| 规格 | 价格 | |
|---|---|---|
| 500mg | ||
| 1g | ||
| Other Sizes |
| 靶点 |
Tetracyclic antidepressant; Adrenergic Receptor
|
|---|---|
| 体外研究 (In Vitro) |
当暴露于马普替林 (10 μM) 时,会诱导细胞凋亡,并且 HCC 细胞对索拉非尼 (2 μM) 变得更加敏感 [2]。在 HepG2 和 Huh7 细胞中,马普替林(0、10 或 20 μM,72 小时)通过作用于 ERK 通路来抑制 SREBP2 的磷酸化 [2]。在 HCC 细胞中,马普替林可能通过靶向 CRABP1 来调节胆固醇的产生 [2]。细胞侵袭测试[2]
|
| 体内研究 (In Vivo) |
通过将合成大麻素 WIN 55,212-2 与马普替林(3、10 或 30 mg/kg;腹膜内注射)相结合,可以有效减轻神经性疼痛 [1]。马普替林(0、20 或 40 mg/kg)对器官、免疫系统和造血功能具有低毒性;腹腔内;每周两次; 3周[2]。通过阻断胆固醇产生并与 CRABP1 相互作用,马普替林(0、20 或 40 mg/kg;腹腔注射;每周两次;3 周)抑制 HCC 细胞的发育和转移 [2]。
|
| 酶活实验 |
许多药物阻断延迟整流K+通道,延长心脏动作电位持续时间。在这里,我们研究了马普替林对HEK-293细胞和非洲爪蟾卵母细胞中表达的人乙醚-a-go-go相关基因(HERG) K+通道电压依赖性阻断的分子机制。0 mV下对HERG表达的HEK-293细胞和卵母细胞的IC50分别为5.2和23.7微米。马普罗替林对卵母细胞中HERG表达的阻断作用随着膜的渐进式去极化而增强,并伴随着通道激活的电压依赖性的负移。马普替林的效价通过关键芳香残基F656T的点突变降低了7倍,Y652A的点突变降低了3倍,均位于S6结构域。突变Y652A逆转了马普罗替林对HERG通道阻滞的电压依赖性。综上所述,这些结果表明HERG的电压依赖性阻断是由于药物结合位点的关键成分Y652的可及性发生了门压依赖性变化。Eur J Pharmacol . 2006 Feb 15;531(1-3):1-8.
|
| 细胞实验 |
细胞侵袭测试 [2]
细胞类型:人肝癌细胞系 Huh7 和 HepG2 测试浓度: 0、10、20 μM 孵化持续时间:24小时 实验结果:抑制肝癌细胞迁移和上皮间质转化(EMT)。 细胞活力测定 [2] 细胞类型:人肝癌细胞系 Huh7 和 HepG2 测试浓度: 0、10、 20 μM 孵育时间:0、24、48、72、96、120 小时 实验结果:触发细胞凋亡和以剂量和时间依赖性方式抑制 Huh7 和 HepG2 细胞的细胞活力。 蛋白质印迹分析 [2] 细胞类型: 人肝癌细胞系 Huh7 和 HepG2 测试浓度: 0、10、 20 μM 孵育时间:72小时 实验结果:抑制肝癌细胞中的胆固醇生物合成。 |
| 动物实验 |
Animal/Disease Models: Male Balb-c mouse (25-30 g) [1]
Doses: 3, 10, 30 mg/kg Route of Administration: intraperitoneal (ip) injection; assessment 30 minutes after treatment Experimental Results: Pain-related behaviors in neuropathic mice weaken. Animal/Disease Models: Nude mice (BALB/C nu/nu, 4-6 weeks old, female) [2] Doses: 40 mg/kg Route of Administration: intraperitoneal (ip) injection; twice a week; 3-week Experimental Results: diminished serum and tumor cholesterol levels, inhibited the growth of Huh7-derived tumor xenografts without obvious toxic effects. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Slowly, but completely absorbed from the GI tract following oral administration. Approximately 60% of a single orally administered dose is excreted in urine as conjugated metabolites within 21 days; 30% is eliminated in feces. Maprotiline and its metabolites may be detected in the lungs, liver, brain, and kidneys; lower concentrations may be found in the adrenal glands, heart and muscle. Maprotiline is readily distributed into breast milk to similar concentrations as those in maternal blood. Metabolism / Metabolites Hepatic. Maprotiline is metabolized by N-demethylation, deamination, aliphatic and aromatic hydroxylations and by formation of aromatic methoxy derivatives. It is slowly metabolized primarily to desmethylmaprotiline, a pharmacologically active metabolite. Desmethylmaprotiline may undergo further metabolism to maprotiline-N-oxide. Maprotiline has known human metabolites that include 