| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
| 靶点 |
K+/H+ ionophore; NLRP3
|
|---|---|
| 体外研究 (In Vitro) |
通过 caspase 1/GSDMD,尼日利亚霉素(0–4 μg/ml;24 小时)有效引起 TNBC 细胞焦亡 [6]。凭借其集中作用,尼日利亚菌素(0-0.25 μg/ml;24 小时)可抑制 H460 细胞中 Wnt/β-连环蛋白的上调,并表现出抗癌特性 [7]。革兰氏阳性菌对抗生素具有耐药性[4]。
|
| 体内研究 (In Vivo) |
通过每 12 小时腹腔注射 1 mg/kg 尼日利亚霉素,持续三天,可以减少金黄色葡萄球菌 USA300 感染的小鼠 [4]。尼日利亚霉素(皮下注射,每两天一次;0.025 mg/kg)。
体积数据表明,ngericin(4 mg/kg,腹腔注射)表现出肿瘤生长的显着减少,并与化疗剂 DDP 表现出良好的相互作用。在体内,尼日利亚菌素可显着降低 Bmi-1。在尼日利亚素处理下,鼻咽癌细胞的CSC含量和转移潜力部分受到Bmi-1过表达的影响。尼日利亚菌素对鼻咽癌干细胞的抑制可能与Bmi-1的下降有关[3]。 尼日利亚菌素对CSCs在体内表现出选择性毒性[3] 为评价尼日利亚菌素对鼻咽癌细胞的体内作用,将分别皮下接种S18和S26细胞的裸鼠随机分为4个亚组,分别给药、DDP、尼日利亚菌素或DPP和尼日利亚菌素联合给药。在S18组中,尼日利亚菌素显著抑制肿瘤生长,并与化疗药物DDP协同作用,从肿瘤体积来看(P < 0.05或<0.01,图6A)。然而,在S26组中,尼日利亚菌素仅轻微抑制S26异种移植物的生长,而DDP单独或联合尼日利亚菌素均显著抑制肿瘤生长(P < 0.05或<0.01,图6B)。重要的是,与对照组相比,每种药物治疗对小鼠体重的减轻都有影响,从尼日利亚菌素,DDP到两种药物的联合,其严重程度逐渐增加(图6C)。 免疫组化分析显示,尼日利亚菌素处理组S18异种移植物中Bmi-1的表达较低,提示尼日利亚菌素可以下调体内Bmi-1。 此外,我们还评估了尼日利亚菌素治疗后参与Bmi-1通路的两个分子PTEN和Snail的变化。正如预期的那样,与对照组相比,在体内使用尼日利亚菌素后,PTEN蛋白水平升高,蜗牛表达降低。这些结果表明,Bmi-1的下调可能有助于尼日利亚菌素对NPC CSCs的抑制作用。 接下来,我们在4T1异种移植物模型中评估了Nigericin与抗pd -1抗体的协同抗肿瘤作用,该模型包括相对冷的肿瘤,并且由于缺乏T细胞浸润和激活而对免疫检查点抑制剂治疗产生抗性[43,44]。将4T1细胞原位移植到BALB/c小鼠乳腺脂肪垫中。将小鼠随机分为4组,分别给予对照组、尼日利亚菌素(皮下注射)或抗pd -1抗体(腹腔注射)单独和联合治疗。正如预期的那样,单独的PD-1抗体没有明显的抗肿瘤作用,而尼日利亚菌素则有中等的抗肿瘤作用。尼日利亚菌素与抗pd -1抗体联合使用几乎完全抑制肿瘤生长(图6B-D)。在尼日利亚菌素治疗组和联合治疗组中,肿瘤浸润CD4+或CD8+ T细胞的数量一致增加(图6E),提示尼日利亚菌素介导的热亡调节肿瘤微环境,促进T细胞浸润,从而使冷肿瘤转变为热肿瘤。尼日利亚菌素和抗pd -1联合治疗组CD4+或CD8+细胞分泌的TNF-α和IFN-γ水平较高(图6F和图S4C)。根据上述结果,在尼日利亚菌素处理组中,Caspase-1和Caspase-3的裂解量也有所增加(图6F)。