| 规格 | 价格 | |
|---|---|---|
| 500mg | ||
| 1g | ||
| Other Sizes |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
IDENTIFICATION AND USE: Batrachotoxins are neurotoxic steroidal alkaloids first isolated from a Colombian poison-dart frog and later found in certain passerine birds of New Guinea. Neither vertebrate group is thought to produce the toxins de novo, but instead they likely sequester them from dietary sources. HUMAN STUDIES: Batrachotoxin is a potent modulator of voltage-gated sodium channels, leading to irreversible depolarization of nerves and muscles, fibrillation, arrhythmias and eventually cardiac failure. Since its discovery, field researchers also reported numbness after their skin came into contact with this toxin. ANIMAL STUDIES: Levels of batrachotoxin tend to be reduced when P. terribilis is maintained in captivity, but even after being confined for up to 6 years, these frogs were still at least five times more toxic than other Phyllobates species used by natives for poisoning blowgun darts. Batrachotoxin was not detectable in F1 progeny reared to maturity in captivity. Nerve and muscle preparations from wild-caught frogs and from the nontoxic F1 frogs were both insensitive to batrachotoxin. The regulatory site controlling sodium-channel activation and permeability appears to have been minimally altered to prevent interaction with batrachotoxin, but is still sensitive to other sodium conductance activators (veratridine, grayanotoxin) to which the frogs are not exposed naturally. Interactions Two distinct types of local anesthetics (LAs) have previously been found to block batrachotoxin (BTX)-modified Na+ channels: type 1 LAs such as cocaine and bupivacaine interact preferentially with open channels, whereas type 2 LAs, such as benzocaine and tricaine, with inactivated channels. Herein, we describe our studies of a third type of LA, represented by tetracaine as a dual blocker that binds strongly with closed channels but also binds to a lesser extent with open channels when the membrane is depolarized. Enhanced inactivation of BTX-modified Na+ channels by tetracaine was determined by steady-state inactivation measurement and by the dose-response curve. The 50% inhibitory concentration (IC50) was estimated to be 5.2 microM at -70 mV, where steady-state inactivation was maximal, with a Hill coefficient of 0.98 suggesting that one tetracaine molecule binds with one inactivated channel. Tetracaine also interacted efficiently with Na+ channels when the membrane was depolarized; the IC50 was estimated to be 39.5 microM at +50 mV with a Hill coefficient of 0.94. Unexpectedly, charged tetracaine was found to be the primary active form in the blocking of inactivated channels. In addition, external Na+ ions appeared to antagonize the tetracaine block of inactivated channels. Consistent with these results, N-butyl tetracaine quaternary ammonium, a permanently charged tetracaine derivative, remained a strong inactivation enhancer. Another derivative of tetracaine, 2-(di-methylamino) ethyl benzoate, which lacked a 4-butylamino functional group on the phenyl ring, elicited block that was approximately 100-fold weaker than that of tetracaine. We surmise that 1) the binding site for inactivation enhancers is within the Na+ permeation pathway, 2) external Na+ ions antagonize the block of inactivation enhancers by electrostatic repulsion, 3) the 4-butylamino functional group on the phenyl ring is critical for block and for the enhancement of inactivation, and 4) there are probably overlapping binding sites for both inactivation enhancers and open-channel blockers within the Na+ pore PURPOSE: To investigate the response to general anesthetics of different sodium-channel subtypes, we examined the effects of pentobarbital, a close thiopental analogue, on single sodium channels from human skeletal muscle and compared them to existing data from human brain and human ventricular muscle channels. METHODS: Sodium channels from a preparation of human skeletal muscle were incorporated into planar lipid bilayers, and the steady-state behavior of single sodium channels and their response to pentobarbital was examined in the presence of batrachotoxin, a sodium-channel activator. Single-channel currents were recorded before and after the addition of pentobarbital (0.34-1.34 mM). RESULTS: In symmetrical 500 mM NaCl, human skeletal muscle sodium channels