| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 1mg |
|
||
| Other Sizes |
|
| 靶点 |
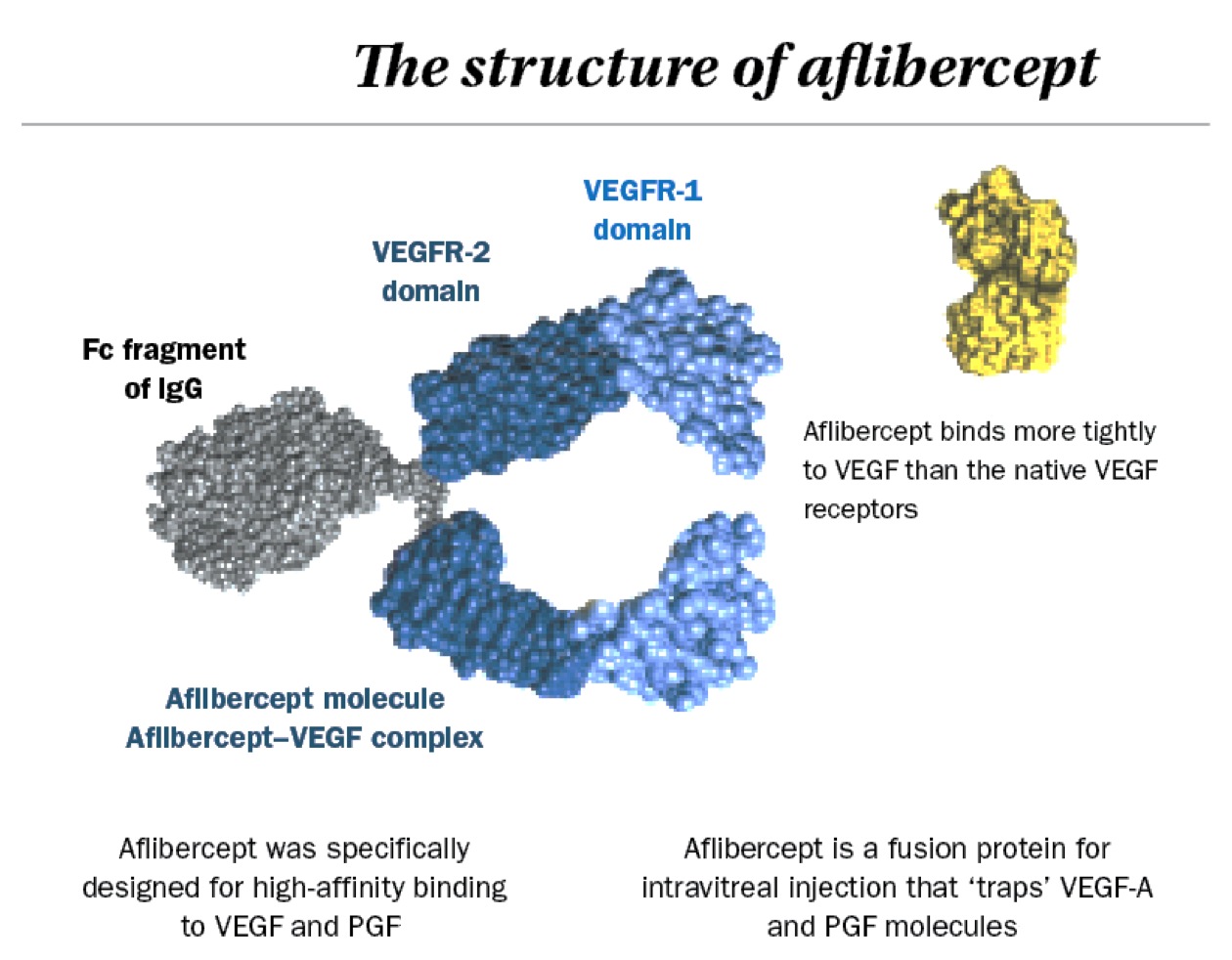
Aflibercept inhibits vascular endothelial growth factor (VEGF) signaling by acting as a soluble decoy receptor for VEGF-A, VEGF-B, and placental growth factor (PlGF) [1]
|
|---|---|
| 体外研究 (In Vitro) |
在台盼蓝排除实验或 MTT 测定中,阿柏西普(500 μg/mL;24 小时和 7 d)对 RPE 细胞均未表现出任何毒性[1]。在具有三个伤口的汇合 RPE 细胞层中,与对照相比,阿柏西普(500 μg/mL;24 小时)对伤口愈合表现出统计学上显着的影响[1]。与未处理的对照相比,阿柏西普(500 μg/mL;7 d)表现出对调理乳胶珠的吞噬作用明显降低[1]。阿柏西普(1 和 10 μg/mL;10 小时)可降低血管生成和通透性(这两个 VEGF 调节过程),进而抑制 VEGF 信号传导[2]。
Aflibercept (500 µg/mL) 对原代猪RPE细胞无细胞毒性:MTT实验中细胞存活率为97.8±3.0%(24小时)和102.4±0.9%(7天);台盼蓝排除实验中为97.9±7.3%(24小时)和97.2±17.4%(7天)。[1] 临床相关浓度(500 µg/mL)下,Aflibercept 显著抑制RPE伤口愈合(划痕实验),伤口闭合率降至70.3±10.3%(对照组87.3±8.4%,p<0.01)。125 µg/mL时无影响(72.2±6.1% vs. 对照组74.2±5.5%)。[1] Aflibercept (500 µg/mL) 降低RPE细胞对调理化乳胶珠的吞噬能力(28.3±2.9 珠/细胞 vs. 对照组42.8±4.3 珠/细胞,p<0.001),效果与贝伐单抗相当(30.2±5.2 珠/细胞)。[1] Aflibercept (1–10 µg/mL) 降低rVEGF-A诱导的人脐静脉内皮细胞(HUVECs)通透性18.8–27.1%(p<0.01–0.0001),经FITC-葡聚糖跨孔实验测定。管腔形成呈剂量依赖性抑制,证实抗血管生成活性。[2] 在原代猪RPE细胞中,Aflibercept (500 µg/mL) 损害伤口愈合(闭合率70.3±10.3% vs. 对照组87.3±8.4%,p<0.01),并降低对调理化珠粒的吞噬能力(28.3±2.9 珠/细胞 vs. 对照组42.8±4.3,p<0.001)。[2] HUVECs经Aflibercept(50 nM,24小时)处理后,细胞内NO水平显著降低(DAF-FM荧光检测),ROS积累增加(DHE染色显示),与NOX1/NOX4蛋白表达上调相关[3] Western blot分析表明,Aflibercept(50 nM,24小时)降低Akt(Ser473)和eNOS(Ser1177)磷酸化,抑制CAT-1转运蛋白表达,并减少细胞内L-精氨酸浓度[3] |
| 体内研究 (In Vivo) |
在肥胖小鼠中,阿柏西普(10 mg/kg;大脑中动脉闭塞后 3 小时;MCAO))通过减少中风诱导的 VEGF-A 和 VEGFR2 表达、脑水肿和 BBB 破坏来增加中风后存活率 [2]。阿柏西普(18.2 mg/kg 和 36.4 mg/kg;腹腔注射一次)影响小鼠的血压、ROS 的产生和 eNOS[3]。
在饮食诱导的肥胖卒中小鼠中,Aflibercept (10 mg/kg 静脉注射,大脑中动脉闭塞(MCAO)后3h单次给药) 降低死亡率(17% vs. IgG对照组40%)、出血性转化(27% vs. 43%)和脑水肿(18% vs. 28%,p<0.01)。血脑屏障破坏(IgG/葡聚糖外渗)显著减弱(p<0.05)。[2] 神经行为评分在卒中后1/3天改善(p<0.05)。在非肥胖恶性梗死小鼠中无获益,证实疗效具共病选择性。[2] C57BL/6小鼠单次静脉注射Aflibercept(18.2或36.4 mg/kg)诱发急性剂量依赖性高血压(收缩压峰值出现在第2天),损害乙酰胆碱介导的内皮依赖性舒张(EDR),并降低主动脉NO生物利用度[3] 长期给药(14天内5次注射)导致持续高血压,增加主动脉ET-1水平,升高ROS(通过NOX1/NOX4介导),并持续抑制p-Akt/p-eNOS信号及CAT-1表达[3] |
| 细胞实验 |
伤口愈合(划痕实验): 融合的原代猪RPE细胞用牙签划伤创口,洗涤后加入含Aflibercept (125 µg/mL或500 µg/mL)的无酚红DMEM(含10% FBS)。24小时后通过显微镜定量伤口闭合率(AxioVision软件)。[1]
吞噬功能实验: RPE细胞经Aflibercept (500 µg/mL)处理7天后,与猪光感受器外节调理化的FITC标记乳胶珠共孵育4小时。通过荧光显微镜计数每个细胞的内化珠粒量化吞噬能力。[1] 细胞摄取: RPE细胞经Aflibercept (125 µg/mL或500 µg/mL)处理1小时至7天后,固定、透化,并用山羊抗人AlexaFluor555抗体染色。荧光显微镜显示囊泡状摄取(≥82.5%细胞阳性),持续7天。[1] |
| 动物实验 |
Animal/Disease Models: Male C57BL/6 mice[3]
Doses: 18.2 mg/kg and 36.4 mg/kg Route of Administration: intravenous (iv) injection; 18.2 mg/kg and 36.4 mg/kg once Experimental Results: Rapidly and dose-dependently elevated BP in mice and markedly impaired endothelial-dependent relaxation (EDR) and resulted in NADPH oxidases 1 (NOX1)- and NADPH oxidases 4 (NOX4 )-mediated generation of ROS, diminished the activation of protein kinase B (Akt) and endothelial nitric oxide synthase (eNOS) concurrently with a reduction in nitric oxide (NO) production and elevation of ET-1 levels in mouse aortas. Obese C57BL/6 mice (HFD for 8–12 weeks) underwent 30-min transient MCAO. Aflibercept (10 mg/kg) or IgG control was administered intravenously 3h post-occlusion. Outcomes (infarct volume, swelling, BBB integrity) were assessed at 72h.[2] For severe stroke in lean mice: 40-min MCAO followed by identical Aflibercept dosing (10 mg/kg IV, 3h post-occlusion).[2] Male C57BL/6 mice (8–10 weeks) received intravenous Aflibercept (18.2 or 36.4 mg/kg) as a single dose (short-term) or five doses at 2-day intervals (long-term). Doses were calculated based on human-to-mouse conversion (human equivalent: 4 mg/kg)[3] For L-arg co-administration studies, mice were pretreated orally with L-arg (0.5 or 1.0 g/kg, twice daily) 3 days before Aflibercept injection and continued until endpoint[3] |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Following intravitreal injection of aflibercept (2 mg in each eye) in patients with neovascular (wet) age-related macular degeneration, mean peak plasma concentration of free aflibercept was attained in 1-3 days; this concentration is estimated to be more than 100-fold lower than the concentration of aflibercept required to half-maximally bind systemic VEGF. Concentrations of free aflibercept in plasma were undetectable 2 weeks after intravitreal injection. No accumulation of aflibercept in plasma was observed following repeated intravitreal injections (i.e., once every 4 weeks). Absorption Following unilateral intravitreal administration of 8 mg