| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| 5g |
|
||
| 10g |
|
||
| 25g |
|
||
| Other Sizes |
|

| 靶点 |
H1 Receptor
|
|---|---|
| 体外研究 (In Vitro) |
在预处理的膀胱切片中,Hydroxyzine diHClide 可抑制卡巴胆碱 (10 μM) 诱导的血清素释放,10 μM 时抑制 34%,1 μM 时抑制 25%,0.1 μM 时抑制 17%,持续 60 分钟[1]。
|
| 体内研究 (In Vivo) |
二盐酸羟嗪(12.5 mg/kg、25 mg/kg 和 50 mg/kg ip)几乎没有直接镇痛活性,但仅显着增强吗啡对放电后发声的影响,发声代表大鼠疼痛的情感成分。 Hydroxyzine diHClide (50 mg/kg ip) 可增强吗啡在甩尾试验中的作用,而 Hydroxyzine (12.5 mg/kg ip) 可降低吗啡对大鼠的镇痛作用[3]。
|
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
The absolute bioavailability of hydroxyzine has not been ascertained, as intravenous formulations are unavailable due to a risk of hemolysis. Hydroxyzine is rapidly absorbed from the gastrointestinal tract upon oral administration, reaching its maximum plasma concentration (Tmax) approximately 2 hours following administration. Approximately 70% of hydroxyzine's active metabolite, cetirizine, is excreted unchanged in the urine. The precise extent of renal and fecal excretion in humans has not been determined. The mean volume of distribution is 16.0 ± 3.0 L/kg. Higher concentrations are found in the skin than in the plasma. Clearance of hydroxyzine has been reported to be 31.1 ± 11.1 mL/min/kg in children and 9.8 ± 3.3 mL/min/kg in adults. It is not known if hydroxyzine crosses the placenta or is distributed into milk. Distribution of hydroxyzine into human body tissues and fluids has not been fully characterized. Following administration of hydroxyzine in animals, the drug is widely distributed into most body tissues and fluids with highest concentrations in the liver, lungs, spleen, kidneys, and adipose tissue. The drug is also distributed into bile in animals. Hydroxyzine is rapidly absorbed from the GI tract following oral administration. The distribution into cerebrospinal fluid of 4 structurally similar antihistamines, chlorcyclizine hydrochloride, chlorpheniramine maleate, hydroxyzine hydrochloride (hydroxyzine dihydrochloride), and triprolidine hydrochloride, was studied in Sprague-Dawley rats after the administration of intranasal solutions or intra-arterial injections of solutions of each of the antihistamines; drug concentrations were measured in plasma and cerebrospinal fluid (CSF). Doses of 15.4, 13.3, 8.7, and 16.5 mumol/kg of chlorcyclizine, chlorpheniramine, hydroxyzine, and triprolidine, respectively, were administered. Hydroxyzine plasma and CSF concentrations were significantly greater than most of the other antihistamines. Also, hydroxyzine showed the most rapid absorption into plasma following intranasal administration, and its CSF Cmax values were significantly higher after intranasal administration compared to intra-arterial administration. The ratios of AUC (0-180 min) values for intranasal:intra-arterial administration in CSF and plasma for hydroxyzine were 4 and 0.42 and for triprolidine, the only other antihistamine with measurable CSF concentrations, were 0.54 and 0.66, respectively. For more Absorption, Distribution and Excretion (Complete) data for HYDROXYZINE (8 total), please visit the HSDB record page. Metabolism / Metabolites Hydroxyzine is metabolized in the liver by CYP3A4 and CYP3A5. While the precise metabolic fate of hydroxyzine is unclear, its main and active metabolite (~45 to 60% of an orally administered dose), generated by oxidation of its alcohol moiety to a carboxylic acid, is the second-generation antihistamine [cetirizine]. Hydroxyzine is likely broken down into several other metabolites, though specific structures and pathways have not been elucidated in humans. Pharmacokinetic parameters of hydroxyzine and its active metabolite cetirizine were determined after oral and intravenous administration of 2 mg kg(-1) of hydroxyzine