| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 100mg |
|
||
| 500mg |
|
||
| Other Sizes |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Overall there are signs of systemic absorption via oral and dermal exposures, no evidence of target organs or of excretion. After oral ingestion and dermal absorption, the test substance will be metabolised to hippuric acid. Despite the low log Pow value, results of the 28-day study in rats and the predicted metabolism do not indicate a potential for the substance to bioaccumulate. After oral ingestion of benzoic acid and sodium benzoate, there is a rapid absorption (of undissociated benzoic acid) from the gastrointestinal tract in experimental animals or humans. ... 100% absorption can be assumed. In humans, the peak plasma concentration is reached within 1-2 hr. Hippuric acid is rapidly excreted in urine. In humans, after oral doses of up to 160 mg/kg body weight, 75-100% of the applied dose is excreted as hippuric acid within 6 hr after administration, and the rest within 2-3 days. Experiments on the distribution and elimination of (14)C-benzoate in the rat have shown no accumulation of sodium benzoate or benzoic acid in the body. For more Absorption, Distribution and Excretion (Complete) data for SODIUM BENZOATE (6 total), please visit the HSDB record page. Metabolism / Metabolites After oral and dermal uptake, benzoate is metabolized in the liver by conjugation with glycine, resulting in the formation of hippuric acid. The rate of biotransformation in humans is high: after oral doses of 40, 80 or 160 mg sodium benzoate/kg body weight, the transformation to hippuric acid was independent of the dose - about 17-29 mg/kg body weight per hour, corresponding to about 500 mg/kg body weight per day. Other /studies/ obtained higher values of 0.8-2 g/kg body weight per day. Another metabolite of benzoate is the benzoyl glucuronide. The metabolism of the benzoates depletes glycine concentrations and can therefore alter the glycine-dependent metabolism of other compounds. /A study/ demonstrated that ... sodium benzoate successfully competed with aspirin for glycine, resulting in increased concentration and persistence of salicyclic acid in the body. This study underlines the importance of cinnamon, a widely-used food spice and flavoring material, and its metabolite sodium benzoate (NaB), a widely-used food preservative and a FDA-approved drug against urea cycle disorders in humans, in increasing the levels of neurotrophic factors [e.g., brain-derived neurotrophic factor (BDNF) and neurotrophin-3 (NT-3)] in the CNS. NaB, but not sodium formate (NaFO), dose-dependently induced the expression of BDNF and NT-3 in primary human neurons and astrocytes. Interestingly, oral administration of ground cinnamon increased the level of NaB in serum and brain and upregulated the levels of these neurotrophic factors in vivo in mouse CNS. Accordingly, oral feeding of NaB, but not NaFO, also increased the level of these neurotrophic factors in vivo in the CNS of mice. NaB induced the activation of protein kinase A (PKA), but not protein kinase C (PKC), and H-89, an inhibitor of PKA, abrogated NaB-induced increase in neurotrophic factors. Furthermore, activation of cAMP response element binding (CREB) protein, but not NF-kappaB, by NaB, abrogation of NaB-induced expression of neurotrophic factors by siRNA knockdown of CREB and the recruitment of CREB and CREB-binding protein to the BDNF promoter by NaB suggest that NaB exerts its neurotrophic effect through the activation of CREB. Accordingly, cinnamon feeding also increased the activity of PKA and the level of phospho-CREB in vivo in the CNS. These results highlight a novel neutrophic property of cinnamon and its metabolite NaB via PKA - CREB pathway, which may be of benefit for various neurodegenerative disorders. |
|---|---|
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
