| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| Other Sizes |
|

| 靶点 |
anti-HBV, HepG2 cell(EC50=3.75 nM)
The target of Entecavir (SQ 34676) is the DNA polymerase (HBV Pol) of hepatitis B virus (HBV), including wild-type HBV Pol and lamivudine (3TC)-resistant HBV Pol mutants (YMDD mutants: M550V/L526M, M550I). Entecavir triphosphate (ETV-TP) is 100- to 300-fold more potent than 3TC-TP against 3TC-resistant HBV Pol, and 20- to 30-fold higher concentrations of Entecavir are required to inhibit the replication of 3TC-resistant HBV in cell culture [1] |
|---|---|
| 体外研究 (In Vitro) |
体外活性:恩替卡韦三磷酸盐是野生型 HBV Pol 的高效抑制剂,对 3TC 耐药的 HBV Pol 的抑制作用比拉米夫定三磷酸盐强 100 至 300 倍。恩替卡韦可抑制 3TC 耐药 HBV 的复制,但需要高 20 至 30 倍的浓度。恩替卡韦可显着减少血清病毒 DNA 与肝活检标本中的共价闭合环状 DNA 和乙型肝炎病毒核心抗原阴性。在独特的单周期、基于单细胞的假病毒测定中,恩替卡韦具有有效的抗 HIV 活性(EC50,0.1 nM)(24),使用绿色荧光蛋白报告基因荧光激活细胞分选仪测定作为终点,以 CD4+ 淋巴细胞为终点。激酶测定:BMS-200475 针对 HBV 的 EC50 为 3.75 nM。它被掺入 HBV 的蛋白质引物中,随后抑制逆转录酶的引发步骤。 BMS-200475 对其他 RNA 和 DNA 病毒的抗病毒活性明显较低。恩替卡韦比其他脱氧鸟苷类似物(喷昔洛韦、更昔洛韦、洛布卡韦和阿昔洛韦)或拉米夫定更容易磷酸化为其活性代谢物。恩替卡韦的细胞内半衰期为15小时。细胞测定:BMS 200475 在磷酸盐缓冲盐水 (PBS) 中制备,并用含有 2% 胎牛血清的适当培养基稀释。 HepG2 2.2.15 细胞以每孔 5×105 个细胞的密度接种在 12 孔 Biocoat 胶原蛋白包被的板上,并保持汇合状态 2 至 3 天,然后用 1 mL 掺有 BMS 200475 的培养基覆盖. 第 10 天进行 HBV 定量。
1. 酶活性层面:恩替卡韦三磷酸盐(ETV-TP)是野生型HBV Pol的高效抑制剂,对拉米夫定耐药的HBV Pol(YMDD突变体:M550V/L526M、M550I)的抑制活性比3TC-TP高100-300倍 [1] 2. 细胞活性层面:恩替卡韦可在HepG2细胞中抑制拉米夫定耐药HBV的复制,但所需浓度比抑制野生型HBV高20-30倍 [1] 3. 细胞内磷酸化:在肝癌细胞中,使用与患者血浆药物水平相当的外源性恩替卡韦处理后,细胞内的ETV-TP可积累至足以抑制野生型和拉米夫定耐药HBV Pol酶活性的水平 [1] |
| 体内研究 (In Vivo) |
恩替卡韦可使鸭血清 DHBV DNA 水平在 80 天内下降 4 个对数级,并在 120 天内使血清 DHBV 表面抗原 (DHBsAg) 水平缓慢下降 2 至 3 个对数级。恩替卡韦治疗使肝脏中的 DHBV DNA 复制中间体减少了 70 倍,而鸭子中稳定的模板形式共价闭合环状 DNA 的水平仅减少了 4 倍。恩替卡韦治疗降低了鸭肝脏中抗原染色的强度和抗原阳性肝细胞的百分比,但胆管细胞中抗原染色的强度似乎不受影响。每日口服 BMS-200475,剂量范围为 0.02 至 0.5 mg/kg 体重,持续 1 至 3 个月,可有效降低慢性感染土拨鼠的土拨鼠肝炎病毒 (WHV) 病毒血症水平
1. 在持续性鸭乙型肝炎病毒(DHBV)感染的鸭子中,每日口服0.1 mg/kg体重的恩替卡韦,持续244天,可在80天内使血清DHBV DNA水平下降4个对数级,在120天内使血清DHBV表面抗原(DHBsAg)水平下降2-3个对数级 [2] 2. 对DHBV感染的鸭子停用恩替卡韦后,血清DHBV DNA和DHBsAg水平在40天内反弹至与蒸馏水处理组鸭子相当的水平 [2] 3. 恩替卡韦治疗使鸭子肝脏中的DHBV DNA复制中间体减少70倍,而稳定的模板形式——共价闭合环状DNA(cccDNA)的水平仅下降4倍 [2] 4. 恩替卡韦治疗降低了鸭子肝脏中抗原染色的强度和抗原阳性肝细胞的比例,但胆管细胞中的抗原染色强度未受影响 [2] 5. 肌内注射五剂DHBV DNA疫苗(表达前表面、表面、前核心和核心抗原),无论是单独使用还是与恩替卡韦治疗联合使用,均未对DHBV感染鸭子的病毒标志物产生显著影响 [2] |
| 酶活实验 |
BMS-200475 针对 HBV 的 EC50 为 3.75 nM。它被掺入 HBV 的蛋白质引物中,随后抑制逆转录酶的引发步骤。 BMS-200475 对其他 RNA 和 DNA 病毒的抗病毒活性明显较低。恩替卡韦比其他脱氧鸟苷类似物(喷昔洛韦、更昔洛韦、洛布卡韦和阿昔洛韦)或拉米夫定更容易磷酸化为其活性代谢物。恩替卡韦的细胞内半衰期为15小时。
1. 制备包含野生型或拉米夫定耐药HBV Pol(YMDD突变体:M550V/L526M、M550I)的重组HBV核衣壳 [1] 2. 将重组HBV核衣壳与不同浓度的ETV-TP或3TC-TP共同孵育,检测其对HBV Pol活性的抑制作用 [1] 3. 采用四参数逻辑方程绘制抑制曲线,确定ETV-TP和3TC-TP对野生型及突变型HBV Pol的IC₅₀值,并比较两者的抑制效力 [1] |
| 细胞实验 |
BMS 200475 在磷酸盐缓冲盐水 (PBS) 中制备,并用含有 2% 胎牛血清的适当培养基稀释。 HepG2 2.2.15 细胞以每孔 5×105 个细胞的密度接种在 12 孔 Biocoat 胶原蛋白包被的板上,并保持汇合状态 2 至 3 天,然后用 1 mL 掺有 BMS 200475 的培养基覆盖. 第 10 天进行 HBV 定量。
1. 野生型HBV复制实验:将HepG2细胞以感染复数(MOI)100感染野生型BAC-HBV,持续3小时后洗涤,加入含不同浓度恩替卡韦或拉米夫定的RPMI 1640培养基(含5%胎牛血清)培养;在不同时间点采集培养上清,通过DNA斑点杂交分析HBV DNA水平,评估药物的抑制效果 [1] 2. 拉米夫定耐药HBV复制实验:将编码拉米夫定耐药HBV的质粒(pCMV-M550V/L526M或pCMV-M550I)转染至HepG2细胞,转染4小时后洗涤,加入含不同浓度恩替卡韦或拉米夫定的RPMI 1640培养基(含5%胎牛血清);转染后第6天采集培养上清,通过DNA斑点杂交检测HBV DNA水平 [1] 3. 细胞内ETV-TP积累实验:使用浓度为0.2、1.0和5.0 nM的³H标记恩替卡韦(13.9 Ci/mmol)处理HepG2细胞,检测细胞内ETV-TP的积累动力学,评估恩替卡韦在肝癌细胞中的磷酸化效率 [1] |
| 动物实验 |
0.02 to 0.5 mg/kg; oral