to six healthy dogs. Plasma drug levels were determined with high-pressure liquid chromatography. Pharmacodynamic studies evaluated the suppressive effect on histamine and anticanine IgE-mediated cutaneous wheal formation. Pharmacokinetic and pharmacodynamic correlations were determined with computer modelling. The mean systemic availability of oral hydroxyzine was 72%. Hydroxyzine was rapidly converted to cetirizine regardless of the route of administration. The mean area-under-the-curve was eight and ten times higher for cetirizine than hydroxyzine after intravenous and oral dosing, respectively. After oral administration of hydroxyzine, the mean peak concentration of cetirizine was approximately 2.2 ug mL(-1) and that of hydroxyzine 0.16 ug mL(-1). The terminal half-life for cetirizine varied between 10 and 11 hr after intravenous and oral administration of hydroxyzine. A sigmoidal relationship was fit to the data comparing cetirizine plasma concentration to wheal suppression. Maximum inhibition (82% and 69% for histamine and anticanine IgE-mediated skin reactions, respectively) was observed during the first 8 hr, which correlated with a plasma concentration of cetirizine greater than 1.5 ug mL(-1). Pharmacological modelling suggested that increasing either hydroxyzine dosages or frequencies of administration would not result in histamine inhibition superior to that obtained with twice daily hydroxyzine at 2 mg kg(-1). In conclusion, there was rapid conversion of hydroxyzine to cetirizine. The reduction of wheal formation appeared almost entirely due to cetirizine. Pharmacodynamic modelling predicted that maximal antihistamine effect would occur with twice daily oral administration of hydroxyzine at 2 mg kg(-1). Although the exact metabolic fate of hydroxyzine is not clearly established, it appears that the drug is completely metabolized, principally in the liver. In animals, hydroxyzine and its metabolites are excreted in feces via biliary elimination. The carboxylic acid metabolite of hydroxyzine, cetirizine, is a long-acting antihistamine. Hepatic Half Life: 20 to 25 hours Biological Half-Life The half-life of hydroxyzine is reportedly 14-25 hours, and appears to be, on average, shorter in children (~7.1 hours) than in adults (~20 hours). Elimination half-life is prolonged in the elderly, averaging approximately 29 hours, and is likely to be similarly prolonged in patients with renal or hepatic impairment. Hydroxyzine, a potent H1-receptor antagonist often used for relief of pruritus in patients with hepatic dysfunction, was studied in eight patients, mean age 53.4 +/- SD 11.2 years, with primary biliary cirrhosis. The patients ingested a single dose of hydroxyzine, 0.7 mg/kg (mean dose 43.9 +/- 6.6 mg). Before the dose, then hourly for 6 hours, every 2 hours from 6-12 hours, at 24 hours, and every 24 hours for 6 days, serum hydroxyzine and cetirizine were measured and an intradermal injection of 0.01 mL of a 0.1 mg/mL solution of histamine phosphate was performed. ... The mean serum elimination half-life of hydroxyzine was 36.6 +/- 13.1 hours, and the mean serum elimination half-life of cetirizine was 25.0 +/- 8.2 hours. ... ... The pharmacokinetics and antipruritic effects of hydroxyzine hydrochloride in 12 children, mean age 6.1 +/- 4.6 years, with severe atopic dermatitis /were examined/. After a single 0.7 mg/kg orally administered dose of the drug, ... . The mean elimination half-life was 7.1 +/- 2.3 hours, ... . ... The changes in serum half-life values and clearance rates in dogs who were administered hydroxyzine, 0.7 mg/kg, intramuscularly, daily, for 150 days /were studied/. Pharmacokinetic studies were performed on the first day of drug administration, and on days 30, 60, 90, 