| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 50mg |
|

| 体外研究 (In Vitro) |
普罗帕酮 (5–25 μM) 可抑制食管鳞状细胞癌 (ESCC) 细胞的生长 [3]。普罗帕酮降低线粒体膜电位并降低 Bcl-xL 和 Bcl-2 的表达,从而导致线粒体功能障碍 [3]。研究发现,经普罗帕酮(10 和 20 μm)处理后,ESCC 细胞中抗凋亡蛋白 Bcl-xL 和 Bcl-2 的表达水平显着下调。此外,普罗帕酮可以降低 p-ERK 表达 [3]。
|
|---|---|
| 体内研究 (In Vivo) |
当给予普罗帕酮(20 mg/kg;每隔一天腹腔注射)时,肿瘤负荷显着降低了 69.2% [3]。此外,肿瘤细胞增殖显着降低(平均指数从 DMSO 治疗组的 56.3±6.7% 降至 10 mg/kg 普罗帕酮治疗组的 20.7±5.1%,从 20 mg/kg 普罗帕酮治疗组的 20.7±5.1% 降至普罗帕酮治疗组为 11.3±4.0%。治疗组)[3]。
|
| 细胞实验 |
细胞增殖测定[3]
细胞类型:人食管鳞状细胞癌细胞系KYSE30、KYSE150和KYSE270 测试浓度:5、10、15、20和 25 μm 孵育持续时间:24、48 和 72 小时 实验结果:随着时间的推移,KYSE30 中的细胞增殖逐渐减少, KYSE150和KYSE270细胞,随着浓度的增加,细胞增殖被有效抑制。 蛋白质印迹分析 [3] 细胞类型: 人类 ESCC 细胞系 KYSE30、KYSE150 和 KYSE270 测试浓度: 0, 10和 20 μm 孵育持续时间:72 小时 实验结果:Bcl-xL 和 Bcl-2 显着下调观察表达水平。 |
| 动物实验 |
Animal/Disease Models: Female BALB/c nude mice (6-8 weeks) carrying KYSE270 xenografts [3]
Doses: 10 mg/kg or 20 mg/kg Route of Administration: intraperitoneal (ip) injection Experimental Results:Significant effect on tumor growth Inhibitory xenografts. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Nearly completely absorbed following oral administration (90%). Systemic bioavailability ranges from 5 to 50%, due to significant first-pass metabolism. This wide range in systemic bioavailability is related to two factors: presence of food (food increases bioavailability) and dosage (bioavailability is 3.4% for a 150-mg tablet compared to 10.6% for a 300-mg tablet). Approximately 50% of propafenone metabolites are excreted in the urine following administration of immediate release tablets. 252 L In patients with ventricular arrhythmias and the extensive-metabolizer phenotype receiving 337.5, 450, 675, or 900 mg of propafenone hydrochloride daily (immediate-release tablets), the proportions of 5-hydroxypropafenone (5-OHP) to propafenone in plasma were 45, 40, 24, or 19%, respectively, while a subset of patients with the poor-metabolizer phenotype had higher relative plasma concentrations of the parent drug at each dosage and no detectable 5-OHP. Ratios of N-depropylpropafenone (NDPP) to propafenone are similar in extensive and poor metabolizers (approximately 10 and 6%, respectively). In poor metabolizers, NDPP is the principal metabolite and 5-OHP may not be detectable. Following oral administration of propafenone hydrochloride 300 mg (immediate-release tablets) every 8 hours for 14 days, plasma propafenone, 5-OHP, and NDPP concentrations averaged 1010, 174, and 179 ng/mL, respectively, in healthy individuals with the extensive-metabolizer phenotype. In an individual presumed to have the poor-metabolizer phenotype, plasma concentrations of propafenone, 5-OHP, and NDPP concentrations were 1048, undetectable, and 219 ng/mL, respectively, following oral administration of immediate-release tablets. Following administration of extended-release capsules of propafenone hydrochloride, plasma concentrations of 5-OHP and NDPP are generally less than 40 and 10% of plasma propafenone concentrations, respectively. The pattern of plasma concentrations of propafenone and its metabolites observed in an individual patient with long-term oral propafenone therapy depends principally on the genetically determined metabolizer phenotype and, to a lesser extent, on hepatic blood flow and enzyme function. Following oral administration of propafenone (immediate-release tablets), steady-state plasma concentrations of the parent drug and its metabolites are attained within 4-5 days in individuals with normal hepatic and renal function. Plasma concentrations of 5-hydroxypropafenone (5-OHP) and N-depropylpropafenone (NDPP) generally average less than 20% those of propafenone. Poor metabolizers achieve plasma propafenone concentrations 1.5-2 times higher than those of extensive metabolizers at propafenone hydrochloride dosages of 675-900 mg (immediate-release tablets) daily; at lower dosages, poor metabolizers may attain plasma propafenone concentrations more than fivefold higher than those of extensive metabolizers. The considerable degree of