| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 1mg |
|
||
| 2mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| Other Sizes |
|
| 靶点 |
GLP-1 receptor/glucagon-like peptide-1 receptor
|
|---|---|
| 体外研究 (In Vitro) |
利拉鲁肽与内源性代谢激素 GLP-1 结合相同的受体。利拉鲁肽是一种用于治疗2型糖尿病的注射药物,也可用于治疗患有某些相关合并症的成人肥胖症。利拉鲁肽在 oxLDL 刺激的 Raw264.7 细胞中激活 AMPK/SREBP1 通路[1]。
|
| 体内研究 (In Vivo) |
在 ApoE-/-小鼠模型中,在体内研究了血管反应性和免疫组织化学分析。在给予利拉鲁肽的小鼠中,内皮功能显着改善,这种效果依赖于 GLP-1R。此外,配体霉素治疗可降低主动脉内皮细胞间粘附分子-1 (ICAM-1) 的表达并增加内皮一氧化氮合酶 (eNOS),这两者都依赖于 GLP-1R[3]。利拉鲁肽通过增强增殖来增加胰腺 b 细胞质量,从而降低 T2D 小鼠模型中的高血糖[2]。
促肠促胰岛素模拟物经常用于治疗2型糖尿病,因为它们增强了β细胞对葡萄糖的反应。临床证据显示这些治疗方法(例如,利拉鲁肽)的短期益处是丰富的;然而,最近有几篇关于与肠促胰岛素模拟治疗相关的意外并发症的报道。重要的是,在长期、多年的使用中,这些药物对β细胞和胰岛功能的潜在影响的临床证据仍然缺乏。我们现在表明,在眼前房移植人胰岛的人源化小鼠中,延长每日<强>利拉鲁肽治疗>200天,与人胰岛素释放受损和整体葡萄糖稳态紊乱有关。这些发现引起了人们对糖尿病患者通过模拟肠促胰岛素治疗慢性增强β细胞功能的关注[2]。 胰高血糖素样肽-1受体(GLP-1R)激动剂利拉鲁肽减弱人血管内皮细胞(hVECs)中纤溶酶原激活物抑制剂1型(PAI-1)和血管粘附分子(VAM)表达的诱导,并可能对内皮细胞功能障碍(ECD)(糖尿病血管疾病的早期异常)提供保护。我们的研究旨在建立利拉鲁肽对GLP-1R的体外作用依赖性,并表征其在ECD小鼠模型中的体内作用。体外研究利用人血管内皮细胞系C11-STH和酶联免疫吸附法(ELISA)测定PAI-1和VAM的表达。在ApoE(-/-)小鼠模型中进行了血管反应性和免疫组织化学分析的体内研究。体外研究显示glp - 1r依赖性利拉鲁肽介导的刺激PAI-1和VAM表达的抑制作用。体内研究表明,利拉鲁肽处理小鼠内皮功能显著改善,这是一种GLP-1R依赖效应。利拉鲁肽治疗还增加了内皮一氧化氮合酶(eNOS),降低了主动脉内皮细胞间粘附分子-1 (ICAM-1)的表达,这种作用同样依赖于GLP-1R。这些研究共同确定了GLP-1R激动剂利拉鲁肽对ECD的体内保护作用,并提供了导致这些作用的潜在分子机制。[3] |
| 细胞实验 |
在涂有明胶并补充有含有青霉素/链霉素、20% FCS、20 µg/ml 内皮细胞生长因子和 20 µg/ml 肝素的 Media-199 的 Nunclon 细胞培养皿中,C11-STH 细胞在 37° 下生长直至汇合C。在无血清条件下,C11-STH 细胞单独与 100 nM 利拉鲁肽或 100 nM GLP-1 受体拮抗剂毒蜥外泌肽 (9-39) 一起培养,或与 10 ng/ml TNFα 一起培养 16 小时,或者与利拉鲁肽和/或毒蜥外泌肽(9-39)。使用来自 C11-STH 细胞的条件培养基对 VCAM-1 和 ICAM-1 进行 ELISA 测定来测量蛋白质表达水平。
|
| 动物实验 |
Athymic nude mice
300 μg/kg/day s.c. Islets destined for transplantation into liraglutide-treated diabetic recipients were cultured for 48h in Miami Media supplemented with liraglutide (0.1 nM) (Bohman et al., 2007). Recipient treatment with either liraglutide (300 μg/kg/day s.c.) (Merani et al., 2008) or saline was also started two days prior to transplantation. The rationale for pretreatment was to establish baseline drug levels in the recipient mice before transplantation. Islet transplantation into the anterior chamber of the eye of diabetic nude mice was performed as previously described (Abdulreda et al., 2013; Speier et al., 2008a; Speier et al., 2008b). A total of 1000 human islet equivalents (IEQs) (500 IEQs in each eye) were transplanted into confirmed hyperglycemic nude mouse recipients.[2] |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Bioavailability of liraglutide after subcutaneous injection is approximately 55% and maximum concentrations are reached after 11.7 hours. 6% excreted in urine and 5% excreted in feces. 13L. 1.2L/h. The mean apparent volume of distribution after subcutaneous administration of Victoza 0.6 mg is approximately 13 L. The mean volume of distribution after intravenous administration of Victoza is 0.07 L/kg. Liraglutide is extensively bound to plasma protein (>98%). Following a 3(H)-liraglutide dose, intact liraglutide was not detected in urine or feces. Only a minor part of the administered radioactivity was excreted as liraglutide-related metabolites in urine or feces (6% and 5%, respectively). The majority of urine and feces radioactivity was excreted during the first 6-8 days. The mean apparent clearance following subcutaneous administration of a single dose of liraglutide is approximately 1.2 L/hr with an elimination half-life of approximately 13 hours, making Victoza suitable for once daily administration. Following subcutaneous