aflibercept, the mean (SD) Cmax of free aflibercept in plasma was 0.30 (0.27) mg/L, and the median time to maximal concentration in plasma was 2.9 days. The accumulation of free aflibercept in plasma following three initial monthly intravitreal doses was minimal (mean accumulation ratio 1.2); subsequently, no further accumulation was observed. In patients with wet age-related macular degeneration (AMD), retinopathy of prematurity (RVO), and diabetic macular edema (DME), the mean Cmaxof free aflibercept in the plasma was 0.02 mcg/mL (range: 0 to 0.054 mcg/mL), 0.05 mcg/mL (range: 0 to 0.081 mcg/mL), and 0.03 mcg/mL (range: 0 to 0.076 mcg/mL), respectively and was attained in 1 to 3 days following intravitreal administration of 2 mg per eye. The free aflibercept plasma concentrations were undetectable two weeks post-dosing in all patients. Volume of Distribution The volume of distribution of free aflibercept following intravenous (I.V.) administration of aflibercept is approximately 7 L. Clearance Following an hour of intravenous infusion of 2 to 9 mg/kg every 2 or 3 week in cancer patients, the clearances of free and bound aflibercept were estimated to be 0.88 L/day and 0.14 L/day respectively. Healthy subjects have a similar clearance of free aflibercept but slightly faster clearance of bound aflibercept (0.19 L/day). Patients with a low albumin or high alkaline phosphatase levels also typically exhibit faster clearance of free aflibercept. Metabolism / Metabolites Aflibercept is a therapeutic protein and no drug metabolism studies have been conducted. Aflibercept is expected to undergo elimination through both target-mediated disposition via binding to free endogenous VEGF and metabolism via proteolysis. Biological Half-Life For the intravitreal formulation, the half-life was estimated to be 7.13 days. For the intravenous formulation, following a dose of 4 mg per kg every two weeks administered intravenously, the elimination half-life of free ziv-aflibercept was approximately 6 days (range 4-7 days). |
| 毒性/毒理 (Toxicokinetics/TK) |
Single IV dose (10 mg/kg) caused no hypertension or leukopenia in mice. Hemorrhagic transformation was reduced (27% vs. 43% in controls), indicating no bleeding risk exacerbation.[2]
In RPE cells, 500 µg/mL Aflibercept showed no cytotoxicity (cell viability >97% at 24h/7d in MTT/trypan blue assays).[1] Aflibercept induced hypertension in 42.4% of patients and hypertensive crisis in 17.4% (clinical data). In mice, it caused vascular dysfunction via eNOS/NO signaling suppression, ROS overproduction, and ET-1 elevation[3] Toxicity Summary IDENTIFICATION AND USE: Aflibercept intravitreal injection is used for the treatment of neovascular (wet) age-related macular degeneration. HUMAN EXPOSURE AND TOXICITY: At worse levels of initial visual acuity, aflibercept was more effective at improving vision. Progression-free survival for patients receiving ziv-aflibercept was higher compared with placebo. The most common adverse effects observed were anemia, diarrhea, and neutropenia. Ziv-aflibercept is a safe and effective option in combination with FOLFIRI for the treatment of metastatic colorectal cancer in patients who progress on oxaliplatin-containing therapy. Superiority over other antiangiogenic treatment has not been established. Aflibercept is a valuable treatment alternative in patients previously treated with bevacizumab and/or ranibizumab injections. Stability of visual acuity and anatomic improvement on spectral-domain optical coherence tomography were observed after initiation of aflibercept treatment in those previously treated with ranibizumab and/or bevacizumab injections every 4-6 weeks. The mean change in visual acuity (defined as the number of letters of visual acuity gained or lost compared with baseline) at 52 weeks was a gain of 7.9-8.9, 7.6-10.9, or 8.1-9.4 letters in patients receiving aflibercept 2 mg every 8 weeks, aflibercept 2 mg every 4 weeks, or ranibizumab 0.5 mg every 4 weeks, respectively. ANIMAL STUDIES: Erosions and ulcerations of the respiratory epithelium in nasal turbinates in monkeys treated with aflibercept intravitreally were observed at intravitreal doses of 2 or 4 mg per eye. Intravenous administration of the lowest dose of aflibercept assessed in monkeys (3 mg per kg) resulted in systemic exposure (AUC) that was approximately 1500 times higher than the systemic exposure observed in humans after an intravitreal dose of 2 mg. All changes