2-hydroxy-maprotiline, desmethylmaprotiline, and 3-hydroxy-maprotiline. Hepatic. Maprotiline is metabolized by N-demethylation, deamination, aliphatic and aromatic hydroxylations and by formation of aromatic methoxy derivatives. It is slowly metabolized primarily to desmethylmaprotiline, a pharmacologically active metabolite. Desmethylmaprotiline may undergo further metabolism to maprotiline-N-oxide. Route of Elimination: Approximately 60% of a single orally administered dose is excreted in urine as conjugated metabolites within 21 days; 30% is eliminated in feces. Half Life: Average ~ 51 hours (range: 27-58 hours) Biological Half-Life Average ~ 51 hours (range: 27-58 hours) |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
Maprotiline exerts its antidepressant action by inhibition of presynaptic uptake of catecholamines, thereby increasing their concentration at the synaptic clefts of the brain. In single doses, the effect of maprotiline on the EEG revealed a rise in the alpha-wave density, a reduction of the alpha-wave frequency and an increase in the alpha-wave amplitude. However, as with other tricyclic antidepressants, maprotiline lowers the convulsive threshold. Maprotiline acts as an antagonist at central presynaptic α2-adrenergic inhibitory autoreceptors and hetero-receptors, an action that is postulated to result in an increase in central noradrenergic and serotonergic activity. Maprotiline is also a moderate peripheral α1 adrenergic antagonist, which may explain the occasional orthostatic hypotension reported in association with its use. Maprotiline also inhibits the amine transporter, delaying the reuptake of noradrenaline and norepinephrine. Lastly, maprotiline is a strong inhibitor of the histamine H1 receptor, which explains its sedative actions. Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Because there is little published experience with maprotiline during breastfeeding, other agents may be preferred, especially while nursing a newborn or preterm infant. ◉ Effects in Breastfed Infants Although it is structurally a tetracyclic compound, maprotiline has pharmacologic actions similar to the tricyclic antidepressants. Follow-up for 1 to 3 years in a group of 20 breastfed infants whose mothers were taking a tricyclic antidepressant found no adverse effects on growth and development. Two small controlled studies indicate that other tricyclic antidepressants have no adverse effect on infant development. In another study, 25 infants whose mothers took a tricyclic antidepressant during pregnancy and lactation were assessed formally between 15 to 71 months and found to have normal growth and development. One of the mothers was taking maprotiline. ◉ Effects on Lactation and Breastmilk Maprotiline has caused increased serum prolactin levels and galactorrhea in