administration, maximum concentrations of liraglutide are achieved at 8-12 hours post dosing. The mean peak (Cmax) and total (AUC) exposures of liraglutide were 35 ng/mL and 960 ng hr/mL, respectively, for a subcutaneous single dose of 0.6 mg. After subcutaneous single dose administrations, Cmax and AUC of liraglutide increased proportionally over the therapeutic dose range of 0.6 mg to 1.8 mg. At 1.8 mg Victoza, the average steady state concentration of liraglutide over 24 hours was approximately 128 ng/mL. AUC0-8 was equivalent between upper arm and abdomen, and between upper arm and thigh. AUC0-8 from thigh was 22% lower than that from abdomen. However, liraglutide exposures were considered comparable among these three subcutaneous injection sites. Absolute bioavailability of liraglutide following subcutaneous administration is approximately 55%. Liraglutide is a novel once-daily human glucagon-like peptide (GLP)-1 analog in clinical use for the treatment of type 2 diabetes. To study metabolism and excretion of 3(H)-liraglutide, a single subcutaneous dose of 0.75 mg/14.2 MBq was given to healthy males. The recovered radioactivity in blood, urine, and feces was measured, and metabolites were profiled. In addition, 3(H)-liraglutide and [(3)H]GLP-1(7-37) were incubated in vitro with dipeptidyl peptidase-IV (DPP-IV) and neutral endopeptidase (NEP) to compare the metabolite profiles and characterize the degradation products of liraglutide. The exposure of radioactivity in plasma (area under the concentration-time curve from 2 to 24 hr) was represented by liraglutide (> or = 89%) and two minor metabolites (totaling < or =11%). Similarly to GLP-1, liraglutide was cleaved in vitro by DPP-IV in the Ala8-Glu9 position of the N terminus and degraded by NEP into several metabolites. The chromatographic retention time of DPP-IV-truncated liraglutide correlated well with the primary human plasma metabolite [GLP-1(9-37)], and some of the NEP degradation products eluted very close to both plasma metabolites. Three minor metabolites totaling 6 and 5% of the administered radioactivity were excreted in urine and feces, respectively, but no liraglutide was detected. In conclusion, liraglutide is metabolized in vitro by DPP-IV and NEP in a manner similar to that of native GLP-1, although at a much slower rate. The metabolite profiles suggest that both DPP-IV and NEP are also involved in the in vivo degradation of liraglutide. The lack of intact liraglutide excreted in urine and feces and the low levels of metabolites in plasma indicate that liraglutide is completely degraded within the body. For more Absorption, Distribution and Excretion (Complete) data for Liraglutide (8 total), please visit the HSDB record page. Metabolism / Metabolites Liraglutide is less sensitive to metabolism than the endogenous GLP-1 and so is more slowly metabolized by dipeptidyl peptidase-4 and neutral endopeptidase to various smaller polypeptides which have not all been structurally determined. A portion of Liraglutide may be completely metabolized to carbon dioxide and water. The metabolic and excretion patterns were highly similar across species with liraglutide being fully metabolised in the body by sequential cleavage of small peptide fragments and amino acids. The in vitro metabolism studies indicate that the initial metabolism involves cleavage of the peptide backbone with no degradation of the glutamate-palmitic acid side-chain. Mice, rats and monkeys displayed