were reversible within 20 weeks after cessation of treatment. Aflibercept produced fetal malformations at all doses assessed in rabbits. Administration of the lowest dose assessed in rabbits (0.1 mg per kg) resulted in systemic exposure (AUC) that was approximately 10 times the systemic exposure observed in humans after an intravitreal dose of 2 mg. Aflibercept is intended for intravitreal administration to exert local effects in the eye. IVI allows the medication to penetrate all retinal layers, minimizing systemic effects. No cytotoxic effects have been observed in studies that exposed cultured corneal endothelial cells to varying concentrations of aflibercept. However, there has been an interest in the potential for drug overdose with intravitreal aflibercept therapy due to a slight misalignment of the plunger in prefilled syringes. These small mismeasurements can lead to delivering double the intended volume of medication. In part, aflibercept overdose accounts for a number of intraocular pressure elevations since its launch. Unfortunately, there is no known antidote for aflibercept overdose. Proper adherence to instructions for use can minimize dosing errors and prevent toxicity of intravitreal aflibercept. Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation This record refers to the use of intravitreal aflibercept. Aflibercept inhibits vascular endothelial growth factor (VEGF). Aflibercept is a large protein molecule with a molecular weight of 115,000, absorption is unlikely because it is probably partly destroyed in the infant's gastrointestinal tract and poorly absorbed orally, so systemic effects in infants are not expected. Aflibercept appeared in breastmilk in small amounts in only one of four days after intravitreal injection in one mother. Aflibercept is approved for intravitreal injection in preterm infants with retinopathy of prematurity. The risk to the nursing infant appears to be very low. Since VEGF is present in human milk and is thought to help in maturation of the infant’s gastrointestinal tract, concern has been raised about the maternal use of VEGF inhibitors during breastfeeding. However, the typical alternative to breastmilk is infant formula, which contains no VEGF. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk A woman with diabetic macular edema was given intravitreal aflibercept 2 mg one week postpartum. She was not breastfeeding her infant. Milk samples were obtained before the injection and on days 1 to 4 after the injection. VEGF levels were reduced from 10.6 mcg/L at baseline to 4.9 mcg/L on day 1, where it remained for the next 3 days. Adverse Effects Adverse effects associated with aflibercept use include eye irritation, vitreous detachment, temporary blurred vision, eyelid swelling, and conjunctival hemorrhage. Serious adverse reactions related to the administration of aflibercept and the injection procedure include retinal detachment, traumatic cataracts, thromboembolic events, and increased intraocular pressure (IOP). These complications are observed in less than 0.1% of intravitreal injections with aflibercept. A temporary rise in intraocular pressure within 60 minutes of administration can be expected and should return to baseline in minutes following injection. Intraocular pressure may take longer to normalize in patients with glaucoma and other ocular comorbidities. Patients should be educated about common and severe adverse effects and know when to notify their doctor. Human Toxicity Excerpts /HUMAN EXPOSURE STUDIES/ The relative efficacy and safety of intravitreous aflibercept, bevacizumab, and ranibizumab in the treatment of diabetic macular edema are unknown. METHODS: At 89 clinical sites, we randomly assigned 660 adults (mean age, 61+/-10 years) with diabetic macular edema involving the macular center to receive intravitreous aflibercept at a dose of 2.0 mg (224 participants), bevacizumab at a dose of 1.25 mg (218 participants), or ranibizumab at a dose of 0.3 mg (218 participants). The study drugs were administered as often as every 4 weeks, according to a protocol-specified algorithm. The primary outcome was the mean change in visual acuity at 1 year. RESULTS: From baseline to 1 year, the mean visual-acuity letter score (range, 0 to 100, with higher scores indicating better visual acuity; a score of 85 is approximately 20/20) improved by 13.3 with aflibercept, by 9.7 with bevacizumab, and by 11.2 with ranibizumab. Although the