 (Febuxostat-controlled, Double-blind, Comparative Study of FYU-981 in Hyperuricemia With or Without Gout).
The factors that maintain a high plasma drug concentration include high bioavailability (BA), low Vd, and low CL/F. The BA of dotinurad in rats and monkeys were 86.9 and 91.0%, respectively, and CL/F in human (0.013 L·h-1·kg-1) was lower than in rats (0.052 L·h-1·kg-1) and in monkeys (0.037 L·h-1·kg-1). Furthermore, a human mass balance study showed that at least 91.4% of dotinurad was absorbed after oral administration, which was calculated using excreted percentage radioactivity of urine and expired air. Although the BA of dotinurad in humans has not been evaluated, it is expected to be high. Vd/F values of dotinurad in rats and monkeys were nearly equal to the extracellular fluid volume (0.297 and 0.208 L/kg, respectively). Furthermore, the Vd/F of dotinurad in humans was almost the same as that in rats and monkeys (Table 1). This result could be attributable to certain factors such as the similar Vd of rats and monkeys, which was almost constant following administration of doses of 0.3–3 mg/kg in rats (data not shown). In addition, the plasma protein binding was almost the same in rats, monkeys, and humans. The CL of dotinurad seems to be mainly mediated by metabolism, because the excretion pathways of dotinurad is mainly through the urine as metabolites (Fig. 3 and Table 4). In rats and monkeys the CL/F values were considerably lower than the hepatic blood flow values, which were 3.3 and 2.6 L·h-1·kg-1, respectively, indicating that the CL of dotinurad was low. These results indicated that high BA, low Vd/F, and CL/F leads to high plasma concentration of dotinurad at a low administration dose.[2] Luminal drug concentrations in the renal proximal tubules could be regarded as the unbound plasma concentrations. Although lower plasma protein binding ratio would lead to higher concentrations in the renal lumen, this would also persistently affect the pharmacological by increasing the renal CL. The plasma protein binding of dotinurad was 99.4% in humans. This value might seem high as the pharmacological target of the drug is the renal tubules. However, this value suggests an adequate balance between the pharmacological effects and PK with a long duration. In fact, effects on serum urate levels and renal urate excretion of dotinurad were apparently saturable at a dose >5 mg, and PK/PD modeling and simulation of dotinurad (simple maximal effect model) indicated that the plasma concentration at the half-maximal effect of dotinurad was 3.8 nM (196 ng/mL corresponding to Cmax at a dose of 2 mg). Clinical dosage of benzbromarone is 50 mg (12.5-fold of dotinurad), even though IC50 value of benzbromarone (0.190 μM) in urate transport via URAT1 is approximately 5-fold that of dotinurad (0.0372 μM). The CL/F and Vd/F of benzbromarone in humans were approximately 0.053 L·h-1·kg-1, and 0.4 L/kg, respectively (calculated from dosage, AUC0-24 and T1/2). Although BA of dotinurad and benzbromarone remains unclear, if BA of dotinurad and benzbromarone were similar, the CL and Vd of dotinurad would be predicted to be lower than benzbromarone. Therefore, these results suggested that dotinurad has an ideal PK profile for a UA rather than benzbromarone for efficient drug delivery to its target.