similar plasma profiles and showed no significant gender differences. A higher number of metabolites were observed in plasma from the animal species (especially the rat and monkey) as compared to human plasma. This disparity can partly be explained by differences in the sample preparation as human plasma samples were freeze dried prior to analysis causing a removal of volatile metabolites (including tritiated water). All detected metabolites were minor and obtained in low amount (<15%) and therefore no structural identification of these was performed. This is acceptable since the metabolites are only formed in low amounts and since the metabolites are expected to resemble endogenous substances with well-known metabolic pathways During the initial 24 hours following administration of a single 3(H)-liraglutide dose to healthy subjects, the major component in plasma was intact liraglutide. Liraglutide is endogenously metabolized /SRP: in a manner similar to large proteins/ without a specific organ as a major route of elimination. Biological Half-Life Terminal half life of 13 hours. The terminal half-life of liraglutide seems to be similar in pigs (approximately 14 hr) and humans (approximately 15 hr) while shorter in mice, rats, rabbits and monkeys (4-8 hr). Several studies in monkeys, pigs and humans indicated that extravascular administration (SC and pulmonary) of liraglutide prolongs the terminal half-life as compared to intravenous (IV) administration. Furthermore, the terminal half-life seemed also to be prolonged by repeated dosing in rats, monkeys, pigs and humans. This tendency was not apparent for mice and rabbits. elimination half-life ... approximately 13 hours |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
IDENTIFICATION AND USE: Liraglutide is a clear colorless liquid formulated into solution for subcutaneous use. Liraglutide is a synthetic, long-acting human glucagon-like peptide-1 (GLP-1) receptor agonist (incretin mimetic). It is used as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. HUMAN EXPOSURE AND TOXICITY: Overdoses have been reported in clinical trials and post-marketing use of liraglutide. Effects have included severe nausea and severe vomiting. Post-marketing reports also include acute pancreatitis, including fatal and non-fatal hemorrhagic or necrotizing pancreatitis, serious hypersensitivity reactions (e.g., anaphylactic reactions and angioedema), and acute renal failure and worsening of chronic renal failure (which may require hemodialysis). Liraglutide also causes dose-dependent and treatment-duration-dependent thyroid C-cell tumors at clinically relevant exposures in both genders of rats and mice. It is unknown whether liraglutide causes thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), in humans, as human relevance could not be ruled out by clinical or nonclinical studies. Therefore, liraglutide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) and in patients with multiple endocrine neoplasia syndrome type 2 (MEN 2). Finally, there are no adequate and well-controlled studies of liraglutide in pregnant women; however the drug did cause developmental toxicity in experimental animals. Therefore, liraglutide should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. ANIMAL STUDIES: Liraglutide had no adverse effects on fertility when given to male rats at doses up to 1.0 mg/kg/day. However, liraglutide caused developmental toxicity in both rats and rabbits. When female rats were given