improvement was greater with aflibercept than with the other two drugs (P<0.001 for aflibercept vs. bevacizumab and P=0.03 for aflibercept vs. ranibizumab), it was not clinically meaningful, because the difference was driven by the eyes with worse visual acuity at baseline (P<0.001 for interaction). When the initial visual-acuity letter score was 78 to 69 (equivalent to approximately 20/32 to 20/40) (51% of participants), the mean improvement was 8.0 with aflibercept, 7.5 with bevacizumab, and 8.3 with ranibizumab (P>0.50 for each pairwise comparison). When the initial letter score was less than 69 (approximately 20/50 or worse), the mean improvement was 18.9 with aflibercept, 11.8 with bevacizumab, and 14.2 with ranibizumab (P<0.001 for aflibercept vs. bevacizumab, P=0.003 for aflibercept vs. ranibizumab, and P=0.21 for ranibizumab vs. bevacizumab). There were no significant differences among the study groups in the rates of serious adverse events (P=0.40), hospitalization (P=0.51), death (P=0.72), or major cardiovascular events (P=0.56). CONCLUSIONS: Intravitreous aflibercept, bevacizumab, or ranibizumab improved vision in eyes with center-involved diabetic macular edema, but the relative effect depended on baseline visual acuity. When the initial visual-acuity loss was mild, there were no apparent differences, on average, among study groups. At worse levels of initial visual acuity, aflibercept was more effective at improving vision. PMID:25692915 /HUMAN EXPOSURE STUDIES/ Review pharmacology, pharmacokinetics, efficacy, and safety of ziv-aflibercept in combination with FOLFIRI for treatment of metastatic colorectal cancer (mCRC) resistant to or progressed following oxaliplatin-containing regimens.... Ziv-aflibercept, a selective vascular endothelial growth factor antagonist, was evaluated as monotherapy for treatment of mCRC in a phase 2 study and added to FOLFIRI in a phase 3 trial. Patient response to ziv-aflibercept as monotherapy did not reach statistical significance. Results suggest that response to ziv-aflibercept treatment is not influenced by prior bevacizumab therapy. A phase 3 trial compared the safety and efficacy of ziv-aflibercept plus FOLFIRI with placebo plus FOLFIRI in patients with mCRC who experienced disease progression on an oxaliplatin-containing regimen. Patients in the ziv-aflibercept arm had a median overall survival of 13.5 months, versus 12.06 months for those receiving placebo (hazard ratio [HR] = 0.817, 95% CI = 0.713 to 0.937). Progression-free survival for patients receiving ziv-aflibercept was higher compared with placebo (HR = 0.758; 95% CI = 0.661 to 0.869). The most common adverse effects observed were anemia, diarrhea, and neutropenia. Ziv-aflibercept is a safe and effective option in combination with FOLFIRI for the treatment of mCRC in patients who progress on oxaliplatin-containing therapy. Superiority over other antiangiogenic treatment has not been established. PMID:24259608 /HUMAN EXPOSURE STUDIES/ Intravitreal aflibercept, a fusion protein with high affinity for vascular endothelial growth factor, offers an alternative treatment for exudative age-related macular degeneration. Preclinical studies and early and late phase clinical trials suggest that aflibercept's high binding affinity may impart greater durability of activity and increased efficacy compared to ranibizumab or bevacizumab. A total of 266 eyes of 249 patients with exudative age-related macular degeneration who received aflibercept after treatment with bevacizumab and/or ranibizumab were included in a retrospective review. Mean central subfoveal thickness on spectral-domain optical coherence tomography and mean logarithm of the minimal angle of resolution (logMAR) visual acuity were calculated at 1, 3, 6, and 12 months after the first aflibercept injection. Subgroup analyses were performed in eyes receiving at least 5 bevacizumab and/or ranibizumab injections in the 6 months prior to aflibercept and in eyes receiving at least 10 injections in the 12 months prior to aflibercept. Eyes received an average of 14.7 (range 1-43) ranibizumab and/or bevacizumab treatments prior to initiation of aflibercept therapy. The mean central subfoveal thickness decreased from 300 to 275 um at 1 month (p<0.001) and was maintained at 6 months. Mean logMAR visual acuity improved from 0.60 (Snellen equivalent 20/80) to 0.54 (20/70, p = 0.01) at 1 month and was stable at 0.55 at 6 months (Snellen equivalent 