120, and 150. The mean serum half-life value on day 30, 60, and 120 was significantly longer (p less than 0.05) than that of 2.4 +/- 0.3 hours obtained on day 1. ... ... The pharmacokinetics and the suppression of histamine-induced wheals, flares, and pruritus in the skin after administration of the histamine H1 antagonist hydroxyzine to seven healthy adults /were studied/. After a single oral dose of hydroxyzine, 0.7 mg/kg (mean dose 39.0 +/- 5.4 mg), ... The mean elimination half-life calculated from the terminal linear portion of the serum hydroxyzine concentration vs. time curve was 20.0 +/- 4.1 hr. ... |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
Hydroxyzine competes with histamine for binding at H1-receptor sites on the effector cell surface, resulting in suppression of histaminic edema, flare, and pruritus. The sedative properties of hydroxyzine occur at the subcortical level of the CNS. Secondary to its central anticholinergic actions, hydroxyzine may be effective as an antiemetic. Hepatotoxicity Despite widespread use, hydroxyzine has not been linked to liver test abnormalities or to clinically apparent liver injury. Indeed, hydroxyzine is commonly used for the pruritus associated with liver disease. The reason for its safety may relate to low daily dose and limited duration of use. Likelihood score: E (unlikely to be a cause of clinically apparent liver injury). References on the safety and potential hepatotoxicity of antihistamines are given together after the Overview section on Antihistamines. Drug Class: Antihistamines Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Small occasional doses of hydroxyzine would not be expected to cause any adverse effects in breastfed infants. Larger doses or more prolonged use may cause drowsiness and other effects in the infant or decrease the milk supply, particularly in combination with a sympathomimetic such as pseudoephedrine or before lactation is well established. Other agents are preferred, especially while nursing a newborn or preterm infant. ◉ Effects in Breastfed Infants In one telephone follow-up study, mothers reported irritability and colicky symptoms 10% of infants exposed to various antihistamines and drowsiness was reported in 1.6% of infants. None of the reactions required medical attention. All adverse reactions in breastfed infants reported in France between January 1985 and June 2011 were compiled by a French pharmacovigilance center. Of 174 reports, hydroxyzine was reported to cause adverse reactions in 8 infants and to be one of the drugs most often suspected in serious adverse reactions, primarily sedation. ◉ Effects on Lactation and Breastmilk Antihistamines in relatively high doses given by injection can decrease basal serum prolactin in nonlactating women and in early postpartum women However, suckling-induced prolactin secretion is not affected by antihistamine pretreatment of postpartum mothers. Whether lower oral doses of antihistamines have the same effect on serum prolactin or whether the effects on prolactin have any consequences on breastfeeding success have not been studied. The prolactin level in a mother with established lactation may not affect her ability to breastfeed. The breastfeeding mother of a 5-week-old infant was diagnosed with bipolar disorder, panic attacks and anxiety disorder. She was started on hydroxyzine 50 mg at an unspecified interval and took it for 3 to 5 days with no effect on milk production. She then started aripiprazole 5 mg at an unspecified interval. After 5 days, she reported a decrease in milk production that required supplementation with formula. Nine days after stopping both drugs, her milk supply returned to normal. The decreased milk supply was possibly caused by the