subcutaneous doses of 0.1, 0.25 and 1.0 mg/kg/day, the number of early embryonic deaths in the 1 mg/kg/day group increased slightly. Fetal abnormalities and variations in kidneys and blood vessels, irregular ossification of the skull, and a more complete state of ossification occurred at all doses. Mottled liver and minimally kinked ribs occurred at the highest dose. The incidences of fetal malformations in liraglutide-treated groups were misshapen oropharynx and/or narrowed opening into larynx at 0.1 mg/kg/day and umbilical hernia at 0.1 and 0.25 mg/kg/day. In a rabbit developmental study, pregnant females were administered liraglutide subcutaneously at doses of 0.01, 0.025 and 0.05 mg/kg/day from gestation day 6 through day 18 inclusive. Fetal weight was decreased and the incidence of total major fetal abnormalities was increased at all dose levels tested. Single cases of microphthalmia were noted at all dose levels. In addition, there was an increase in the fetal incidence of connected parietals in the high dose group, and a single case of split sternum in the 0.025 and 0.05 mg/kg/day. Minor abnormalities considered to be treatment-related were an increase in the incidence of jugal(s) connected/fused to maxilla at all dose levels and an increase in the incidence of bilobed/bifurcated gallbladder at 0.025 and 0.50 mg/kg/day. Studies for the carcinogenicity potential of liraglutide were also conducted in mice and rats. In both species, a dose-related increase in benign thyroid C-cell adenomas and malignant C-cell carcinomas were observed. Also, there was a treatment-related increase in the incidence and severity of focal C-cell hyperplasia in both male and female rats. In addition, there was a treatment-related increase in fibrosarcomas on the dorsal skin and subcutis, the body surface used for drug injection, in male mice. These fibrosarcomas were attributed to the high local concentration of drug near the injection site. Finally, liraglutide was negative with and without metabolic activation in the Ames test for mutagenicity and in a human peripheral blood lymphocyte chromosome aberration test for clastogenicity. Liraglutide was negative in repeat-dose in vivo micronucleus tests in rats. Hepatotoxicity In large clinical trials, serum enzyme elevations were no more common with liraglutide therapy than with placebo or comparator agents, and no instances of clinically apparent liver injury were reported. Since licensure, there has been a single case report of autoimmune hepatitis arising in a patient taking liraglutide. She did not improve with stopping liraglutide and ultimately required long term corticosteroid therapy, suggesting that the autoimmune hepatitis was independent of the drug therapy or that liraglutide triggered an underlying condition. Other cases of hepatotoxicity due to liraglutide have not been published and the product label does not list liver injury as an adverse event. Thus, liver injury due to liraglutide must be quite rare. Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation No information is available on the excretion of liraglutide int milk or it clinical use during breastfeeding. Because liraglutide is a large peptide molecule with a molecular weight of 3751 daltons, the amount in milk is likely to be very low and absorption is unlikely because it is probably destroyed in the infant's gastrointestinal tract. Until more data become available, liraglutide should be used with caution during breastfeeding, especially while nursing a newborn or preterm infant. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding >98%. Interactions A single dose of an oral contraceptive combination product containing 0.03 mg ethinylestradiol and 0.15 mg levonorgestrel was administered under fed conditions and 7 hours after the dose of Victoza at steady state. Victoza lowered ethinylestradiol and levonorgestrel Cmax by 12% and 13%, respectively. There was no effect of Victoza on the overall exposure (AUC) of ethinylestradiol. Victoza increased the levonorgestrel AUC0-8 by 18%. Victoza delayed Tmax for both ethinylestradiol and levonorgestrel by 1.5 hr. A single dose of digoxin 1 mg was administered 7 hours after the dose of Victoza at steady state. The concomitant administration with Victoza resulted in a reduction of digoxin AUC by 16%; Cmax decreased by 31%. Digoxin median time to maximal concentration (Tmax) was delayed from 1 hr to 1.5 hr. A single dose of lisinopril 20 mg was administered 5 minutes after the dose of Victoza at steady state. The co-administration with Victoza resulted in a reduction of lisinopril AUC by 15%; Cmax decreased by 27%. Lisinopril median Tmax was delayed from 6 hr to 8 hr with Victoza. Victoza did not change the overall exposure (AUC) of griseofulvin following co-administration of a single dose of griseofulvin 500 mg with Victoza at steady state. Griseofulvin Cmax increased by 37% while median Tmax did not change. For more Interactions (Complete) data for Liraglutide (8 total), please visit the HSDB record page. |
| 参考文献 | |
| 其他信息 |
Therapeutic Uses
Hypoglycemic Agents Victoza is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. /Included in US product label/ Because of the uncertain relevance of the rodent thyroid C-cell tumor findings to humans, prescribe Victoza only to patients for whom the potential benefits are considered to outweigh the potential risk. Victoza is not recommended as first-line therapy for patients who have inadequate glycemic control on diet and exercise. ... Victoza is not a substitute for insulin. Victoza should not be used in patients with type 1 diabetes mellitus or for the treatment of diabetic ketoacidosis, as it would not be effective in these settings. EXPL THER: According to World Health Organization estimates, type 2 diabetes (T2D) is an epidemic (particularly in under developed countries) and a socio-economic challenge. This is even more relevant since increasing evidence points to T2D as a risk factor for Alzheimer's disease (AD), supporting the hypothesis that AD is a "type 3 diabetes" or "brain insulin resistant state". Despite the limited knowledge on the molecular mechanisms and the etiological complexity of both pathologies, evidence suggests that neurodegeneration/death underlying cognitive dysfunction (and ultimately dementia) upon long-term T2D may arise from a complex interplay between T2D and brain aging. Additionally, decreased brain insulin levels/signaling and glucose metabolism in both pathologies further suggests that an effective treatment strategy for one disorder may be also beneficial in the other. In this regard, one such promising strategy is a novel successful anti-T2D class of drugs, the glucagon-like peptide-1 (GLP-1) mimetics (e.g. exendin-4 or liraglutide), whose potential neuroprotective effects have been increasingly shown in the last years. In fact, several studies showed that, besides improving peripheral (and probably brain) insulin signaling, GLP-1 analogs