20/70, p = 0.11, n = 251). In 82 eyes receiving at least 5 injections in the 6 months prior to aflibercept treatment (average of 18.1 injections total), the central subfoveal thickness improved from 296 to 279 um at 1 month (p<0.0001) and was maintained at 6 months (p<0.0001). Visual acuity did not change (0.48 [20/61] at 1 month compared to baseline, 0.49 [20/62], p = 0.634, and at 6 months 0.51 [20/65], p = 0.601). In 50 eyes receiving at least 10 injections in the 12 months prior to aflibercept treatment (average of 21.8 injections total), the mean central subfoveal thickness decreased by 17 um at 1 month (p = 0.0007) and was maintained at 6 months (p = 0.013). Again, visual acuity did not change (0.46 [20/56] at 1 month, baseline 0.44 [20/56], p = 0.547, and 0.50 [20/63] at 6 months, p = 0.2445). Aflibercept is a valuable treatment alternative in patients previously treated with bevacizumab and/or ranibizumab injections. Stability of visual acuity and anatomic improvement on spectral-domain optical coherence tomography were observed after initiation of aflibercept treatment in those preciously treated with ranibizumab and/or bevacizumab injections every 4-6 weeks. PMID:24706352 /HUMAN EXPOSURE STUDIES/ To assess for change in intraocular pressure (IOP) in neovascular age-related macular degeneration patients switched to aflibercept after receiving previous treatments of intravitreal bevacizumab or ranibizumab. This is a retrospective chart review of the first 53 patients (53 eyes) treated with at least 2 injections of 2 mg in 0.05 mL of aflibercept by March 6, 2013, after at least 2 previous injections of 0.5 mg in 0.05 mL of ranibizumab with or without previous injections of 1.25 mg in 0.05 mL of bevacizumab. The analysis was restricted to the first such sequence within each patient. The last previous anti-vascular endothelial growth factor injection before the switch to aflibercept was ranibizumab in all cases included in the study. Each person served as his or her own control. The pre-aflibercept IOP in the before state (treatment with bevacizumab or ranibizumab) was the preinjection IOP measure before dilation at the visit of the first aflibercept injection. Statistical analysis was performed using Microsoft Excel. There were 41 patients who were first treated with ranibizumab followed by aflibercept and 12 patients treated with ranibizumab and bevacizumab followed by aflibercept. For each of these sequences, IOP in the treated eye during treatment with aflibercept (the after state) was computed in 3 different ways: the first IOP, the last IOP, and the mean IOP for the period when treated with aflibercept. The pooled data showed a mean pre-aflibercept (the before state) IOP of 14.87 that decreased to a mean first IOP of 14.57, mean last IOP of 13.79, and a mean IOP of 14.14 during aflibercept treatment. The inference is based on the pooled analysis. The 95% confidence interval for the differences (after minus before) were -0.30 (-1.12 to 0.52), -1.08 (-1.83 to -0.32), and -0.73 (-1.30 to -0.17) for the first, last, and mean IOPs, respectively. The corresponding P values were 0.46 for the first, 0.006 for the last, 0.01 for the mean IOP during the aflibercept treatment period. Intraocular pressure was found to be significantly lower in patients switched to aflibercept after previous treatments with ranibizumab and/or bevacizumab. Aflibercept may have a more favorable IOP safety profile in patients previously on other anti-vascular endothelial growth factor treatments. PMID:25072648 Non-Human Toxicity Excerpts /LABORATORY ANIMALS: Acute Exposure/ Erosions and ulcerations of the respiratory epithelium in nasal turbinates in monkeys treated with aflibercept intravitreally were observed at intravitreal doses of 2 or 4 mg per eye. At the NOAEL of 0.5 mg per eye in monkeys, the systemic exposure (AUC) was 56 times higher than the exposure observed in humans after an intravitreal dose of 2 mg. /LABORATORY ANIMALS: Developmental or Reproductive Toxicity/ Effects on male and female fertility were assessed as part of a 6-month study in monkeys with intravenous administration of aflibercept at weekly doses ranging from 3 to 30 mg per kg. Absent or irregular menses associated with alterations in female reproductive hormone levels and changes in sperm morphology and motility were observed at all dose levels. In addition, females showed decreased ovarian and uterine weight accompanied by compromised