| 规格 | 价格 | ||
|---|---|---|---|
| 500mg | |||
| 1g | |||
| Other Sizes |

| 靶点 |
Human D1 Receptor; human 5-HT2; Human D4 Receptor; Human D2Receptor
|
|---|---|
| 体外研究 (In Vitro) |
在洛沙平存在的情况下,[3H]酮色林附着在人和牛大脑额叶皮质中的 5-HT2 受体上,Ki 值分别为 6.2 nM 和 6.6 nM。在使用人膜的竞争测定中,洛沙平对不同受体的效力分级如下:5-HT2≥D4>>>>>D1>D2[1]。在 LPS 激活的混合神经胶质细胞培养物中,洛沙平 (0–20 μM) 会降低 IL-1β 的分泌;在混合神经胶质细胞培养物中,它会减少 IL-2 的分泌;在小胶质细胞中,它会减少 LPS 诱导的 IL-1β 和 IL-2 分泌 [2]。
|
| 体内研究 (In Vivo) |
在大鼠大脑中,洛沙平(5 mg/kg;腹腔注射;每日一次,持续 4 或 10 周)会减少血清素 (S2),但不会增加多巴胺 (D2) 受体的数量 [3]。
|
| 酶活实验 |
受体结合测定-多巴胺、5-HT2、NMDA受体[1]
为了进行受体结合测定,将0.8 nM的[3H]SCH23390(Di受体拮抗剂)、0.5 nM的[3H]螺环哌啶醇(D2和D4受体拮抗剂”)、0.5 nM的[3H]酮色林(5-HT2受体拮抗剂“)和2.0 nM的[3H]MK801(NMDA受体拮抗剂,)与150μg的膜蛋白一起孵育,最终体积为1 ml。在1μM(+)丁咯酚(D2和D4-测定)、10μM顺式氟戊噻醇(Di测定)、2μM甲氧基嘧啶(5-HT2测定)和50μM MK801(NMDA测定)存在的情况下,在平行测定中测定非特异性结合。使用[3H]螺环哌啶醇的检测还包括50 nM酮色林,以阻断血清素能位点的存在。对于竞争实验,在测定管中加入了不同浓度的洛沙平。Di、D2、5-HT2和NMDA受体分别在25°C下孵育90分钟、25°C孵育60分钟、37°C孵孵育15分钟和25°C孵化120分钟。使用膜制备部分所述的细胞结合缓冲液,在22°C下孵育COS细胞的D4受体结合试验120分钟。在孵育结束时,通过在Whatman GF/B过滤器上快速过滤来分离结合和游离配体,用5 ml冷过滤缓冲液洗涤3次:(50 mM Tris-HCL,1.0 mM EDTA,pH 7.4)用于[3H]螺哌啶醇和[3H]SCH23390测定,(50 mM Tr-HCL,pH 7.4。使用贝克曼闪烁计数器(型号LS 5000TA)测量结合放射性。
|
| 细胞实验 |
细胞因子IL-1β和IL-2由中枢神经系统中活化的神经胶质细胞释放,能够增强儿茶酚胺能神经传递。目前尚无关于抗精神病药物对神经胶质细胞活性影响的数据。到达大脑的抗精神病药物不仅作用于神经元,还可能作用于神经胶质细胞。本研究旨在评估氯丙嗪和洛沙平对混合胶质细胞和小胶质细胞培养中IL-1β和IL-2释放的影响。浓度为2和20μM的氯丙嗪以及0.2、2和20微M的洛沙平在暴露1天和3天后减少了LPS激活的混合胶质细胞培养物的IL-1β分泌。0.2、2和20微M浓度的氯丙嗪在接触3天后降低了混合神经胶质培养物中IL-2的分泌。0.2、2和20μM浓度的洛沙平在暴露1和3天后降低了混合胶质细胞培养物中IL-2的分泌,此外,洛沙平还降低了2、10和20μm浓度的LPS诱导的小胶质细胞培养中IL-1β和IL-2的分泌。Quinpirole是一种D2多巴胺能激动剂,仅在20微M的最高剂量下增加了LPS诱导的混合胶质细胞培养中IL-1β和IL-2的分泌。这些发现表明皮质小胶质细胞上缺乏功能性多巴胺受体。去除小胶质细胞的混合胶质细胞培养物(通过摇晃和用L-亮氨酸甲酯孵育)不释放IL-1β和IL-2。这一观察表明,小胶质细胞可能是评估细胞因子的来源。本研究的结果支持了抗精神病药物不仅作用于神经元,而且作用于神经胶质细胞的观点。然而,这些观察结果的临床意义尚不清楚[2]。
|
| 动物实验 |
Animal/Disease Models: Adult male Wistar rat (150-175 g) [3]
Doses: 5 mg/kg Route of Administration: intraperitoneal (ip) injection, one time/day for 4 or 10 weeks Experimental Results: Induced significant reduction in serotonin (S2) (more than 50%)) daily injections increased receptor density after 4 or 10 weeks, but did not produce any significant increase in dopamine receptor density. |
| 药代性质 (ADME/PK) |
Absorption
Systemic bioavailability of the parent drug was only about one third that after an equivalent intramuscular dose (25 mg base) in male volunteers Route of Elimination Metabolites are excreted in the urine in the form of conjugates and in the feces unconjugated. Animal studies with radioactive drug indicate that loxapine and/or its metabolites are widely distributed in body tissues with highest concentrations in brain, lungs, heart, liver, and pancreas. The drug appears in the CSF. Loxapine is rapidly and almost completely absorbed from the GI tract. The drug is also almost completely absorbed following IM administration. RAPIDLY & ALMOST COMPLETELY ABSORBED FROM GI TRACT. PEAK LOXAPINE SERUM LEVELS /WITHIN 2 HR, RANGE FROM 0.006 TO 0.013 MCG/ML AFTER/ 25 MG ORAL DOSE...MAJOR /ACTIVE/ METABOLITE IN SERUM IS 8-HYDROXYLOXAPINE /MAX CONCN 0.012-0.038 MCG/ML WITHIN 2-4 HR AFTER ORAL LOXAPINE. HUMAN/ LOXAPINE AND/OR METABOLITES...WIDELY DISTRIBUTED IN BODY TISSUES...HIGHEST CONCN IN BRAIN, LUNGS, HEART, LIVER, & PANCREAS...APPEARS IN CSF...CROSSES PLACENTA...IN MILK OF NURSING MOTHERS /ANIMALS, RADIOACTIVE DRUG/ METABOLITES /7- & 8-HYDROXY-, 7- & 8-HYDROXYDESMETHYLLOXAPINE; N-OXIDES OF LOXAPINE, 7- & 8-HYDROXYLOXAPINE/ EXCRETED IN URINE & FECES. LITTLE OR NO UNMETABOLIZED DRUG...FOUND...METABOLITES /PRIMARILY GLUCURONIDE OR SULFATE CONJUGATES IN URINE, PRIMARILY UNCONJUGATED IN FECES. HUMAN, ORAL/ View More
Metabolism / Metabolites