minimize cell loss and possibly rescue cognitive decline in models of AD, Parkinson's (PD) or Huntington's disease. Interestingly, exendin-4 is undergoing clinical trials to test its potential as an anti-PD therapy. Herewith, we aim to integrate the available data on the metabolic and neuroprotective effects of GLP-1 mimetics in the central nervous system (CNS) with the complex crosstalk between T2D-AD, as well as their potential therapeutic value against T2D-associated cognitive dysfunction. C Drug Warnings /BOXED WARNING/ WARNING: RISK OF THYROID C-CELL TUMORS. Liraglutide causes dose-dependent and treatment-duration-dependent thyroid C-cell tumors at clinically relevant exposures in both genders of rats and mice. It is unknown whether Victoza causes thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), in humans, as human relevance could not be ruled out by clinical or nonclinical studies. Victoza is contraindicated in patients with a personal or family history of MTC and in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Based on the findings in rodents, monitoring with serum calcitonin or thyroid ultrasound was performed during clinical trials, but this may have increased the number of unnecessary thyroid surgeries. It is unknown whether monitoring with serum calcitonin or thyroid ultrasound will mitigate human risk of thyroid C-cell tumors. Patients should be counseled regarding the risk and symptoms of thyroid tumors. There have been postmarketing reports of serious hypersensitivity reactions (e.g., anaphylactic reactions and angioedema) in patients treated with Victoza. If a hypersensitivity reaction occurs, the patient should discontinue Victoza and other suspect medications and promptly seek medical advice. Based on spontaneous postmarketing reports, acute pancreatitis, including fatal and non-fatal hemorrhagic or necrotizing pancreatitis, has been observed in patients treated with Victoza. After initiation of Victoza, observe patients carefully for signs and symptoms of pancreatitis (including persistent severe abdominal pain, sometimes radiating to the back and which may or may not be accompanied by vomiting). If pancreatitis is suspected, Victoza should promptly be discontinued and appropriate management should be initiated. If pancreatitis is confirmed, Victoza should not be restarted. Consider antidiabetic therapies other than Victoza in patients with a history of pancreatitis. In postmarketing reports, acute renal failure and worsening of chronic renal failure (which may require hemodialysis) have been reported with liraglutide. Some of these events occurred in patients without known underlying renal disease. Most of these events occurred in patients experiencing nausea, vomiting, diarrhea, or dehydration. Some of these events occurred in patients receiving liraglutide in combination with one or more agents known to affect renal function or hydration status. Liraglutide has not been found to be directly nephrotoxic in preclinical or clinical studies. Renal effects usually have been reversible with supportive treatment and discontinuance of potentially causative agents, including liraglutide. Clinicians should use caution when initiating liraglutide or escalating dosage in patients with renal impairment. For more Drug Warnings (Complete) data for Liraglutide (15 total), please visit the HSDB record page. Pharmacodynamics Liraglutide is a once-daily GLP-1 derivative for the treatment of type 2 diabetes. The prolonged