[2] In addition, dotinurad potently inhibits URAT1 and exhibits high selectivity for other urate secretory transporters such as ABCG2, organic anion transporter 1 (OAT1, SLC22A6), and OAT3 (SLC22A8); consequently, it is designated a SURI. The pharmacological and PK characteristic of this agent both contribute to be its continuous serum uric acid-lowering activity at low doses (0.5–4 mg). In addition, at pharmacologically active concentrations, dotinurad did not inhibit drug transporters, such as multiple drug resistance 1 (MDR1), OATPs, and MATEs (recommended in DDI guidelines), and drug metabolizing enzymes such as CYPs (e.g., CYP2C9, which is inhibited by benzbromarone) and UGTs (data not shown). Furthermore, the contribution of MDR1 and ABCG2 for absorption of dotinurad from the intestine was low, as dotinurad has high absorption. In a rat in vivo study, dotinurad liver concentration was approximately 2-fold of plasma concentration (data not shown), and Vd/F in human was low. Therefore, this suggested that the contribution of OATP1B1 and OATP1B3 for uptake of dotinurad to the liver was low. If dotinurad was a substrate of these drug transporters, the affinity of dotinurad to these drug transporters would be low when considering IC50 of dotinurad on uptake of typical substrates by these drug transporters (MDR1 > 200 μM, ABCG2 74.7 μM, OATP1B1 11.5 μM, OATP1B3 > 200 μM). Therefore, the risk of DDIs with dotinurad is expected to be low as it exhibits pharmacological effects at low doses.[2] Chronic kidney disease (CKD) has become a global public health issue and uric acid (UA) remains a major risk factor of CKD. As the main organ for the elimination of UA, kidney owned a group of urate transporters in tubular epithelium. Kidney disease hampered the UA excretion, and the accumulation of serum UA in return harmed the renal function. Commercially, there are three kinds of agents targeting at urate-lowering, xanthine oxidoreductase inhibitor which prevents the production of UA, uricosuric which increases the concentration of UA in urine thus decreasing serum UA level, and uricase which converts UA to allantoin resulting in the dramatic decrement of serum UA. Of note, in patients with CKD, administration of above-mentioned agents, alone or combined, needs special attention. New evidence is emerging for the efficacy of several urate-lowering drugs for the treatment of hyperuricemia in patients with CKD. Besides, loads of novel and promising drug candidates and phytochemicals are in the different phases of research and development. As of today, there is insufficient evidence to recommend the widespread use of UA-lowering therapy to prevent or slow down the progression of CKD. The review summarized the evidence and perspectives about the treatment of hyperuricemia with CKD for medicinal chemist and nephrologist.[1] |
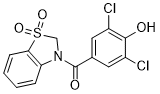
| 分子式 |
C14H9CL2NO4S
|
|---|---|
| 分子量 |
358.1966
|
| 精确质量 |
356.962
|
| 元素分析 |
C, 46.95; H, 2.53; Cl, 19.79; N, 3.91; O, 17.87; S, 8.95
|
| CAS号 |
1285572-51-1
|
| 相关CAS号 |
1285572-51-1;
|
| PubChem CID |
51349053
|
| 外观&性状 |
Typically exists as solid at room temperature
|
| LogP |
2.9
|
| tPSA |
83.1
|
| 氢键供体(HBD)数目 |
1
|
| 氢键受体(HBA)数目 |
4
|
| 可旋转键数目(RBC) |
1
|
| 重原子数目 |
22
|
| 分子复杂度/Complexity |
538
|
| 定义原子立体中心数目 |
0
|
| InChi Key |
VOFLAIHEELWYGO-UHFFFAOYSA-N InChi Code
|
| InChi Code |
InChI=1S/C14H9Cl2NO4S/c15-9-5-8(6-10(16)13(9)18)14(19)17-7-22(20,21)12-4-2-1-3-11(12)17/h1-6,18H,7H2
|
| 化学名 |
(3,5-dichloro-4-hydroxyphenyl)(1,1-dioxidobenzo[d]thiazol-3(2H)-yl)methanone
|
| 别名 |
FYU-981; FYU 981; Dotinurad; 1285572-51-1; (3,5-dichloro-4-hydroxyphenyl)(1,1-dioxidobenzo[d]thiazol-3(2H)-yl)methanone; (3,5-dichloro-4-hydroxyphenyl)-(1,1-dioxo-2H-1,3-benzothiazol-3-yl)methanone; 305EB53128; Urece; FYU981; Urece
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.7917 mL | 13.9587 mL | 27.9174 mL | |
| 5 mM | 0.5583 mL | 2.7917 mL | 5.5835 mL | |
| 10 mM | 0.2792 mL | 1.3959 mL | 2.7917 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。