IDENTIFICATION AND USE: Sodium benzoate is a colorless crystalline powder. It is used as food preservative, antiseptic, medicine, in tobacco, in pharmaceutical preparations, as an intermediate for manufacture of dyes, and as a rust and mildew inhibitor. HUMAN EXPOSURE AND TOXICITY: In a study with 2045 patients of dermatological clinics, only 5 persons (approximately 0.2%) showed a positive reaction in patch tests, while 34 of 5202 patients (approximately 0.7%) with contact urticaria reacted positively. Cases of urticaria, asthma, rhinitis, or anaphylactic shock have been reported following oral, dermal, or inhalation exposure to sodium benzoate. The symptoms appear shortly after exposure and disappear within a few hours. Chromosome aberration test was carried out on sodium benzoate using human embryonic lung culture cells. Sodium benzoate produced no significant increase in the aberration frequency in the anaphase chromosomes when tested at the dosage levels 0, 2.0 ug/mL, 20 ug/mL and 200 g/mL. In human embryonic lung cells (WI-38) treated with sodium benzoate both chromosome abnormalities and mitotic indices were within normal values. Sodium benzoate was mutagenic and cytotoxic in lymphocytes, where it caused micronucleus formation and chromosome break. ANIMAL STUDIES: An acute dermal irritation/corrosion study gave no indication for skin irritating effect in rabbits. Sodium benzoate was only slightly irritating to the eye. In a 90-day study with rats dosed with 0, 1, 2, 4, or 8% sodium benzoate via diet, the mortality in the highest dose group (approx. 6290 mg/kg body weight per day) was about 50%. Other effects in this group included a reduced weight gain, increased relative weights of liver and kidneys, and pathological changes in these organs. Sodium benzoate was given in drinking water to 50 female and 50 male mice from weeks 5 on for lifespan. The average daily intake of sodium benzoate was 119.2 mg for a female and 124.0 mg for a male (approx. 5.95 - 6.2 g/kg bw/d). There was no effect on the survival of the treated mice when compared with the untreated control. There were no significant differences between the tumor distribution in sodium benzoate-treated and untreated control mice. In a developmental study rats were injected intraperitoneally with 100, 315, or 1000 mg/kg sodium benzoate on gestation days 9 to 11 or 12 to 14. Reduced fetal body weight, increased in utero deaths (by 12%), and gross anomalies were noted at the highest dose. No evidence of teratogenicity was noted in rats administered 510 mg/kg of sodium benzoate by gavage on gestation days 9 to 11. Sodium benzoate (up to 3.0 mg/plate) was tested in the Salmonella/microsome test using S. typhimurium TA 92, TA 94, TA 98, TA 100, TA 1535 and TA 1537. No significant increases in the numbers of revertant colonies were detected in any S. typhimurium strains at the maximum dose. Sodium benzoate tested negative in a cytogenetic assay (bone marrow) in rats after single or multiple oral application of doses up to 5000 mg/kg body weight. In a study with mice, there was also no indication of mutagenic activity in a host-mediated assay. Interactions The GRAS report cited studies in which ingestion of sodium benzoate reduced the glycine-dependent formation of creatine, glutamine, urea, and uric acid and increased the effects of procaine, lidocaine, cocaine, tetracaine, and dibucaine. Under conditions of severely restricted fluid and salt intake, benzoates increased and prolonged the concentration of serum penicillin. The interaction between sodium benzoate (SB) and calf thymus DNA in simulated physiological buffer (pH 7.4) using acridine orange (AO) dye as a fluorescence probe, was investigated by UV-Vis absorption, fluorescence and circular dichroism (CD) spectroscopy along with DNA melting studies and viscosity measurements. An expanded UV-Vis spectral data matrix was resolved by multivariate curve resolution-alternating least squares (MCR-ALS) approach. The equilibrium