action of liraglutide is achieved by attaching a fatty acid molecule at position 26 of the GLP-1 molecule, enabling it to bind reversibly to albumin within the subcutaneous tissue and bloodstream and be released slowly over time. Binding with albumin results in slower degradation and reduced elimination of liraglutide from the circulation by the kidneys compared to GLP-1. The effect of liraglutide is the increased secretion of insulin and decreased secretion of glucagon in response to glucose as well as slower gastric emptying. Liraglutide also does not adversely affect glucagon secretion in response to low blood sugar. |
| 分子式 |
C172H265N43O51
|
|---|---|
| 分子量 |
3751.2020
|
| 精确质量 |
3748.95
|
| 元素分析 |
C, 55.07; H, 7.12; N, 16.06; O, 21.75
|
| CAS号 |
204656-20-2
|
| 相关CAS号 |
Liraglutide-d8 triTFA; Liraglutide-13C5,15N tetraTFA
|
| PubChem CID |
16134956
|
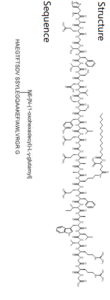
| 序列 |
His-Ala-Glu-Gly-Thr-Phe-Thr-Ser-Asp-Val-Ser-Ser-Tyr-Leu-Glu-Gly-Gln-Ala-Ala-{Lys-N6-[N-(1-oxohexadecyl)-L-g-glutamyl]}-Glu-Phe-Ile-Ala-Trp-Leu-Val-Arg-Gly-Arg-Gly
|
| 短序列 |
HAEGTFTSDVSSYL-{N6-[N-(1-oxohexadecyl)-L-γ-Etamyl]-Glu}-GQAAKEFIAWLVRGRG; HAEGTFTSDVSSYLEGQAA-{Lys-N6-[N-(1-oxohexadecyl)-L-g-glutamyl]}-EFIAWLVRGRG
|
| 外观&性状 |
White to off-white solid powder
|
| LogP |
6.129
|
| tPSA |
1513.76
|
| 氢键供体(HBD)数目 |
54
|
| 氢键受体(HBA)数目 |
55
|
| 可旋转键数目(RBC) |
132
|
| 重原子数目 |
266
|
| 分子复杂度/Complexity |
8760
|
| 定义原子立体中心数目 |
31
|
| SMILES |
O=C([C@]([H])(C([H])([H])C([H])(C([H])([H])[H])C([H])([H])[H])N([H])C([C@]([H])(C([H])([H])C1=C([H])N([H])C2=C([H])C([H])=C([H])C([H])=C12)N([H])C([C@]([H])(C([H])([H])[H])N([H])C([C@]([H])([C@@]([H])(C([H])([H])[H])C([H])([H])C([H])([H])[H])N([H])C([C@]([H])(C([H])([H])C1C([H])=C([H])C([H])=C([H])C=1[H])N([H])C([C@]([H])(C([H])([H])C([H])([H])C(=O)O[H])N([H])C([C@]([H])(C([H])([H])C([H])([H])C([H])([H])C([H])([H])N([H])C(C([H])([H])C([H])([H])[C@@]([H])(C(=O)O[H])N([H])C(C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])C([H])([H])[H])=O)=O)N([H])C([C@]([H])(C([H])([H])[H])N([H])C([C@]([H])(C([H])([H])[H])N([H])C([C@]([H])(C([H])([H])C([H])([H])C(N([H])[H])=O)N([H])C(C([H])([H])N([H])C([C@]([H])(C([H])([H])C([H])([H])C(=O)O[H])N([H])C([C@]([H])(C([H])([H])C([H])(C([H])([H])[H])C([H])([H])[H])N([H])C([C@]([H])(C([H])([H])C1C([H])=C([H])C(=C([H])C=1[H])O[H])N([H])C([C@]([H])(C([H])([H])O[H])N([H])C([C@]([H])(C([H])([H])O[H])N([H])C([C@]([H])(C([H])(C([H])([H])[H])C([H])([H])[H])N([H])C([C@]([H])(C([H])([H])C(=O)O[H])N([H])C([C@]([H])(C([H])([H])O[H])N([H])C([C@]([H])([C@@]([H])(C([H])([H])[H])O[H])N([H])C([C@]([H])(C([H])([H])C1C([H])=C([H])C([H])=C([H])C=1[H])N([H])C([C@]([H])([C@@]([H])(C([H])([H])[H])O[H])N([H])C(C([H])([H])N([H])C([C@]([H])(C([H])([H])C([H])([H])C(=O)O[H])N([H])C([C@]([H])(C([H])([H])[H])N([H])C([C@]([H])(C([H])([H])C1=C([H])N=C([H])N1[H])N([H])[H])=O)=O)=O)=O)=O)=O)=O)=O)=O)=O)=O)=O)=O)=O)=O)=O)=O)=O)=O)=O)=O)=O)=O)=O)=O)N([H])[C@]([H])(C(N([H])[C@]([H])(C(N([H])C([H])([H])C(N([H])[C@]([H])(C(N([H])C([H])([H])C(=O)O[H])=O)C([H])([H])C([H])([H])C([H])([H])N([H])/C(=N/[H])/N([H])[H])=O)=O)C([H])([H])C([H])([H])C([H])([H])N([H])/C(=N/[H])/N([H])[H])=O)C([H])(C([H])([H])[H])C([H])([H])[H]
|
| InChi Key |
YSDQQAXHVYUZIW-QCIJIYAXSA-N
|
| InChi Code |