luteal development and reduction of maturing follicles. These changes correlated with uterine and vaginal atrophy. A No Observed Adverse Effect Level (NOAEL) was not identified. Intravenous administration of the lowest dose of aflibercept assessed in monkeys (3 mg per kg) resulted in systemic exposure (AUC) that was approximately 1500 times higher than the systemic exposure observed in humans after an intravitreal dose of 2 mg. All changes were reversible within 20 weeks after cessation of treatment. /LABORATORY ANIMALS: Developmental or Reproductive Toxicity/ Aflibercept produced embryo-fetal toxicity when administered every three days during organogenesis to pregnant rabbits at intravenous doses >/= 3 mg per kg, or every six days at subcutaneous doses >/= 0.1 mg per kg. Adverse embryo-fetal effects included increased incidences of postimplantation loss and fetal malformations, including anasarca, umbilical hernia, diaphragmatic hernia, gastroschisis, cleft palate, ectrodactyly, intestinal atresia, spina bifida, encephalomeningocele, heart and major vessel defects, and skeletal malformations (fused vertebrae, sternebrae, and ribs; supernumerary vertebral arches and ribs; and incomplete ossification). The maternal No Observed Adverse Effect Level (NOAEL) in these studies was 3 mg per kg. Aflibercept produced fetal malformations at all doses assessed in rabbits and the fetal NOAEL was less than 0.1 mg per kg. Administration of the lowest dose assessed in rabbits (0.1 mg per kg) resulted in systemic exposure (AUC) that was approximately 10 times the systemic exposure observed in humans after an intravitreal dose of 2 mg. |
| 参考文献 |
|
| 其他信息 |
Aflibercept is internalized by RPE cells within 1 h and retained intracellularly for ≥7 days in vesicular and net-like structures. This uptake correlates with reduced phagocytic function, independent of VEGF inhibition.[1]
The impairment of RPE wound healing and phagocytosis by Aflibercept at clinical concentrations (500 µg/mL) suggests potential side effects in long-term therapy, including delayed retinal repair and photoreceptor degeneration.[1] Aflibercept is internalized by RPE cells (vesicular/net-like patterns) and retained for ≥7 days, correlating with phagocytosis impairment. In obese stroke, it downregulates ipsilateral VEGF-A/VEGFR2/NRP-1 expression (p<0.05).[2] FDA-approved for ocular neovascular diseases; repurposing potential for obesity-exacerbated stroke edema due to selective reduction of vascular permeability without infarct modification.[2] Aflibercept is a fusion protein comprising Ig domains of VEGFR1/R2 and Fc region of human IgG1, used as first-line monotherapy for cancers. It inhibits VEGF/PlGF-driven angiogenesis but triggers hypertension via CAT-1/AKT/eNOS/NO pathway disruption[3] Mechanistically, it reduces NO bioavailability, increases ET-1 and oxidative stress (NOX1/NOX4-mediated), and downregulates cationic amino acid transporter CAT-1[3] Drug Indication The opthalmic agent is used for the treatment of neovascular (Wet) age-related macular degeneration (AMD), macular edema following retinal vein occlusion (RVO), diabetic macular edema (DME), diabetic retinopathy (DR), and retinopathy of prematurity (ROP). The systemic injection, known as ziv-aflibercept, in combination with 5-fluorouracil, leucovorin, irinotecan-(FOLFIRI), is for the treatment of metastatic colorectal cancer that is resistant to or progressed following treatment with oxaliplatin. Yesafili is indicated for adults for the treatment ofneovascular (wet) age-related macular degeneration (AMD) (see section 5. 1),visual impairment due to macular oedema secondary to retinal vein occlusion (branch RVO or central RVO) (see section 5. 1),visual impairment due to diabetic macular oedema (DME) (see section 5. 1),visual impairment due to myopic choroidal neovascularisation (myopic CNV) (see section 5. 