Ducks and Wookchucks This study was designed to test the efficacy of antiviral treatment with entecavir (ETV) in combination with DNA vaccines expressing duck hepatitis B virus (DHBV) antigens as a therapy for persistent DHBV infection in ducks. Ducks were inoculated with 10(9) DHBV genomes at 7 days of age, leading to widespread infection of the liver and viremia within 7 days, and were then treated orally with either ETV (0.1 mg/kg of body weight/day) or distilled water from 21 days posthatch for 244 days. Treatment with ETV caused a 4-log drop in serum DHBV DNA levels within 80 days and a slower 2- to 3-log drop in serum DHBV surface antigen (DHBsAg) levels within 120 days. Following withdrawal of ETV, levels of serum DHBV DNA and DHBsAg rebounded to match those in the water-treated animals within 40 days. Sequential liver biopsy samples collected throughout the study showed that ETV treatment reduced DHBV DNA replicative intermediates 70-fold in the liver, while the level of the stable, template form, covalently closed circular DNA decreased only 4-fold. ETV treatment reduced both the intensity of antigen staining and the percentage of antigen-positive hepatocytes in the liver, but the intensity of antigen staining in bile duct cells appeared not to be effected. Intramuscular administration of five doses of a DNA vaccine expressing the DHBV presurface, surface, precore, and core antigens, both alone and concurrently with ETV treatment, on days 50, 64, 78, 127, and 141 did not result in any significant effect on viral markers.[2] Drug administration. Ducks from groups 1 and 2 were weighed three times a week, and ETV at a dose of 0.1 mg/kg/day was administered by gavage to these ducks each day for 244 days. Control ducks (groups 3, 4, and 5) were weighed weekly and given 2 ml of distilled water by gavage daily.[2] 1. Establishment of persistent DHBV infection model: Ducks were inoculated with 10⁹ DHBV genomes at 7 days of age, leading to widespread liver infection and viremia within 7 days [2] 2. Drug administration: Starting from 21 days post-hatch, ducks were treated orally with Entecavir at a dose of 0.1 mg/kg of body weight per day or distilled water for 244 days [2] 3. DNA vaccination: Intramuscular administration of five doses of DHBV DNA vaccine (expressing DHBV presurface, surface, precore, and core antigens) or empty DNA vector on days 50, 64, 78, 127, and 141 post-hatch, either alone or in combination with Entecavir treatment [2] 4. Sample collection and detection: Surgical liver biopsies were performed on days 18, 42, 91, and 181 post-hatch; two ducks from each treatment group were autopsied on day 243 (the day before drug withdrawal), and the remaining ducks were biopsied on day 287 and autopsied on day 298 or 320. Serum DHBV DNA was detected by real-time PCR, serum DHBsAg was quantified by ELISA, and liver tissue was analyzed for total DHBV DNA and cccDNA by Southern blot hybridization; immunoperoxidase staining was used to detect DHBsAg-positive cells in the liver [2] |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Absorption Following oral administration in healthy subjects, entecavir peak plasma concentrations occurred between 0.5 and 1.5 hours. In healthy subjects, the bioavailability of the tablet is 100% relative to the oral solution. renal cl=383.2 +/- 101.8 mL/min [Unimpaired renal function] renal cl=197.9 +/- 78.1 mL/min [Mild impaired renal function] renal