nonpregnant, nonnursing patients. The clinical relevance of these findings in nursing mothers is not known. The prolactin level in a mother with established lactation may not affect her ability to breastfeed. An observational study looked at outcomes of 2859 women who took an antidepressant during the 2 years prior to pregnancy. Compared to women who did not take an antidepressant during pregnancy, mothers who took an antidepressant during all 3 trimesters of pregnancy were 37% less likely to be breastfeeding upon hospital discharge. Mothers who took an antidepressant only during the third trimester were 75% less likely to be breastfeeding at discharge. Those who took an antidepressant only during the first and second trimesters did not have a reduced likelihood of breastfeeding at discharge. The antidepressants used by the mothers were not specified. A retrospective cohort study of hospital electronic medical records from 2001 to 2008 compared women who had been dispensed an antidepressant during late gestation (n = 575) to those who had a psychiatric illness but did not receive an antidepressant (n = 1552) and mothers who did not have a psychiatric diagnosis (n = 30,535). Women who received an antidepressant were 37% less likely to be breastfeeding at discharge than women without a psychiatric diagnosis, but no less likely to be breastfeeding than untreated mothers with a psychiatric diagnosis. None of the mothers were taking maprotiline. In a study of 80,882 Norwegian mother-infant pairs from 1999 to 2008, new postpartum antidepressant use was reported by 392 women and 201 reported that they continued antidepressants from pregnancy. Compared with the unexposed comparison group, late pregnancy antidepressant use was associated with a 7% reduced likelihood of breastfeeding initiation, but with no effect on breastfeeding duration or exclusivity. Compared with the unexposed comparison group, new or restarted antidepressant use was associated with a 63% reduced likelihood of predominant, and a 51% reduced likelihood of any breastfeeding at 6 months, as well as a 2.6-fold increased risk of abrupt breastfeeding discontinuation. Specific antidepressants were not mentioned. Protein Binding 88% Toxicity Data LD50: 900 mg/kg (Oral, Rat) (A308) LD50: 90 mg/kg (Oral, Human) (A308) |
| 参考文献 |
[1]. Gunduz O, et al. Analysis of the anti-allodynic effects of combination of a synthetic cannabinoid and a selective noradrenaline re-uptake inhibitor in nerve injury-induced neuropathic mice. Eur J Pain. 2016 Mar. 20(3):465-71.
[2]. Zheng C, et al. Maprotiline Suppresses Cholesterol Biosynthesis and Hepatocellular Carcinoma Progression Through Direct Targeting of CRABP1. Front Pharmacol. 2021 May 20. 12:689767. |
| 其他信息 |
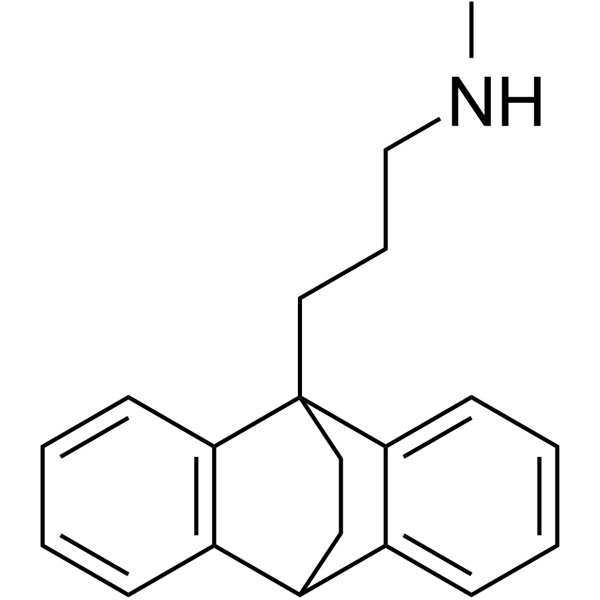
Maprotiline is a member of anthracenes.