medications, with aripiprazole most likely. Protein Binding Hydroxyzine has been shown to bind to human albumin _in vitro_, but the extent of protein binding in plasma has not been evaluated. Toxicity Data Oral, rat LD50: 950 mg/kg. Interactions Hydroxyzine has been shown to inhibit and reverse the vasopressor effect of epinephrine. If a vasopressor agent is required in patients receiving hydroxyzine, norepinephrine or metaraminol should be used; epinephrine should not be used. Additive anticholinergic effects may occur when hydroxyzine is administered concomitantly with other anticholinergic agents. Hydroxyzine may be additive with, or may potentiate the action of, other CNS depressants such as opiates or other analgesics, barbiturates or other sedatives, anesthetics, or alcohol. When hydroxyzine is used concomitantly with other CNS depressants, caution should be used to avoid excessive sedation, and the manufacturers recommend that dosage of the CNS depressant be reduced by up to 50%. Mechanism of a rise of blood hydroxyzine concentrations due to ethanol administration was investigated used rabbits. When 10 mg/kg hydroxyzine dihydrochloride were orally administered together with 10 mL/kg of 1 to 15% ethanol solution, blood hydroxyzine concentrations rised in all rabbits given ethanol solution more than 10%. When 10 mL/kg of 15% ethanol solution were orally administered at 1, 2 or 3 hours before oral administration of hydroxyzine, blood hydroxyzine concentrations rised markedly in all cases. Blood hydroxyzine concentrations rised little or a little when hydroxyzine were orally administered immediately after intravenous administration of 5 mL/kg of 20% ethanol solution. It was considered that the main mechanism of a rise of blood hydroxyzine concentration was not metabolic interaction between hydroxyzine and ethanol, but an enhancement of intestinal absorption of hydroxyzine due to ethanol. It was also found that hydroxyzine in blood distributed rapidly into bodily tissues. Non-Human Toxicity Values LD50 Rat oral 840 mg/kg LD50 Rat ip 160 mg/kg LD50 Rat iv 45 mg/kg LD50 Mouse oral 480 mg/kg For more Non-Human Toxicity Values (Complete) data for HYDROXYZINE (6 total), please visit the HSDB record page. |
| 参考文献 | |
| 其他信息 |
Therapeutic Uses
Anti-Anxiety Agents; Antiemetics; Antipruritics; Histamine H1 Antagonists; Sedatives, Nonbarbiturate MEDICATION (VET): The efficacy of antihistamines for the treatment of pruritus is highly variable. The most commonly used antihistamines include hydroxyzine hydrochloride ... MEDICATION (VET): In chronic urticaria, antihistamines such as hydroxyzine may be useful ... in horses ... . Hydroxyzine has also been used for the management of agitation caused by acute alcohol withdrawal; to reduce opiate analgesic dosage; to control motion sickness; and to control nausea and vomiting of various etiologies (e.g., postoperative). /Included in US product label/ Hydroxyzine is used for the symptomatic management of anxiety and tension associated with psychoneuroses and as an adjunct in patients with organic disease states who have associated anxiety; for the management of pruritus caused by allergic conditions such as chronic urticaria or atopic or contact dermatoses, and in histamine-mediated pruritus; and for its sedative effects before and after general anesthesia. The efficacy of hydroxyzine as an anxiolytic agent during long-term administration (i.e., longer than 4 months) has not been established; most clinicians believe that benzodiazepines, barbiturates, and meprobamate are more effective than hydroxyzine for anxiety. Patients with a history of long-term therapy with hydroxyzine should be evaluated periodically to determine the efficacy and need for further