cl=135.6 +/- 31.6 mL/min [Moderate impaired renal function] renal cl=40.3 +/- 10.1 mL/min [severe impaired renal function] apparent oral cl=588.1 +/- 153.7 mL/min [Unimpaired renal function] apparent oral cl=309.2 +/- 62.6 mL/min [Mild impaired renal function] apparent oral cl=226.3 +/- 60.1 mL/min [Moderate impaired renal function] apparent oral cl=100.6 +/- 29.1 mL/min [severe impaired renal function] apparent oral cl=50.6 +/- 16.5 mL/min [severe impaired renal function amnaged with Hemodialysis] apparent oral cl=35.7 +/- 19.6 mL/min [severe impaired renal function amnaged with CAPD] The bioavailability of /entecavir/ tablets was /equivalent/ to the oral solution. Oral administration of 0.5 mg of entecavir given with a standard high fat meal resulted in a delayed in absorption (1 to 1.5 hours fed vs. 0.75 hours fasted), a decrease in Cmax of 44% to 46%, and a decrease in AUC of 18% to 20%. /The estimated apparent volume of distribution is in excess of total body water/, entecavir is extensively distributed into tissues. /Binding of entecavir to human serum proteins in vitro is/ low (13%) For more Absorption, Distribution and Excretion (Complete) data for ENTECAVIR (7 total), please visit the HSDB record page. Metabolism / Metabolites Entecavir is not a substrate, inhibitor, or inducer of the cytochrome P450 (CYP450) enzyme system. Entecavir is efficiently phosphorylated to the active triphosphate form. Following administration of 14C-entecavir, no oxidative or acetylated metabolites were observed. Minor amounts of phase II metabolites (glucuronide and sulfate conjugates) were observed. Entecavir is not a substrate, inhibitor, or inducer of the cytochrome P450 enzyme system. Biological Half-Life After reaching peak concentration, entecavir plasma concentrations decreased in a bi-exponential manner with a terminal elimination half-life of approximately 128-149 hours. The phosphorylated metabolite has a half-life of 15 hours. Elimination /half-life is/ approximately 128 to 149 hours. Accumulation /half-life is/ 24 hours |
| 毒性/毒理 (Toxicokinetics/TK) |
Hepatotoxicity
Elevations in serum ALT levels occur in 2% to 10% patients with chronic hepatitis B treated with entecavir. These elevations appear to be due to a transient flare in the underlying chronic hepatitis B and occur both during and after therapy. On treatment, ALT flares typically occur during the first 1 to 2 months of therapy and are mild, asymptomatic and self-limited, accompanying the rapid declines in HBV DNA levels. Withdrawal flares in ALT levels occur in 8% to 12% of patients who receive entecavir therapy of hepatitis B and are subsequently withdrawn from treatment. The withdrawal flares arise within 1 to 3 months of stopping treatment and are usually preceded by marked and sudden rises in HBV DNA levels towards pretreatment values. Withdrawal flares of hepatitis B can be symptomatic and severe, and several instances of acute liver failure have been described in patients withdrawn from therapy after 1 to 3 years of treatment. There have been few reports of withdrawal flares after stopping entecavir, because the majority of patients have continued therapy indefinitely. However, the rate of flares and their severity are likely to be similar after stopping entecavir as after withdrawal of other therapies of