Biological Half-Life Oral-4 hours SERUM LEVELS OF LOXAPINE & METABOLITES DECLINE IN BIPHASIC MANNER. HALF-LIFE DURING 1ST PHASE...5 HR...DURING 2ND PHASE...19 HR. /AFTER SINGLE 25 MG ORAL DOSE, SEDATIVE EFFECT BEGINS IN 20-30 MIN; PEAK EFFECT WITHIN 1.5-3 HR; DURATION APPROX 12 HR. HUMAN/ |
| 毒性/毒理 (Toxicokinetics/TK) |
Reported Fatal Dose
A 2500 mg ingestion ... proved fatal ... Toxicity Data LD50=65 mg/kg (Orally in mice) Non-Human Toxicity Values Toxicity Summary Loxapine is a dopamine antagonist, and also a serotonin 5-HT2 blocker. The exact mode of action of Loxapine has not been established, however changes in the level of excitability of subcortical inhibitory areas have been observed in several animal species in association with such manifestations of tranquilization as calming effects and suppression of aggressive behavior. Hepatotoxicity Liver test abnormalities have been reported to occur in a small proportion of patients on long term therapy with loxapine, but elevations are uncommonly above 3 times the upper limit of normal. The aminotransferase abnormalities are usually mild, asymptomatic and transient, reversing even with continuation of medication. Instances of clinically apparent acute liver injury have been reported due to loxapine and to the structurally related tricylic amoxapine (not available in the United States), but cases are rare. In reported cases, the onset of jaundice was within 4 to 8 weeks, and the pattern of serum enzyme elevations was typically hepatocellular. Immunoallergic features and autoantibody formation were not prominent. All cases were self-limited without fatalities or residual chronic liver injury. Likelihood score: D (possible rare cause of clinically apparent liver injury). View More
LD50 Rat oral 151 mg/kg Exposure Routes Oral, Intramuscular. Systemic bioavailability of the parent drug was only about one third that after an equivalent intramuscular dose (25 mg base) in male volunteers. Treatment The treatment of overdosage is essentially symptomatic and supportive. Early gastric lavage and extended dialysis might be expected to be beneficial. Centrally-acting emetics may have little effect because of the antiemetic action of loxapine. In addition, emesis should be avoided because of the possibility of aspiration of vomitus. Avoid analeptics, such as pentylenetetrazol, which may cause convulsions. Severe hypotension might be expected to respond to the administration of levarterenol or phenylephrine. Epinephrine should not be used since its use in a patient with partial adrenergic blockade may further lower the blood pressure. Severe extrapyramidal reactions should be treated with anticholinergic antiparkinson agents or diphenhydramine hydrochloride, and anticonvulsant therapy should be initiated as indicated. Additional measures include oxygen and intravenous fluids. (L1712) Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Because no information is available on the use of loxapine during breastfeeding, an alternate drug may be preferred, especially while nursing a newborn or preterm infant. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Loxapine can elevate serum prolactin. The hyperprolactinemia is caused by the drug's dopamine-blocking action in the tuberoinfundibular pathway. The prolactin level in a mother with established lactation may not affect her ability to breastfeed. |
| 参考文献 |
[1]. Singh AN, et al. A neurochemical basis for the antipsychotic activity of loxapine: interactions with dopamine D1, D2, D4 and serotonin 5-HT2 receptor subtypes. J Psychiatry Neurosci. 1996 Jan;21(1):29-35.