had an averaged single-channel conductance of 21.0 +/- 0.6 pS, and the channel fractional open time was 0.96 +/- 0.04. The activation midpoint potential was -96.2 +/- 1.6 mV. Extracellular tetrodotoxin blocked the channel with a half-maximal concentration (k1/2) of 60 nM at 0 mV. Pentobarbital reduced the time-averaged conductance of single skeletal muscle sodium channels in a concentration-dependent manner (inhibitory concentration 50% [IC50] = 0.66 mM). The steady-state activation was shifted to more hyperpolarized potentials (-16.7 mV at 0.67 mM pentobarbital). CONCLUSION: In the planar lipid bilayer system, skeletal muscle sodium channels have some electrophysiological properties that are significantly different compared with those of sodium channels from cardiac or from central nervous tissue. In contrast to the control data, these different human sodium channel subtypes showed the same qualitative and quantitative response to the general anesthetic pentobarbital. The implication of these effects for overall anesthesia will depend on the role the individual channels play within their neuronal networks, but suppression of both central nervous system and peripheral sodium channels may add to general anesthetic effects We have investigated the action of procainamide on batrachotoxin (BTX)-activated sodium channels from bovine heart and rat skeletal muscle. When applied to the intracellular side, procainamide induced rapid, open-channel block. We estimated rate constants using amplitude distribution analysis. Membrane depolarization increased the blocking rate and slowed unblock. The rate constants were similar in both magnitude and voltage dependence for cardiac and skeletal muscle channels. Qualitatively, this block resembled the fast open-channel block by lidocaine, but procainamide was about sevenfold less potent. Molecular modeling suggests that the difference in potency between procainamide and lidocaine might arise from the relative orientation of their aromatic rings, or from differences in the structure of the aryl-amine link. For the cardiac channels, procainamide reduced the frequency of transitions to a long-lived closed state which shows features characteristic of inactivation. Mean durations of kinetically identified closed states were not affected. The degree of fast block and of inhibition of the slow closures were correlated. Internally applied QX-314, a lidocaine derivative and also a fast blocker, produced a similar effect. Thus, drug binding to the fast blocking site appears to inhibit inactivation in BTX-activated cardiac channels. The purpose of the present study was to examine the characteristics of Na+ channel modification by batrachotoxin (BTX) in cardiac cells, including changes in channel gating and kinetics as well as susceptibility to block by local anesthetic agents. We used the whole cell configuration of the patch clamp technique to measure Na+ current in guinea pig myocytes. Extracellular Na+ concentration and temperature were lowered (5-10 mM, 17 degrees C) in order to maintain good voltage control. Our results demonstrated that 1) BTX modifies cardiac INa, causing a substantial steady-state (noninactivating) component of INa, 2) modification of cardiac Na+ channels by BTX shifts activation to more negative potentials and reduces both maximal gNa and selectivity for Na+; 3) binding of BTX to its receptor in the cardiac Na+ channel reduces the affinity of local anesthetics for their binding site; and 4) BTX-modified channels show use-dependent block by local anesthetics. The reduced blocking potency of local anesthetics for BTX-modified Na+ channels probably results from an allosteric interaction between BTX and local anesthetics for their respective binding sites in the Na+ channel. Our observations that use-dependent block by local anesthetics persists in BTX-modified Na+ channels suggest that this form of extra block can occur in the virtual absence of the inactivated state. Thus, the development of use-dependent block appears to rely primarily on local anesthetic binding to activated Na+ channels under these conditions. For more Interactions (Complete) data for Batrachotoxin (6 total), please visit the HSDB record page. Non-Human Toxicity Values LD50 Mice iv 0.002 mg/kg LD50 Mice dermal 2 ug/kg |
|---|---|
| 参考文献 | |
| 其他信息 |
Batrachotoxin has been reported in Phyllobates aurotaenia with data available.