hepatitis B. Several instances of lactic acidosis have been reported in patients with advanced hepatitis B who were treated with entecavir; however, lactate levels were reported to be normal in patients with cirrhosis started on entecavir and followed prospectively, and in large clinical trials lactic acidosis has not been reported. The cases of lactic acidosis attributed to entecavir occurred largely in patients with severe, advanced disease and may have been due to septicemia, hypotension and/or hepatic failure rather than an adverse reaction to entecavir. Therapy with entecavir has not been associated with development of the typical syndrome of lactic acidosis, hepatic steatosis and liver failure in patients without severe preexisting liver disease that has been described with stavudine, didanosine and zidovudine treatment. Thus, clinically apparent direct hepatotoxicity from entecavir must be rare, if it occurs at all. Likelihood score: E* (suspected but unproven cause of clinically apparent liver rinjury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Entecavir has not been studied in nursing mothers being treated for hepatitis B infection. An alternate drug may be preferred, especially while nursing a newborn or preterm infant. No differences exist in infection rates between breastfed and formula-fed infants born to hepatitis B-infected women, as long as the infant receives hepatitis B immune globulin and hepatitis B vaccine at birth. Mothers with hepatitis B are encouraged to breastfeed their infants after their infants receive these preventative measures. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding Binding of entecavir to human serum proteins in vitro is approximately 13%. Interactions Potential pharmacokinetic interactions with drugs that reduce renal function or that may compete with entecavir for active renal tubular secretion; increased serum concentrations of entecavir or the concomitantly used drug may occur. Although the effect of concomitant use of such drugs with entecavir has not been specifically studied, patients receiving entecavir in conjunction with other drugs that may affect renal function or are excreted renally should be monitored closely for adverse effects. In vitro evidence indicates that concurrent use of nucleoside reverse transcriptase inhibitors (NRTIs) and entecavir is unlikely to reduce the antiviral efficacy of entecavir against HBV or the antiretroviral activity of NRTIs (e.g., abacavir, didanosine, lamivudine, stavudine, tenofovir disoproxil fumarate, or zidovudine) against HIV. Possible pharmacokinetic interaction (increased entecavir serum concentrations because of altered renal function) with cyclosporine or tacrolimus. Monitor renal function prior to and during entecavir treatment in patients (e.g., transplant patients) receiving cyclosporine, tacrolimus, or other immunosuppressive agents that may affect renal function. |
| 参考文献 | |
| 其他信息 |
Therapeutic Uses