Maprotiline is a tetracyclic antidepressant with similar pharmacological properties to tricyclic antidepressants (TCAs). Similar to TCAs, maprotiline inhibits neuronal norepinephrine reuptake, possesses some anticholinergic activity, and does not affect monoamine oxidase activity. It differs from TCAs in that it does not appear to block serotonin reuptake. Maprotiline may be used to treat depressive affective disorders, including dysthymic disorder (depressive neurosis) and major depressive disorder. Maprotiline is effective at reducing symptoms of anxiety associated with depression. Maprotiline is a tetracyclic antidepressant with similar pharmacological properties to tricyclic antidepressants (TCAs). Similar to TCAs, maprotiline inhibits neuronal norepinephrine reuptake, possesses some anticholinergic activity, and does not affect monoamine oxidase activity. It differs from TCAs in that it does not appear to block serotonin reuptake. Maprotiline may be used to treat depressive affective disorders, including dysthymic disorder (depressive neurosis) and major depressive disorder. Maprotiline is effective at reducing symptoms of anxiety associated with depression. A bridged-ring tetracyclic antidepressant that is both mechanistically and functionally similar to the tricyclic antidepressants, including side effects associated with its use. Drug Indication For treatment of depression, including the depressed phase of bipolar depression, psychotic depression, and involutional melancholia, and may also be helpful in treating certain patients suffering severe depressive neurosis. Mechanism of Action Maprotiline exerts its antidepressant action by inhibition of presynaptic uptake of catecholamines, thereby increasing their concentration at the synaptic clefts of the brain. In single doses, the effect of maprotiline on the EEG revealed a rise in the alpha-wave density, a reduction of the alpha-wave frequency and an increase in the alpha-wave amplitude. However, as with other tricyclic antidepressants, maprotiline lowers the convulsive threshold. Maprotiline acts as an antagonist at central presynaptic α2-adrenergic inhibitory autoreceptors and hetero-receptors, an action that is postulated to result in an increase in central noradrenergic and serotonergic activity. Maprotiline is also a moderate peripheral α1 adrenergic antagonist, which may explain the occasional orthostatic hypotension reported in association with its use. Maprotiline also inhibits the amine transporter, delaying the reuptake of noradrenaline and norepinephrine. Lastly, maprotiline is a strong inhibitor of the histamine H1 receptor, which explains its sedative actions. Pharmacodynamics Maprotiline is a tetracyclic antidepressant. Although its main therapeutic use is in the treatment of depression, it has also been shown to exert a sedative effect on the anxiety component that often accompanies depression. In one sleep study, it was shown that maprotiline increases the duration of the REM sleep phase in depressed patients, compared to imipramine which reduced the REM sleep phase. Maprotiline is a strong inhibitor of noradrenaline reuptake in the brain and peripheral tissues, however it is worthy to note that it is a weak inhibitor of serotonergic uptake. In addition, it displays strong antihistaminic action (which may explain its sedative effects) as well as weak anticholinergic action. Maprotiline also has lower alpha adrenergic blocking activity than amitriptyline. |
| 分子式 |
C20H23N
|
|---|---|
| 分子量 |
277.40332
|
| 精确质量 |
277.183
|
| 元素分析 |
C, 86.59; H, 8.36; N, 5.05
|
| CAS号 |
10262-69-8
|
| 相关CAS号 |
Maprotiline hydrochloride;10347-81-6
|
| PubChem CID |
4011
|
| 外观&性状 |
Typically exists as solid at room temperature
|
| 密度 |
1.08 g/cm3
|
| 沸点 |
399.6ºC at 760 mmHg
|
| 闪点 |
187.7ºC
|
| 蒸汽压 |
1.35E-06mmHg at 25°C
|
| 折射率 |
1.599
|
| LogP |
4.602
|
| tPSA |
12.03
|
| 氢键供体(HBD)数目 |
1
|
| 氢键受体(HBA)数目 |
1
|
| 可旋转键数目(RBC) |
4
|
| 重原子数目 |
21
|
| 分子复杂度/Complexity |
339
|
| 定义原子立体中心数目 |
0
|
| SMILES |
CNCCCC12CCC(C3=CC=CC=C31)C4=CC=CC=C42
|
| InChi Key |
QSLMDECMDJKHMQ-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C20H23N/c1-21-14-6-12-20-13-11-15(16-7-2-4-9-18(16)20)17-8-3-5-10-19(17)20/h2-5,7-10,15,21H,6,11-14H2,1H3
|
| 化学名 |
N-methyl-3-(1-tetracyclo[6.6.2.02,7.09,14]hexadeca-2,4,6,9,11,13-hexaenyl)propan-1-amine
|
| 别名 |
maprotiline; 10262-69-8; Maprotylina [Polish]; Maprotylina; Maprotilinum [INN-Latin]; Maprotilina [INN-Spanish]; 9,10-Ethanoanthracene-9(10H)-propanamine, N-methyl-; 276-Ba;
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 3.6049 mL | 18.0245 mL | 36.0490 mL | |
| 5 mM | 0.7210 mL | 3.6049 mL | 7.2098 mL | |
| 10 mM | 0.3605 mL | 1.8025 mL | 3.6049 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。