concentration profiles and the pure spectra for SB, DNA and DNA-SB complex from the high overlapping composite response were simultaneously obtained. The results indicated that SB could bind to DNA, and hydrophobic interactions and hydrogen bonds played a vital role in the binding process. Moreover, SB was able to quench the fluorescence of DNA-AO complex through a static procedure. The quenching observed was indicative of an intercalative mode of interaction between SB and DNA, which was supported by melting studies, viscosity measurements and CD analysis. Non-Human Toxicity Values LC50 Rat inhalation >12,200 mg/cu m air/4 hr LD50 Rat oral 3450 mg/kg bw LD50 Rabbit oral 2000 mg/kg LD50 Mouse intramuscular 2306 mg/kg For more Non-Human Toxicity Values (Complete) data for SODIUM BENZOATE (8 total), please visit the HSDB record page. |
| 参考文献 | |
| 其他信息 |
Therapeutic Uses
Antifungal Agents; Food Preservatives Sodium phenylacetate and sodium benzoate is used as adjunctive therapy for the treatment of acute hyperammonemia and associated encephalopathy in patients with disorders (i.e., deficiencies in enzymes) of the urea cycle. Sodium phenylacetate and sodium benzoate is designated an orphan drug by the US Food and Drug Administration (FDA) for this use. /EXPL THER/ In addition to dopaminergic hyperactivity, hypofunction of the N-methyl-d-aspartate receptor (NMDAR) has an important role in the pathophysiology of schizophrenia. Enhancing NMDAR-mediated neurotransmission is considered a novel treatment approach. To date, several trials on adjuvant NMDA-enhancing agents have revealed beneficial, but limited, efficacy for positive and negative symptoms and cognition. Another method to enhance NMDA function is to raise the levels of d-amino acids by blocking their metabolism. Sodium benzoate is a d-amino acid oxidase inhibitor. /The objective of this study was/ to examine the clinical and cognitive efficacy and safety of add-on treatment of sodium benzoate for schizophrenia. /The study consisted of/ a randomized, double-blind, placebo-controlled trial in 2 major medical centers in Taiwan composed of 52 patients with chronic schizophrenia who had been stabilized with antipsychotic medications for 3 months or longer. /Interventions included/ six weeks of add-on treatment of 1 g/d of sodium benzoate or placebo. The primary outcome measure was the Positive and Negative Syndrome Scale (PANSS) total score. Clinical efficacy and adverse effects were assessed biweekly. Cognitive functions were measured before and after the add-on treatment. Benzoate produced a 21% improvement in PANSS total score and large effect sizes (range, 1.16-1.69) in the PANSS total and subscales, Scales for the Assessment of Negative Symptoms-20 items, Global Assessment of Function, Quality of Life Scale and Clinical Global Impression and improvement in the neurocognition subtests as recommended by the National Institute of Mental Health's Measurement and Treatment Research to Improve Cognition in Schizophrenia initiative, including the domains of processing speed and visual learning. Benzoate was well tolerated without significant adverse effects. Benzoate adjunctive therapy significantly improved a variety of symptom domains and neurocognition in patients with chronic schizophrenia. The preliminary results show promise for d-amino acid oxidase inhibition as a novel approach for new drug development for schizophrenia. /EXPL THER/ N-methyl-D-aspartate receptor (NMDAR)-mediated neurotransmission is vital for learning and memory. Hypofunction of NMDAR has been reported to play a role in the pathophysiology of Alzheimer disease (AD), particularly in the early phase. Enhancing NMDAR activation might be a novel treatment approach. One of the methods to enhance NMDAR activity is to raise the levels of NMDA coagonists by blocking their metabolism. This study examined the efficacy and safety of sodium benzoate, a D-amino acid oxidase inhibitor, for