Antiviral Agents Entecavir has been evaluated for the treatment of chronic HBV infection in a phase III, randomized, double-blind, active-controlled study (AI463038) in HIV-infected patients receiving highly active antiretroviral therapy (HAART) that included lamivudine. These patients had recurrent HBV viremia (99% were HBeAg-positive), active HBV replication (median baseline serum HBV DNA levels 9.13 log10 copies/mL), and persistent elevations in serum ALT concentrations (mean serum ALT of 71.5 IU/L). Patients continued HAART (including lamivudine 300 mg daily) and were randomized to receive concurrent therapy with entecavir (1 mg daily) or placebo for 24 weeks followed by an additional 24-week open-label period during which all patients received entecavir (1 mg daily). Analysis of limited data at 24 weeks indicated that 6% of patients who received entecavir in conjunction with lamivudine-containing HAART had undetectable levels of serum HBV DNA (defined as less than 300 copies/mL by PCR assay) compared with 0% of those who received placebo and lamivudine-containing HAART. Thirty-four percent of patients receiving the regimen that included entecavir had normal serum ALT concentrations (i.e., biochemical response) at week 24 compared with 8% of those who did not receive entecavir. In addition, the mean decrease in serum HBV DNA levels from baseline was 3.65 log10 copies/mL at week 24 in those receiving the regimen that included entecavir compared with an increase of 0.11 log10 copies/mL in those receiving a lamivudine-containing HAART regimen alone. Median serum HIV-1 RNA levels remained stable at approximately 2 log10/mL during the 24-week blinded study period. Entecavir has been evaluated for the treatment of lamivudine-refractory chronic HBV infection in a phase III, randomized, double-blind, active-controlled study (AI463026) in adults with active HBV replication (median baseline serum HBV DNA levels 9.36 log10 copies/mL), persistent elevations in serum ALT concentrations (mean serum ALT of 128 IU/L), and histologic evidence of active liver disease (mean Knodell necroinflammatory score of 6.5). 27 Seventy-six percent of patients in the study were male, 37% were Asian, 62% were Caucasian, and 52% had prior treatment with interferon alfa. Patients in the study had previously received lamivudine therapy for a mean duration of 2.7 years and lamivudine-resistant mutations were identified at baseline in 85% of patients. Patients were randomized to switch (without a washout or an overlap period) from lamivudine to entecavir (1 mg daily) or to continue lamivudine (100 mg daily) for 52 weeks. Data analysis at 48 weeks indicated that 55% of patients switched to entecavir had histologic improvement (defined as a reduction of at least 2 points in the Knodell necroinflammatory score with no concurrent worsening of the Knodell fibrosis score) compared with 28% of those who continued to receive lamivudine. Sixty-one percent of patients receiving entecavir had normal serum ALT concentrations (i.e., biochemical response) at week 48 compared with 15% of those receiving lamivudine. In addition, the mean decrease in serum HBV DNA levels from baseline was 5.11 log10 copies/mL at week 48 in those receiving entecavir compared with a decrease of 0.48 log10 copies/mL in those receiving lamivudine. Nineteen percent of patients who received entecavir had undetectable levels of serum HBV DNA (defined as less than 300 copies/mL by PCR assay) at week 48 compared with 1% of those who received lamivudine. Seroconversion to anti-HBe occurred in 8 or 3% of patients who received entecavir or lamivudine, respectively. Approximately 55% of patients treated with entecavir continued