interindividual variability observed in the pharmacokinetics of propafenone in individuals with the extensive-metabolizer phenotype is principally attributable to first-pass hepatic metabolism and non-linear pharmacokinetics. The degree of interindividual variability in propafenone pharmacokinetic parameters is increased following single and multiple dose administration of propafenone hydrochloride extended-release capsules. The fact that interindividual variability in the pharmacokinetics of propafenone appears to be substantially less in individuals with the poor-metabolizer phenotype than in those with the extensive-metabolizer phenotype suggests that such variability may be due to CYP2D6 polymorphism rather than to the formulation. In healthy individuals, administration of propafenone hydrochloride as a single oral (300 or 450 mg immediate-release tablet) or IV (35-50 mg) dose produced similar peak plasma concentrations of the parent drug (278 versus 295 ng/mL, respectively). However, neither 5-hydroxypropafenone (5-OHP) nor N-depropylpropafenone (NDPP) was detectable in plasma after IV administration in these individuals. Since 5-OHP and NDPP has clinically important antiarrhythmic activity, propafenone's effect may differ with oral versus IV administration. Considerable interindividual variation exists in plasma concentrations of propafenone and its metabolites with a given dosage. Peak plasma concentrations of 5-OHP and NDPP average 101-288 and 8-40 ng/mL, respectively, in healthy individuals after administration of a single oral dose (300-450 mg) of propafenone hydrochloride immediate-release tablets. Propafenone, 5-OHP, and NDPP exhibit nonlinear pharmacokinetics in patients with the extensive-metabolizer phenotype, although the pharmacokinetics of 5-OHP and NDPP deviate from linearity only to a small extent. The pharmacokinetic profiles of propafenone, 5-OHP, and NDPP apparently are not affected substantially by age or gender. For more Absorption, Distribution and Excretion (Complete) data for Propafenone (15 total), please visit the HSDB record page. Metabolism / Metabolites Metabolized primarily in the liver where it is rapidly and extensively metabolized to two active metabolites, 5-hydroxypropafenone and N-depropylpropafenone. These metabolites have antiarrhythmic activity comparable to propafenone but are present in concentrations less than 25% of propafenone concentrations. In individuals with the extensive-metabolizer phenotype, propafenone is metabolized in the liver to 2 active metabolites and at least 9 additional metabolites. The 2 active metabolites, 5-hydroxypropafenone (5-OHP) and N-depropylpropafenone (NDPP), are formed through hydroxylation and dealkylation of the parent drug. Propafenone hydroxylation via cytochrome CYP2D6, a cytochrome P-450 isoenzyme under genetic control, produces 5-OHP. Formation of NDPP is catalyzed by different isoenzymes, cytochrome CYP1A2 and CYP3A4. Differences in metabolism between R- and S-propafenone related to stereoselective interaction with the CYP2D6 isoenzyme have been observed in animals and humans receiving single enantiomers of the drug. Following a 250 mg oral dose of R- or S-propafenone hydrochloride administered to adults with the extensive-metabolizer phenotype, the mean values for elimination half-life, clearance, and volume of distribution for R-propafenone were smaller than those for S-propafenone, while AUC was larger; however, these stereospecific effects were not observed in an adult with the poor-metabolizer phenotype who received the separate drug enantiomers. In vitro and in vivo studies indicate that the R-enantiomer is cleared faster than the S-enantiomer via the 5-hydroxylation pathway (CYP2D6). This results in a higher ratio of the S-enantiomer to R-enantiomer at steady state. Although the enantiomers have equivalent sodium-channel blocking potency, the S-enantiomer is a more potent beta-adrenergic antagonist than the R-enantiomer. Following administration of propafenone hydrochloride (immediate-release tablets or