InChI=1S/C172H265N43O51/c1-18-20-21-22-23-24-25-26-27-28-29-30-37-53-129(224)195-116(170(265)266)59-64-128(223)180-68-41-40-50-111(153(248)199-115(62-67-135(232)233)154(249)204-120(73-100-44-33-31-34-45-100)159(254)214-140(93(11)19-2)167(262)192-97(15)146(241)201-122(76-103-79-183-108-49-39-38-48-106(103)108)157(252)203-118(72-90(5)6)158(253)212-138(91(7)8)165(260)200-110(52-43-70-182-172(177)178)149(244)184-81-130(225)193-109(51-42-69-181-171(175)176)148(243)187-84-137(236)237)196-144(239)95(13)189-143(238)94(12)191-152(247)114(58-63-127(174)222)194-131(226)82-185-151(246)113(61-66-134(230)231)198-155(250)117(71-89(3)4)202-156(251)119(75-102-54-56-105(221)57-55-102)205-162(257)124(85-216)208-164(259)126(87-218)209-166(261)139(92(9)10)213-161(256)123(78-136(234)235)206-163(258)125(86-217)210-169(264)142(99(17)220)215-160(255)121(74-101-46-35-32-36-47-101)207-168(263)141(98(16)219)211-132(227)83-186-150(245)112(60-65-133(228)229)197-145(240)96(14)190-147(242)107(173)77-104-80-179-88-188-104/h31-36,38-39,44-49,54-57,79-80,88-99,107,109-126,138-142,183,216-221H,18-30,37,40-43,50-53,58-78,81-87,173H2,1-17H3,(H2,174,222)(H,179,188)(H,180,223)(H,184,244)(H,185,246)(H,186,245)(H,187,243)(H,189,238)(H,190,242)(H,191,247)(H,192,262)(H,193,225)(H,194,226)(H,195,224)(H,196,239)(H,197,240)(H,198,250)(H,199,248)(H,200,260)(H,201,241)(H,202,251)(H,203,252)(H,204,249)(H,205,257)(H,206,258)(H,207,263)(H,208,259)(H,209,261)(H,210,264)(H,211,227)(H,212,253)(H,213,256)(H,214,254)(H,215,255)(H,228,229)(H,230,231)(H,232,233)(H,234,235)(H,236,237)(H,265,266)(H4,175,176,181)(H4,177,178,182)/t93-,94-,95-,96-,97-,98+,99+,107-,109-,110-,111-,112-,113-,114-,115-,116-,117-,118-,119-,120-,121-,122-,123-,124-,125-,126-,138-,139-,140-,141-,142-/m0/s1
|
| 化学名 |
(2S)-5-[[(5S)-5-[[(2S)-2-[[(2S)-2-[[(2S)-5-amino-2-[[2-[[(2S)-2-[[(2S)-2-[[(2S)-2-[[(2S)-2-[[(2S)-2-[[(2S)-2-[[(2S)-2-[[(2S)-2-[[(2S,3R)-2-[[(2S)-2-[[(2S,3R)-2-[[2-[[(2S)-2-[[(2S)-2-[[(2S)-2-amino-3-(1H-imidazol-5-yl)propanoyl]amino]propanoyl]amino]-4-carboxybutanoyl]amino]acetyl]amino]-3-hydroxybutanoyl]amino]-3-phenylpropanoyl]amino]-3-hydroxybutanoyl]amino]-3-hydroxypropanoyl]amino]-3-carboxypropanoyl]amino]-3-methylbutanoyl]amino]-3-hydroxypropanoyl]amino]-3-hydroxypropanoyl]amino]-3-(4-hydroxyphenyl)propanoyl]amino]-4-methylpentanoyl]amino]-4-carboxybutanoyl]amino]acetyl]amino]-5-oxopentanoyl]amino]propanoyl]amino]propanoyl]amino]-6-[[(2S)-1-[[(2S)-1-[[(2S,3S)-1-[[(2S)-1-[[(2S)-1-[[(2S)-1-[[(2S)-1-[[(2S)-5-carbamimidamido-1-[[2-[[(2S)-5-carbamimidamido-1-(carboxymethylamino)-1-oxopentan-2-yl]amino]-2-oxoethyl]amino]-1-oxopentan-2-yl]amino]-3-methyl-1-oxobutan-2-yl]amino]-4-methyl-1-oxopentan-2-yl]amino]-3-(1H-indol-3-yl)-1-oxopropan-2-yl]amino]-1-oxopropan-2-yl]amino]-3-methyl-1-oxopentan-2-yl]amino]-1-oxo-3-phenylpropan-2-yl]amino]-4-carboxy-1-oxobutan-2-yl]amino]-6-oxohexyl]amino]-2-(hexadecanoylamino)-5-oxopentanoic acid
|
| 别名 |
NNC 90-1170; Liraglutide; NN 2211; NN-2211; NN2211; trade names: Saxenda; Victoza; Liraglutida; Liraglutidum
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中(例如氮气保护),避免吸湿/受潮和光照。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO: ~100 mg/mL (~26.7 mM)
Water: 5~10 mg/mL (adjust pH to 3~4 with 1 M HCl) Ethanol: ~100 mg/mL |
|---|---|
| 溶解度 (体内实验) |
如何溶解多肽,详情请参考右上角《产品说明书》第3页:“多肽溶解指南”。
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。 注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 0.2666 mL | 1.3329 mL | 2.6658 mL | |
| 5 mM | 0.0533 mL | 0.2666 mL | 0.5332 mL | |
| 10 mM | 0.0267 mL | 0.1333 mL | 0.2666 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
Saxenda: Underlying Mechanisms and Clinical Outcomes
CTID: NCT02944500
Phase: Phase 4 Status: Active, not recruiting
Date: 2024-10-01
|