the treatment of amnestic mild cognitive impairment and mild AD. We conducted a randomized, double-blind, placebo-controlled trial in four major medical centers in Taiwan. Sixty patients with amnestic mild cognitive impairment or mild AD were treated with 250-750 mg/day of sodium benzoate or placebo for 24 weeks. Alzheimer's Disease Assessment Scale-cognitive subscale (the primary outcome) and global function (assessed by Clinician Interview Based Impression of Change plus Caregiver Input) were measured every 8 weeks. Additional cognition composite was measured at baseline and endpoint. Sodium benzoate produced a better improvement than placebo in Alzheimer's Disease Assessment Scale-cognitive subscale (p = .0021, .0116, and .0031 at week 16, week 24, and endpoint, respectively), additional cognition composite (p = .007 at endpoint) and Clinician Interview Based Impression of Change plus Caregiver Input (p = .015, .016, and .012 at week 16, week 24, and endpoint, respectively). Sodium benzoate was well-tolerated without evident side-effects. Sodium benzoate substantially improved cognitive and overall functions in patients with early-phase AD. The preliminary results show promise for D-amino acid oxidase inhibition as a novel approach for early dementing processes. /EXPL THER/ A recent clinical study demonstrated that sodium benzoate (SB), a prototype competitive d-amino acid oxidase inhibitor, was effective in the treatment of several symptoms, such as positive and negative symptoms, and cognitive impairment in medicated patients with schizophrenia. The objective of the study was to examine the effects of SB on behavioral abnormalities such as pre-pulse inhibition (PPI) deficits and hyperlocomotion in mice after a single administration of the N-methyl-D-aspartate (NMDA) receptor antagonist, phencyclidine (PCP). The effects of SB on behavioral abnormalities (PPI deficits and hyperlocomotion) in mice after PCP administration were examined. Furthermore, effects of SB on tissue levels of amino acids were also examined. A single oral dose of SB (100, 300, or 1000 mg/kg) attenuated PPI deficits in mice after administration of PCP (3.0 mg/kg, s.c.) in a dose-dependent manner. In contrast, L-701,324 (10 mg/kg), an antagonist at the glycine site of the NMDA receptor, did not affect the effect of SB (1000 mg/kg) on PCP-induced PPI deficits. Furthermore, a single oral dose of SB (1000 mg/kg) significantly attenuated the hyperlocomotion in mice after administration of PCP (3.0 mg/kg, s.c.). However, a single oral dose of SB (1000 mg/kg) caused no changes to D-serine levels in plasma or in the frontal cortex, hippocampus, and striatum of these animals. This study suggests that SB induced antipsychotic effects in the PCP model of schizophrenia, although it did not increase D-serine levels in the brain. Drug Warnings At /the therapeutic/ dose level, clinical signs of toxicity are rare and in most cases limited to anorexia and vomiting, especially after intravenous bolus infusions. |
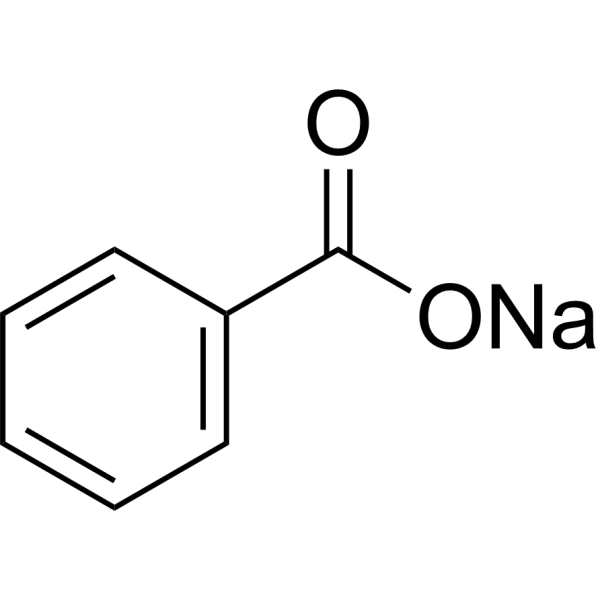
| 分子式 |
C7H5NAO2
|
|---|---|
| 分子量 |
144.10
|
| 精确质量 |
144.018
|
| CAS号 |
532-32-1
|
| 相关CAS号 |
Benzoate-d5 sodium;62790-26-5
|
| PubChem CID |
517055
|
| 外观&性状 |
White to off-white solid powder
|
| 密度 |
1,44 g/cm3
|
| 沸点 |
249.3ºC at 760 mmHg
|
| 熔点 |
>300 °C(lit.)
|
| 闪点 |
111.4ºC
|
| LogP |
0.05
|
| tPSA |
40.13
|
| 氢键供体(HBD)数目 |
0
|
| 氢键受体(HBA)数目 |
2
|
| 可旋转键数目(RBC) |
1
|
| 重原子数目 |
10
|
| 分子复杂度/Complexity |
108
|
| 定义原子立体中心数目 |
0
|
| InChi Key |
WXMKPNITSTVMEF-UHFFFAOYSA-M
|
| InChi Code |
InChI=1S/C7H6O2.Na/c8-7(9)6-4-2-1-3-5-6;/h1-5H,(H,8,9);/q;+1/p-1
|
| 化学名 |
sodium;benzoate
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO: 5 mg/mL (34.70 mM)
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 6.9396 mL | 34.6981 mL | 69.3963 mL | |
| 5 mM | 1.3879 mL | 6.9396 mL | 13.8793 mL | |
| 10 mM | 0.6940 mL | 3.4698 mL | 6.9396 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。