extended-release capsules), the observed ratio of S-enantiomer to R-enantiomer (S/R ratio) for AUC was approximately 1.7. The S/R ratios after administration of 225, 325, or 425 mg extended-release capsules were independent of dose. In addition, similar S/R ratios were observed among metabolizer genotypes and following long-term administration There are two principal patterns of propafenone metabolism. These patterns are genetically determined by an individual's ability to metabolize the drug via a hepatic oxidation pathway. The ability to oxidatively metabolize propafenone is dependent on an individual's ability to metabolize debrisoquin (debrisoquin phenotype). The debrisoquin phenotype or the observed pattern of propafenone metabolites may be used to determine an individual's metabolic phenotype for propafenone. Individuals who extensively metabolize propafenone via the oxidation pathway exhibit the extensive-metabolizer phenotype, while those who have an impaired ability to metabolize the drug by this pathway exhibit the poor-metabolizer phenotype. Approximately 90-95% of Caucasians exhibit the extensive-metabolizer phenotype, with the remainder being poor metabolizers. Propafenone metabolism in patients with the poor-metabolizer phenotype is characterized by a linear dose-concentration relationship and a relatively long terminal elimination half-life; these individuals have increased plasma propafenone concentrations relative to individuals with the extensive-metabolizer phenotype and are more likely to experience beta-adrenergic blocking and adverse effects of the drug. Propafenone has known human metabolites that include 5-Hydroxypropafenone and N-Despropylpropafenone. Biological Half-Life 2-10 hours Following single or multiple oral doses of immediate-release tablets in adults with the extensive-metabolizer phenotype and normal renal and hepatic function, the elimination half-life of propafenone averages about 1-3 hours (range: 2-10 hours). The half-life of propafenone averages approximately 8-13 hours (range: 6-36 hours) in adults with the poor-metabolizer phenotype. Following a single oral dose of 300 mg of propafenone hydrochloride as immediate-release tablets, a half-life of 3.5 hours was reported; after administration of 300 mg of propafenone hydrochloride daily for 1 and 3 months, the reported half-lives were 6.7 and 5.8 hours, respectively. Steady-state plasma elimination half-life of propafenone is prolonged in poor metabolizers, averaging 17.2 hours (range: 10-32 hours) compared with 5.5 hours (range: 2-10 hours) in extensive metabolizers. |
| 毒性/毒理 (Toxicokinetics/TK) |
Hepatotoxicity
In clinical trials, propafenone was associated with a low rate of serum aminotransferase and alkaline phosphatase elevations. Since its approval and more widescale use, propafenone has been linked to rare instances of clinically apparent liver injury, at least a dozen cases of which have been reported in the literature. Patients usually present with symptoms of jaundice and pruritus 2 to 8 weeks after starting propafenone, and the pattern of serum enzyme elevations are typically mixed (Case 1) or cholestatic (Case 2). Immunoallergic and autoimmune features are uncommon. While the jaundice can be prolonged, patients typically recover in 1 to 3 months and there have been no instances of acute liver failure, chronic hepatitis or vanishing bile duct syndrome attributed to its use. Likelihood score: B (rare but likely cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Limited information indicates that maternal doses of propafenone up to 900 mg daily produce low levels in milk. If propafenone is required by the mother it is not a reason to discontinue breastfeeding. Until more data become available, propafenone should be used with caution during breastfeeding, especially while nursing a newborn or preterm infant. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding 97% Interactions Although specific pharmacokinetic drug interaction studies are not available, the manufacturer of propafenone states that the drug should not be used concomitantly with other drugs that prolong the QT interval, including certain phenothiazines, cisapride, bepridil (not currently commercially available in the US), tricyclic antidepressant agents, or macrolides. Although specific pharmacokinetic drug interaction studies are not available, the manufacturer of ritonavir states that ritonavir should not be used concomitantly with certain cardiovascular agents, including propafenone, because of the potential for substantially increased plasma concentrations of these cardiovascular drugs and potentially serious and/or life-threatening adverse effects. This pharmacokinetic interaction may occur because ritonavir has high affinity for several cytochrome P-450 (CYP) isoenzymes (e.g., CYP3A, CYP2D6, CYP1A2) involved in propafenone metabolism. Increased serum theophylline concentrations have been reported in patients receiving theophylline concomitantly with propafenone and some clinicians suggest that serum theophylline concentrations and ECGs be monitored closely in patients receiving such combined therapy. The manufacturer states that concomitant use of propafenone and local anesthetic agents (i.e., during pacemaker implantation, surgery, or dental procedures) may increase the risk of adverse nervous system effects. For more Interactions (Complete) data for Propafenone (24 total), please visit the HSDB record page. Non-Human Toxicity Values LD50 Dogt iv 10 mg/kg /Propafenone hydrochloride/ LD50 Rat iv 18,800 ug/kg /Propafenone hydrochloride/ LD50 Rat oral 700 mg/kg /Propafenone hydrochloride/ |
| 参考文献 |
|
| 其他信息 |
Therapeutic Uses
Anti-Arrhythmia Agents When given as immediate-release tablets, propafenone hydrochloride is used to prolong the time to recurrence of symptomatic, disabling paroxysmal supraventricular tachycardia (PSVT) (e.g., atrioventricular (AV) nodal reentrant tachycardia or AV reentrant tachycardia ( Wolff-Parkinson-White syndrome)) and symptomatic, disabling paroxsymal atrial fibrillation/flutter (PAF) in patients without structural heart disease. While comparative studies are limited, propafenone appears to be comparable to other antiarrhythmic agents (e.g., quinidine, disopyramide, flecainide, procainamide, sotalol) in preventing recurrences of PAF and maintaining sinus rhythm following successful cardioversion of atrial fibrillation. /Included in US product label/ When given as extended-release capsules, propafenone is used to prolong the time to recurrence of symptomatic paroxysmal atrial fibrillation in patients without structural heart disease.289 The safety and efficacy of propafenone as extended-release capsules have not been established in patients with exclusively PSVT or atrial flutter. /Included in US product label/ Propafenone hydrochloride (immediate-release tablets) is used orally to suppress and prevent the recurrence of documented life-threatening ventricular arrhythmias (e.g., sustained ventricular tachycardia, ventricular fibrillation). Based on the results of the Cardiac Arrhythmia Suppression Trial (CAST), the US Food and Drug Administration (FDA), the manufacturer, and many clinicians recommend that therapy with antiarrhythmic agents, including propafenone, be reserved for the suppression and prevention of documented ventricular tachyarrhythmias that, in the clinician's judgment, are considered life-threatening. /Included in US product label/ For more Therapeutic Uses (Complete) data for Propafenone (10 total), please visit the HSDB record page. Drug Warnings In the National Heart, Lung and Blood Institute's Cardiac Arrhythmia Suppression Trial (CAST), a long-term, multi-center, randomized, double-blind study in patients with asymptomatic non-life-threatening ventricular arrhythmias who had a myocardial infarction more than six days but less than two years previously, an increased rate of death or reversed cardiac arrest rate (7.7%; 56/730) was seen in patients treated with encainide or flecainide (Class 1C antiarrhythmics) compared with that seen in patients