Batrachotoxin is batrachotoxins are potent activators of sodium channels identified in extract of frog skins. Mechanism of Action Batrachotoxin is a potent modulator of voltage-gated sodium channels, leading to irreversible depolarization of nerves and muscles, fibrillation, arrhythmias and eventually cardiac failure. Since its discovery, field researchers also reported numbness after their skin came into contact with this toxin. Intrigued by this phenomenon, we determined the effect of batrachotoxin on the voltage-gated sodium channel Nav1.8, which is considered to be a key player in nociception. As a result, we discovered that batrachotoxin profoundly modulates this channel: the inactivation process is severely altered, the voltage-dependence of activation is shifted towards more hyperpolarized potentials resulting in the opening of Nav1.8 at more negative membrane potentials and the ion selectivity is modified. Batrachotoxin (BTX), from South American frogs of the genus Phyllobates, irreversibly activates voltage-gated sodium channels. Previous work demonstrated that a phenylalanine residue approximately halfway through pore-lining transmembrane segment IVS6 is a critical determinant of channel sensitivity to BTX. In this study, we introduced a series of mutations at this site in the Na(v)1.3 sodium channel, expressed wild-type and mutant channels in Xenopus laevis oocytes, and examined their sensitivity to BTX using voltage clamp recording. We found that substitution of either alanine or isoleucine strongly reduced channel sensitivity to toxin, whereas cysteine, tyrosine, or tryptophan decreased toxin action only modestly. These data suggest an electrostatic ligand-receptor interaction at this site, possibly involving a charged tertiary amine on BTX. We then used a mutant channel (mutant F1710C) with intermediate toxin sensitivity to examine the properties of the toxin-receptor reaction in more detail. In contrast to wild-type channels, which bind BTX almost irreversibly, toxin dissociation from mutant channels was rapid, but only when the channels were open, not when they were closed. These data suggest the closed activation gate trapped bound toxin. Although BTX dissociation required channel activation, it was, paradoxically, slowed by strong membrane depolarization, suggesting additional state-dependent and/or electrostatic influences on the toxin binding reaction. We propose that BTX moves to and from its receptor through the cytoplasmic end of the open ion-conducting pore, in a manner similar to that of quaternary local anesthetics like QX314. The binding site for batrachotoxin, a lipid-soluble neurotoxin acting at Na+ channel receptor site 2, was localized using a photoreactive radiolabeled batrachotoxin derivative to covalently label purified and reconstituted rat brain Na+ channels. In the presence of the brevetoxin 1 from Ptychodiscus brevis and the pyrethroid RU51049, positive allosteric enhancers of batrachotoxin binding, a protein with an apparent molecular mass of 240 kDa corresponding to the Na+ channel alpha subunit was specifically covalently labeled. The region of the alpha subunit specifically photolabeled