1). Eylea is indicated for adults for the treatment of: neovascular (wet) age-related macular degeneration (AMD); visual impairment due to macular oedema secondary to retinal vein occlusion (branch RVO or central RVO); visual impairment due to diabetic macular oedema (DME); visual impairment due to myopic choroidal neovascularisation (myopic CNV). Therapeutic Uses Review pharmacology, pharmacokinetics, efficacy, and safety of ziv-aflibercept in combination with FOLFIRI for treatment of metastatic colorectal cancer (mCRC) resistant to or progressed following oxaliplatin-containing regimens.... Ziv-aflibercept, a selective vascular endothelial growth factor antagonist, was evaluated as monotherapy for treatment of mCRC in a phase 2 study and added to FOLFIRI in a phase 3 trial. Patient response to ziv-aflibercept as monotherapy did not reach statistical significance. Results suggest that response to ziv-aflibercept treatment is not influenced by prior bevacizumab therapy. A phase 3 trial compared the safety and efficacy of ziv-aflibercept plus FOLFIRI with placebo plus FOLFIRI in patients with mCRC who experienced disease progression on an oxaliplatin-containing regimen. Patients in the ziv-aflibercept arm had a median overall survival of 13.5 months, versus 12.06 months for those receiving placebo (hazard ratio [HR] = 0.817, 95% CI = 0.713 to 0.937). Progression-free survival for patients receiving ziv-aflibercept was higher compared with placebo (HR = 0.758; 95% CI = 0.661 to 0.869). The most common adverse effects observed were anemia, diarrhea, and neutropenia. Ziv-aflibercept is a safe and effective option in combination with FOLFIRI for the treatment of mCRC in patients who progress on oxaliplatin-containing therapy. Superiority over other antiangiogenic treatment has not been established. PMID:24259608 Intravitreal aflibercept, a fusion protein with high affinity for vascular endothelial growth factor, offers an alternative treatment for exudative age-related macular degeneration. Preclinical studies and early and late phase clinical trials suggest that aflibercept's high binding affinity may impart greater durability of activity and increased efficacy compared to ranibizumab or bevacizumab. A total of 266 eyes of 249 patients with exudative age-related macular degeneration who received aflibercept after treatment with bevacizumab and/or ranibizumab were included in a retrospective review. Mean central subfoveal thickness on spectral-domain optical coherence tomography and mean logarithm of the minimal angle of resolution (logMAR) visual acuity were calculated at 1, 3, 6, and 12 months after the first aflibercept injection. Subgroup analyses were performed in eyes receiving at least 5 bevacizumab and/or ranibizumab injections in the 6 months prior to aflibercept and in eyes receiving at least 10 injections in the 12 months prior to aflibercept. Eyes received an average of 14.7 (range 1-43) ranibizumab and/or bevacizumab treatments prior to initiation of aflibercept therapy. The mean central subfoveal thickness decreased from 300 to 275 um at 1 month (p<0.001) and was maintained at 6 months. Mean logMAR visual acuity improved from 0.60 (Snellen equivalent 20/80) to 0.54 (20/70, p = 0.01) at 1 month and was stable at 0.55 at 6 months (Snellen equivalent 20/70, p = 0.11, n = 251). In 82 eyes receiving at least 5 injections in the 6 months prior to aflibercept treatment (average of 18.1 injections total), the central subfoveal thickness improved from 296 to 279 um at 1 month (p<0.0001) and was maintained at 6 months (p<0.0001). Visual acuity did not change (0.48 [20/61] at 1 month compared to baseline, 0.49 [20/62], p = 0.634, and at 6 months 0.51 [20/65], p = 0.601). In 50 eyes receiving at least 10 injections in the 12 months prior to aflibercept treatment (average of 21.8 injections total), the mean central subfoveal thickness decreased by 17 um at 1 month (p = 0.0007) and was maintained at 6 months (p = 0.013). Again, visual acuity did not change (0.46 [20/56] at 1 month, baseline 0.44 [20/56], p = 0.547, and 0.50 [20/63] at 6 months, p = 0.2445). Aflibercept is a valuable treatment alternative in patients previously treated with bevacizumab and/or ranibizumab injections. Stability of visual acuity and anatomic improvement on spectral-domain optical coherence tomography were observed after initiation of aflibercept treatment in those preciously treated with ranibizumab and/or bevacizumab injections every 4-6 weeks. PMID:24706352 To assess for change in intraocular pressure (IOP) in neovascular age-related macular degeneration patients switched to aflibercept after receiving previous treatments of intravitreal bevacizumab or ranibizumab. This is a retrospective chart review of the first 53 patients (53 eyes) treated with at least 2 injections of 2 mg in 0.05 mL of aflibercept by March 6, 2013, after at least 2 previous injections of 0.5 mg in 0.05 mL of ranibizumab with or without previous injections of 1.25 mg in 0.05 mL of bevacizumab. The analysis was