assigned to placebo (3.0%; 22/725). The average duration of treatment with encainide or flecainide in this study was ten months. The applicability of the CAST results to other populations (e.g., those without recent myocardial infarction) or other antiarrhythmic drugs is uncertain, but at present it is prudent to consider any 1C antiarrhythmic to have a significant risk in patients with structural heart disease. Given the lack of any evidence that these drugs improve survival, antiarrhythmic agents should generally be avoided in patients with non-life-threatening ventricular arrhythmias, even if the patients are experiencing unpleasant, but not life-threatening, symptoms or signs. The most common adverse effects of propafenone involve the GI, cardiovascular, and central nervous systems and generally are dose related. Discontinuance of propafenone therapy was required in about 20% of patients receiving the drug in clinical trials. Drug discontinuance in patients treated for ventricular arrhythmias was required most frequently (i.e., in greater than 1% of patients) for proarrhythmia (4.7%), nausea and/or vomiting (3.4%), dizziness (2.4%), dyspnea (1.6%), congestive heart failure (1.4%), and ventricular tachycardia (1.2%). In patients treated for supraventricular arrhythmias in clinical trials, discontinuance of therapy was required most frequently (i.e., in greater than 1% of patients) for nausea and/or vomiting (2.9%), wide-complex tachycardia (1.9%), dizziness (1.7%), fatigue (1.5%), unusual taste (1.3%), and weakness (1.3%). Adverse nervous system effects reported in US clinical trials in patients receiving propafenone for the treatment of ventricular arrhythmias included dizziness and/or lightheadedness of patients, fatigue/lethargy in 6%, and headache in 5%.1 Weakness, ataxia, insomnia, or anxiety was reported in 2%, and tremor or drowsiness in 1% of patients receiving propafenone for ventricular arrhythmias. Pain or loss of balance also has been reported with propafenone therapy in patients with ventricular arrhythmias. Transient global amnesia, which resolved within hours after drug discontinuance, has been reported in at least one patient receiving propafenone. Peripheral neuropathy, which was characterized by episodic jabbing and crushing pain in the hands and feet and hyperesthesia of the extremities and resolved following discontinuance of the drug, has been reported rarely with propafenone therapy. For more Drug Warnings (Complete) data for Propafenone (31 total), please visit the HSDB record page. Pharmacodynamics Propafenone is a Class 1C antiarrhythmic drug with local anesthetic effects, and a direct stabilizing action on myocardial membranes. It is used in the treatment of atrial and ventricular arrhythmias. It acts by inhibiting sodium channels to restrict the entry of sodium into cardiac cells resulting in reduced excitation. Propafenone has local anesthetic activity approximately equal to procaine. |
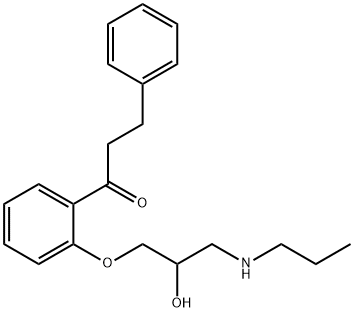
| 分子式 |
C21H27NO3
|
|---|---|
| 分子量 |
341.45
|
| 精确质量 |
341.199
|
| CAS号 |
54063-53-5
|
| 相关CAS号 |
Propafenone hydrochloride;34183-22-7;(S)-Propafenone;107381-32-8;Propafenone-d7 hydrochloride;1219799-06-0;Propafenone-d5 hydrochloride;1346605-05-7
|
| PubChem CID |
4932
|
| 外观&性状 |
White to off-white solid powder
|
| 密度 |
1.096 g/cm3
|
| 熔点 |
171 - 174ºC
|
| 闪点 |
268ºC
|
| 折射率 |
1.557
|
| LogP |
3.632
|
| tPSA |
58.56
|
| 氢键供体(HBD)数目 |
2
|
| 氢键受体(HBA)数目 |
4
|
| 可旋转键数目(RBC) |
11
|
| 重原子数目 |
25
|
| 分子复杂度/Complexity |
368
|
| 定义原子立体中心数目 |
0
|
| InChi Key |
JWHAUXFOSRPERK-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C21H27NO3/c1-2-14-22-15-18(23)16-25-21-11-7-6-10-19(21)20(24)13-12-17-8-4-3-5-9-17/h3-11,18,22-23H,2,12-16H2,1H3
|
| 化学名 |
1-[2-[2-hydroxy-3-(propylamino)propoxy]phenyl]-3-phenylpropan-1-one
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.9287 mL | 14.6434 mL | 29.2869 mL | |
| 5 mM | 0.5857 mL | 2.9287 mL | 5.8574 mL | |
| 10 mM | 0.2929 mL | 1.4643 mL | 2.9287 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。