by the photoreactive batrachotoxin derivative was identified by antibody mapping of proteolytic fragments. Even after extensive trypsinization, and anti-peptide antibody recognizing an amino acid sequence adjacent to Na+ channel transmembrane segment IS6 was able to immunoprecipitate up to 70% of the labeled peptides. Analysis of a more complete digestion with trypsin or V8 protease indicated that the batrachotoxin receptor site is formed in part by a portion of domain I. The identification of a specifically immunoprecipitated photolabeled 7.3-kDa peptide containing transmembrane segment S6 from domain I restricted the site of labeling to residues Asn-388 to Glu-429 if V8 protease digestion was complete or Leu-380 to Glu-429 if digestion was incomplete. These results implicate the S6 transmembrane region of domain I of the Na+ channel alpha subunit as an important component of the batrachotoxin receptor site. The steroidal neurotoxin (-)-batrachotoxin functions as a potent agonist of voltage-gated sodium ion channels (NaVs). Here we report concise asymmetric syntheses of the natural (-) and non-natural (+) antipodes of batrachotoxin, as well both enantiomers of a C-20 benzoate-modified derivative. Electrophysiological characterization of these molecules against NaV subtypes establishes the non-natural toxin enantiomer as a reversible antagonist of channel function, markedly different in activity from (-)-batrachotoxin. Protein mutagenesis experiments implicate a shared binding side for the enantiomers in the inner pore cavity of NaV. These findings motivate and enable subsequent studies aimed at revealing how small molecules that target the channel inner pore modulate NaV dynamics. Batrachotoxins (BTX): Neurotoxin, activates sodium ion channels, digitalis (digitoxin)-like cardiotoxin, causes fibrillation and cardiac arrest. /from table/ |
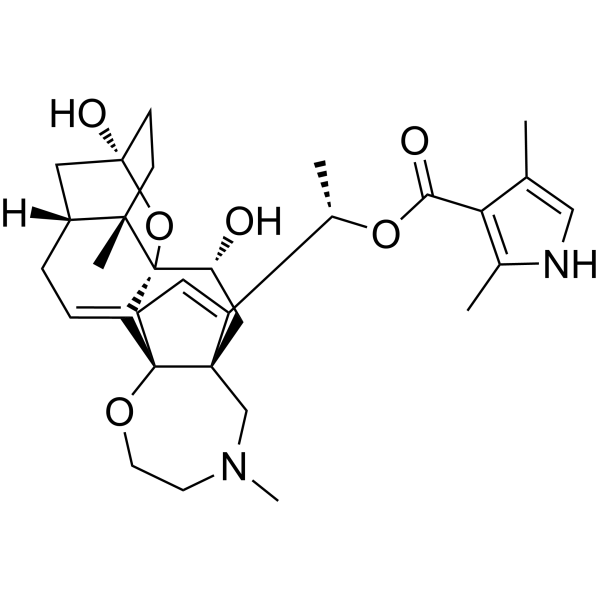
| 分子式 |
C31H42N2O6
|
|---|---|
| 分子量 |
538.67
|
| 精确质量 |
538.304
|
| CAS号 |
23509-16-2
|
| PubChem CID |
6324647
|
| 外观&性状 |
Noncrystal
|
| 密度 |
1.34g/cm3
|
| 沸点 |
744ºC at 760mmHg
|
| 闪点 |
403.8ºC
|
| 蒸汽压 |
3E-23mmHg at 25°C
|
| 折射率 |
1.642
|
| LogP |
3.49
|
| tPSA |
104.25
|
| 氢键供体(HBD)数目 |
3
|
| 氢键受体(HBA)数目 |
7
|
| 可旋转键数目(RBC) |
4
|
| 重原子数目 |
39
|
| 分子复杂度/Complexity |
1140
|
| 定义原子立体中心数目 |
8
|
| SMILES |
CC1=CNC(=C1C(=O)O[C@@H](C)C2=CC[C@@]34[C@@]2(C[C@H]([C@@]56C3=CC[C@H]7[C@@]5(CC[C@](C7)(O6)O)C)O)CN(CCO4)C)C
|
| InChi Key |
ISNYUQWBWALXEY-OMIQOYQYSA-N
|
| InChi Code |
InChI=1S/C31H42N2O6/c1-18-16-32-19(2)25(18)26(35)38-20(3)22-8-9-30-23-7-6-21-14-29(36)11-10-27(21,4)31(23,39-29)24(34)15-28(22,30)17-33(5)12-13-37-30/h7-8,16,20-21,24,32,34,36H,6,9-15,17H2,1-5H3/t20-,21+,24+,27-,28-,29+,30-,31-/m0/s1
|
| 化学名 |
[(1S)-1-[(1R,5R,6S,9R,11S,12R,14R)-9,12-dihydroxy-6,16-dimethyl-10,19-dioxa-16-azahexacyclo[12.5.3.15,9.01,14.02,11.06,11]tricosa-2,21-dien-22-yl]ethyl] 2,4-dimethyl-1H-pyrrole-3-carboxylate
|
| 别名 |
BTX
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.8564 mL | 9.2821 mL | 18.5642 mL | |
| 5 mM | 0.3713 mL | 1.8564 mL | 3.7128 mL | |
| 10 mM | 0.1856 mL | 0.9282 mL | 1.8564 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。