restricted to the first such sequence within each patient. The last previous anti-vascular endothelial growth factor injection before the switch to aflibercept was ranibizumab in all cases included in the study. Each person served as his or her own control. The pre-aflibercept IOP in the before state (treatment with bevacizumab or ranibizumab) was the preinjection IOP measure before dilation at the visit of the first aflibercept injection. Statistical analysis was performed using Microsoft Excel. There were 41 patients who were first treated with ranibizumab followed by aflibercept and 12 patients treated with ranibizumab and bevacizumab followed by aflibercept. For each of these sequences, IOP in the treated eye during treatment with aflibercept (the after state) was computed in 3 different ways: the first IOP, the last IOP, and the mean IOP for the period when treated with aflibercept. The pooled data showed a mean pre-aflibercept (the before state) IOP of 14.87 that decreased to a mean first IOP of 14.57, mean last IOP of 13.79, and a mean IOP of 14.14 during aflibercept treatment. The inference is based on the pooled analysis. The 95% confidence interval for the differences (after minus before) were -0.30 (-1.12 to 0.52), -1.08 (-1.83 to -0.32), and -0.73 (-1.30 to -0.17) for the first, last, and mean IOPs, respectively. The corresponding P values were 0.46 for the first, 0.006 for the last, 0.01 for the mean IOP during the aflibercept treatment period. Intraocular pressure was found to be significantly lower in patients switched to aflibercept after previous treatments with ranibizumab and/or bevacizumab. Aflibercept may have a more favorable IOP safety profile in patients previously on other anti-vascular endothelial growth factor treatments. PMID:25072648 Aflibercept intravitreal injection is used for the treatment of neovascular (wet) age-related macular degeneration. Pharmacodynamics The equilibrium dissociation constants (KD) for aflibercept for various human receptors are as follow: 0.5 pM for VEGF-A165, 0.36 pM for VEGF-A121, 1.92 pM for VEGF-B, and 39 pM for PlGF-2. The effect of 6 mg per kg intravenous aflibercept every three weeks on QTc interval was evaluated in 87 patients with solid tumors in a randomized, placebo-controlled study. No large changes in the mean QT interval from baseline (i.e., greater than 20 ms as corrected for placebo) based on the Fridericia correction method were detected in the study. However, a small increase in the mean QTc interval (i.e., less than 10 ms) cannot be excluded due to the limitations of the study design. Mechanism of Action Aflibercept, a recombinant humanized fusion protein, is a vascular endothelial growth factor A (VEGF-A) and placental growth factor (PlGF) antagonist. The drug consists of portions of human VEGF receptor (VEGFR) 1 and 2 extracellular domains fused to the Fc portion of human immunoglobulin G1 (IgG1). Aflibercept acts as a soluble decoy receptor that binds to VEGF-A and PlGF and inhibits their biologic activity. VEGF-A and PlGF are angiogenic factors that can act as mitogenic, chemotactic, and vascular permeability factors for endothelial cells. VEGF-A induces neovascularization (angiogenesis) and increases vascular permeability, which appear to play a role in the pathogenesis and progression of the neovascular (wet) form of age-related macular degeneration, a leading cause of blindness in geriatric adults in developed countries. Binding of aflibercept to VEGF-A and PlGF prevents these factors from binding to endogenous VEGF receptors (i.e., VEGFR-1, VEGFR-2), reducing neovascularization and vascular permeability. The binding affinity of aflibercept for VEGF-A isoforms is higher than that of endogenous receptors; aflibercept blocks VEGF binding and activation of VEGFR-1 and VEGFR-2 even at low concentrations. Ablibercept is a recombinant fusion protein that acts as a decoy receptor for the ligands, vascular endothelial growth factor-A (VEGF-A) and placental growth factor (PIGF). It prevents these ligands to binding to endothelial receptors, VEGFR-1 and VEGFR-2, to suppress neovascularization and decrease vascular permeability. This ultimately will slow vision loss or the progression of metastatic colorectal cancer. |
| 分子量 |
97kD
|
|---|---|
| CAS号 |
862111-32-8
|
| 相关CAS号 |
Aflibercept (VEGF Trap); 862111-32-8; 845771-78-0
|
| 外观&性状 |
Colorless to light yellow liquid
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。