treatment for up to 96 weeks; 40% of these patients had undetectable levels of serum HBV DNA, 81% had normal ALT concentrations, and 10% achieved seroconversion. Efficacy of entecavir for the management of HBeAg-negative, anti-HBe- and HBV-DNA-positive chronic HBV infection was evaluated in a phase III, randomized, double-blind, active-controlled study (AI463027) in nucleoside-naive adults with active HBV replication (median baseline serum HBV DNA levels 7.58 log10 copies/mL by a PCR-based assay), persistent elevations in serum ALT concentrations (mean serum ALT of 142 IU/L), and histologic evidence of active liver disease (mean Knodell necroinflammatory score of 7.8). Seventy-six percent of patients in the study were male, 58% were Caucasian, 39% were Asian, and 13% had prior treatment with interferon alfa. Data analysis at 48 weeks indicated that 70% of patients who received entecavir (0.5 mg daily) had histologic improvement (defined as a reduction of at least 2 points in the Knodell necroinflammatory score with no concurrent worsening of the Knodell fibrosis score) compared with 61% of those who received lamivudine (100 mg daily). Serum ALT concentrations also normalized at week 48 in 78% of patients who received entecavir compared with 71% of those who received lamivudine daily. In addition, the mean decrease in serum HBV DNA levels from baseline was 5.04 log10 copies/mL at week 48 in patients receiving entecavir 0.5 mg daily compared with a mean decrease of 4.53 log10 copies/mL in those receiving lamivudine 100 mg daily. Ninety percent of patients who received entecavir had undetectable levels of serum HBV DNA (defined as less than 300 copies/mL by PCR assay) at week 48 compared with 72% of those who received lamivudine. Eighty-five percent of patients treated with entecavir met the response criteria (determined at 48 weeks based on HBV virologic suppression [less than 0.7 MEq/mL by bDNA assay] and loss of HBeAg) and discontinued entecavir at 52 weeks per protocol; very few of these patients had undetectable levels of serum HBV DNA and 46% of patients maintained normal ALT concentrations during an additional 24 weeks of follow-up. For more Therapeutic Uses (Complete) data for ENTECAVIR (6 total), please visit the HSDB record page. Drug Warnings The optimal duration of treatment with entecavir in patients with chronic hepatitis B infection and the relationship between treatment and long-term outcomes such as cirrhosis and hepatocellular carcinoma are unknown. Severe acute exacerbations of hepatitis have occurred following discontinuance of hepatitis B virus (HBV) therapy, including entecavir therapy. In studies that evaluated safety of entecavir, exacerbations of hepatitis or ALT flare was defined as ALT elevations greater than 10 times the upper limit of normal (ULN) and greater than 2 times baseline serum concentrations. In clinical studies (AI463022, AI463027, AI463026), ALT flare occurred in 2, 8, or 12% of nucleoside-naive HBeAg-positive, nucleoside-naive HBeAg-negative, or lamivudine-refractory patients, respectively, following discontinuance of entecavir. The median time to exacerbations of hepatitis was 23 weeks. Rates of post-treatment ALT flare may be higher if entecavir therapy is discontinued without regard to previous response to therapy. FDA Pregnancy