[2]. Labuzek K, et al. Chlorpromazine and loxapine reduce interleukin-1beta and interleukin-2 release by rat mixed glial and microglial cell cultures. Eur Neuropsychopharmacol. 2005 Jan;15(1):23-30. [3]. Lee T, et al. Loxapine and clozapine decrease serotonin (S2) but do not elevate dopamine (D2) receptor numbers in the rat brain. Psychiatry Res. 1984 Aug;12(4):277-85. [4]. Keating GM. Loxapine inhalation powder: a review of its use in the acute treatment of agitation in patients with bipolar disorder or schizophrenia. CNS Drugs. 2013 Jun;27(6):479-89. |
| 其他信息 |
An antipsychotic agent used in schizophrenia.
See also: Loxapine (has active moiety). |
| 分子式 |
C18H18N3OCL.HCL
|
|---|---|
| 分子量 |
364.26896
|
| 精确质量 |
363.09
|
| CAS号 |
54810-23-0
|
| 相关CAS号 |
Loxapine;1977-10-2;Loxapine succinate;27833-64-3;Loxapine-d8 hydrochloride;1246820-19-8;Loxapine-d8;1189455-63-7
|
| PubChem CID |
71400
|
| 外观&性状 |
Typically exists as solid at room temperature
|
| 沸点 |
458.6ºC at 760 mmHg
|
| 熔点 |
109-110ºC
|
| 闪点 |
231.1ºC
|
| LogP |
3.884
|
| tPSA |
28.07
|
| 氢键供体(HBD)数目 |
1
|
| 氢键受体(HBA)数目 |
3
|
| 可旋转键数目(RBC) |
1
|
| 重原子数目 |
24
|
| 分子复杂度/Complexity |
450
|
| 定义原子立体中心数目 |
0
|
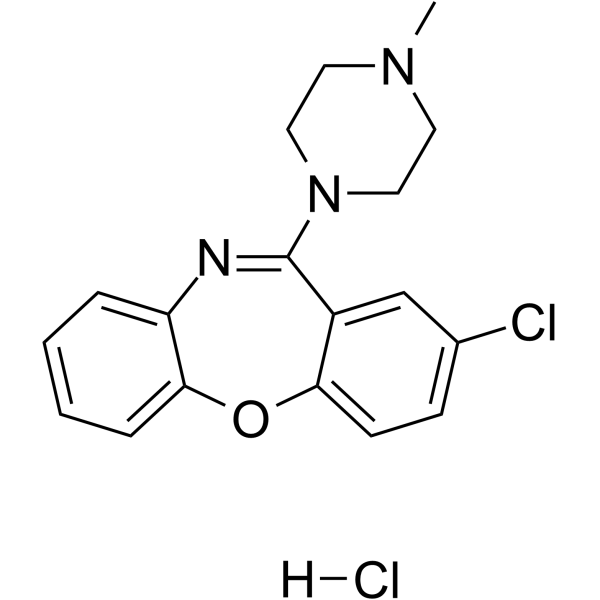
| SMILES |
CN1CCN(CC1)C2=NC3=CC=CC=C3OC4=C2C=C(C=C4)Cl.Cl
|
| InChi Key |
JSXBVMKACNEMKY-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C18H18ClN3O.ClH/c1-21-8-10-22(11-9-21)18-14-12-13(19)6-7-16(14)23-17-5-3-2-4-15(17)20-18;/h2-7,12H,8-11H2,1H3;1H
|
| 化学名 |
8-chloro-6-(4-methylpiperazin-1-yl)benzo[b][1,4]benzoxazepine;hydrochloride
|
| 别名 |
Loxapine hydrochloride; Loxapine HCl; LOXITANE C; 54810-23-0; Loxitane IM; UNII-376MYL4MAL; 376MYL4MAL; Loxapine (hydrochloride);
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.7452 mL | 13.7261 mL | 27.4522 mL | |
| 5 mM | 0.5490 mL | 2.7452 mL | 5.4904 mL | |
| 10 mM | 0.2745 mL | 1.3726 mL | 2.7452 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。