treatment. Hydroxyzine should not be used as the sole agent for the treatment of depression or psychoses. /Included in US product label/ Drug Warnings Marked local discomfort, sterile abcesses, erythema, local irritation, and tissue necrosis may occur at the site of IM injection, and marked localized subcutaneous tissue induration has been reported as a result of extravasation of the drug. The most frequent adverse effects of hydroxyzine are drowsiness and dry mouth. Drowsiness usually diminishes with continued therapy or reduction in dosage. Other less frequent adverse nervous system effects of hydroxyzine include dizziness, ataxia, weakness, slurred speech, headache, agitation, and increased anxiety. Involuntary motor activity, including tremor and seizures, has occurred rarely, usually in patients receiving higher than recommended dosages of the drug. Patients should be warned that hydroxyzine may impair their ability to perform activities requiring mental alertness or physical coordination (e.g., operating machinery, driving a motor vehicle). Because of the risk of adverse local effects, which may be severe (e.g., gangrene, thrombosis), IM administration of hydroxyzine should be performed with caution to avoid extravasation or inadvertent subcutaneous, IV, or intra-arterial injection. For more Drug Warnings (Complete) data for HYDROXYZINE (11 total), please visit the HSDB record page. Pharmacodynamics Hydroxyzine blocks the activity of histamine to relieve allergic symptoms such as pruritus. Activity at off-targets also allows for its use as a sedative anxiolytic and an antiemetic in certain disease states. Hydroxyzine is relatively fast-acting, with an onset of effect that occurs between 15 and 60 minutes and a duration of action between 4-6 hours. Hydroxyzine may potentiate the effects of central nervous system (CNS) depressants following general anesthesia - patients maintained on hydroxyzine should receive reduced doses of any CNS depressants required. Hydroxyzine is reported to prolong the QT/QTc interval based on postmarketing reports of rare events of Torsade de Pointes, cardiac arrest, and sudden death, and should be used with caution in patients with an increased baseline risk for QTc prolongation. |
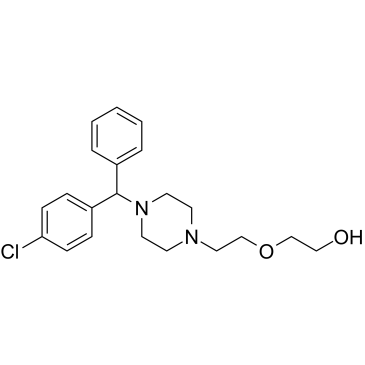
| 分子式 |
C21H27CLN2O2
|
|---|---|
| 分子量 |
374.91
|
| 精确质量 |
374.176
|
| 元素分析 |
C, 67.28; H, 7.26; Cl, 9.46; N, 7.47; O, 8.53
|
| CAS号 |
68-88-2
|
| 相关CAS号 |
Hydroxyzine dihydrochloride; 2192-20-3; Hydroxyzine-d4 dihydrochloride; 1219805-91-0; Hydroxyzine-d8; 1189480-47-4; Hydroxyzine pamoate; 10246-75-0; Hydroxyzine-d4 dihydrochloride; 1244-76-4 (HCl); 5978-92-7 (pamoate ester)
|
| PubChem CID |
3658
|
| 外观&性状 |
Colorless to light yellow solid powder
|
| 沸点 |
220 (0.5 torr)
|
| 熔点 |
190°C
|
| LogP |
2.931
|
| tPSA |
35.94
|
| 氢键供体(HBD)数目 |
1
|
| 氢键受体(HBA)数目 |
4
|
| 可旋转键数目(RBC) |
8
|
| 重原子数目 |
26
|
| 分子复杂度/Complexity |
376
|
| 定义原子立体中心数目 |
0
|
| SMILES |
ClC1=CC=C(C(N2CCN(CCOCCO)CC2)C3=CC=CC=C3)C=C1
|
| InChi Key |
ZQDWXGKKHFNSQK-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C21H27ClN2O2/c22-20-8-6-19(7-9-20)21(18-4-2-1-3-5-18)24-12-10-23(11-13-24)14-16-26-17-15-25/h1-9,21,25H,10-17H2
|
| 化学名 |
2-[2-[4-[(4-chlorophenyl)-phenylmethyl]piperazin-1-yl]ethoxy]ethanol
|
| 别名 |
NSC-169188; NSC169188; Hydroxyzine; NSC 169188; U.C.B 4492
|
| HS Tariff Code |
2933.59.9500
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.6673 mL | 13.3365 mL | 26.6731 mL | |
| 5 mM | 0.5335 mL | 2.6673 mL | 5.3346 mL | |
| 10 mM | 0.2667 mL | 1.3337 mL | 2.6673 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
Effet d’une prémédication sur la douleur, en IRM fonctionnelle, chez des volontaires sains.
CTID: null
Phase: Phase 1, Phase 4 Status: Ongoing
Date: 2009-03-20
|