Category C; RISK CANNOT BE RULED OUT. Adequate, well controlled human studies are lacking, and animal studies have shown risk to the fetus or are lacking as well. There is a chance of fetal harm if the drug is given during pregnancy; but the potential benefits may outweigh the potential risk. Not known whether entecavir is distributed into milk. Discontinue nursing or the drug, taking into account the importance of the drug to the woman. For more Drug Warnings (Complete) data for ENTECAVIR (15 total), please visit the HSDB record page. Pharmacodynamics Entecavir is a guanosine nucleoside analogue with selective activity against hepatitis B virus (HBV). It is designed to selectively inhibit the Hepatitis B virus, blocking all three steps in the replication process. Entecavir is more efficient than an older Hepatitis B drug, lamivudine. 1. Entecavir (SQ 34676) is a potent and selective inhibitor of HBV replication in vitro and in vivo, and was in clinical trials for the treatment of chronic HBV infections at the time of the study [1] 2. A major limitation of lamivudine (3TC), the current HBV antiviral therapy, is the emergence of drug-resistant HBV in most treated patients due to specific mutations in the nucleotide binding site of HBV Pol [1] 3. The persistence of covalently closed circular DNA (cccDNA) in the liver is a key obstacle to the eradication of HBV infection, as Entecavir only causes a modest reduction in cccDNA levels despite significant inhibition of viral replication [2] 4. Combined treatment with Entecavir and DHBV DNA vaccine did not enhance the antiviral effect in persistent DHBV infection, suggesting that immune-based therapies may need to be optimized to achieve synergistic effects with antiviral drugs [2] |
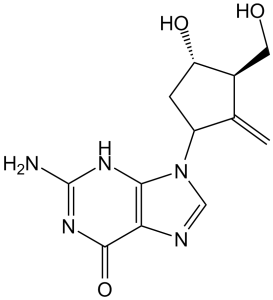
| 分子式 |
C12H15N5O3
|
|---|---|
| 分子量 |
277.28
|
| 精确质量 |
277.117
|
| 元素分析 |
C, 51.98; H, 5.45; N, 25.26; O, 17.31
|
| CAS号 |
142217-69-4
|
| 相关CAS号 |
Entecavir monohydrate;209216-23-9;Entecavir-13C2,15N;(1R,3S,4R)-ent-Entecavir;188399-46-4;Entecavir-d2
|
| PubChem CID |
135398508
|
| 外观&性状 |
White to off-white solid powder
|
| 密度 |
1.8±0.1 g/cm3
|
| 沸点 |
734.2ºC at 760 mmHg
|
| 熔点 |
249-252ºC
|
| 闪点 |
397.9ºC
|
| 折射率 |
1.837
|
| LogP |
-0.96
|
| tPSA |
130.05
|
| 氢键供体(HBD)数目 |
4
|
| 氢键受体(HBA)数目 |
5
|
| 可旋转键数目(RBC) |
2
|
| 重原子数目 |
20
|
| 分子复杂度/Complexity |
480
|
| 定义原子立体中心数目 |
3
|
| SMILES |
O([H])[C@@]1([H])C([H])([H])[C@@]([H])(C(=C([H])[H])[C@]1([H])C([H])([H])O[H])N1C([H])=NC2C(N([H])C(N([H])[H])=NC1=2)=O
|
| InChi Key |
QDGZDCVAUDNJFG-FXQIFTODSA-N
|
| InChi Code |
InChI=1S/C12H15N5O3/c1-5-6(3-18)8(19)2-7(5)17-4-14-9-10(17)15-12(13)16-11(9)20/h4,6-8,18-19H,1-3H2,(H3,13,15,16,20)/t6-,7-,8-/m0/s1
|
| 化学名 |
2-amino-9-[(1S,3R,4S)-4-hydroxy-3-(hydroxymethyl)-2-methylidenecyclopentyl]-3H-purin-6-one
|
| 别名 |
Entecavir; Baraclude; BMS-200475; BMS-200475; BMS-200475; FT-0083013; FT0083013; FT0083013; D07896; SQ 34676; SQ-34676; SQ34676;
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中(例如氮气保护),避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : ≥ 44~55 mg/mL (158.68~198.35 mM)
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 3.6065 mL | 18.0323 mL | 36.0646 mL | |
| 5 mM | 0.7213 mL | 3.6065 mL | 7.2129 mL | |
| 10 mM | 0.3606 mL | 1.8032 mL | 3.6065 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
|
|
|
|
|