此外,我们没有观察到尼日利亚菌素影响免疫细胞和癌细胞中PD-1或PD-L1的表达(图S4D)。这些数据证实了尼日利亚菌素与抗pd -1抗体的协同抗肿瘤作用。 同时,在体内评估了这些治疗的系统性副作用。心、肝、脾、肺、肾组织未见明显组织学毒性(图S5A)。治疗结束时,血液学参数包括白细胞、血红蛋白、天冬氨酸转氨酶、丙氨酸转氨酶、白蛋白和肌酐均在正常范围内(图S5B)。总之,这些结果表明,应用尼日利亚菌素是使tnbc对免疫检查点阻断治疗增敏的有效策略,并且系统副作用可接受。[5] 尼日利亚霉素对USA300感染小鼠模型有效[6] 由于NIG出色的抗菌性能及其在感染动物模型中的疗效尚未得到评价,我们进一步利用金黄色葡萄球菌USA300感染小鼠模型来测试NIG的体内疗效。我们首先使用金黄色葡萄球菌USA300菌株的小鼠深部生物膜感染模型来模拟人类深部慢性感染。每只小鼠大腿注射5 × 107 CFU金黄色葡萄球菌USA300。细菌感染24小时后,小鼠每12小时腹腔注射50 mg/kg VAN或1 mg/kg NIG,连续3天。VAN处理没有显著降低金黄色葡萄球菌USA300的丰度,这表明在该模型中存在对VAN耐受的细菌群体(图3A)。值得注意的是,NIG治疗导致感染大腿的USA300负荷减少了约103倍(图3A)。NIG在体内减少固定细胞和生物膜数量的效果令人鼓舞。 然后,我们使用了金黄色葡萄球菌USA300菌株的创伤感染模型。在小鼠背部皮肤上穿孔创口,随后感染金黄色葡萄球菌USA300。感染后第1天,应用NIG软膏,每日1次,连用9天。结果显示,NIG将伤口中的USA300负荷降低了约104倍(图3B)。同时,NIG治疗10天后伤口大小减少了80%,莫匹罗星(一种已建立的抗葡萄球菌药物)也是如此(图3C, D),这表明NIG和莫匹罗星可能通过大幅减少感染部位的细菌负荷来促进伤口愈合。通过感染皮肤的苏木精和伊红(H&E)染色,usa300感染小鼠的皮肤表皮层被破坏,间质中有大量淋巴细胞浸润,而莫匹罗星或NIG处理小鼠的皮肤结构愈合程度更高,间质中淋巴细胞水平降低(图3E)。值得注意的是,NIG的疗效与莫匹罗星相当,但浓度低8,000倍。 进一步采用小鼠血流感染模型。小鼠尾静脉注射致死剂量USA300 1小时后,每12 h给药(经ip),连续3天。1mg /kg NIG处理显著延长了usa300感染小鼠的存活时间,与5mg /kg VAN处理小鼠的存活时间相当(图3F)。感染72 h后检测心脏、肝脏、脾脏、肺和肾脏中USA300的细菌载量。NIG治疗使主要器官的细菌负担减少了1000到10000倍。1 mg/kg NIG的效果略好于2.5 mg/kg VAN(图3G-K)。这些结果证明了NIG在体内治疗金黄色葡萄球菌感染的有效性。 |
| 酶活实验 |
K(+)、H(+)离子载体和抗生素黑曲霉素已被证明可以引发细胞凋亡,因此被认为可以治疗恶性肿瘤。所涉及的细胞机制包括诱导氧化应激,已知氧化应激会激活红细胞内可渗透钙的非选择性阳离子通道,导致钙进入,增加细胞质钙活性([Ca(2+)]i),随后刺激红细胞凋亡,这是一种自杀性红细胞死亡,其特征是细胞收缩和细胞膜紊乱,磷脂酰丝氨酸易位到红细胞表面。本研究探讨了黑曲霉素是否以及如何诱导红细胞凋亡。根据膜联蛋白V结合、前向散射的细胞体积、Fluo3荧光的[Ca(2+)]i、BCECF荧光的pHi、利用抗体的神经酰胺丰度和DCFDA依赖性荧光的活性氧(ROS)形成来估计细胞表面的磷脂酰丝氨酸暴露量。人红细胞暴露于黑曲霉素48小时后,膜联蛋白-V结合细胞的百分比显著增加(0.1-10 nM),前向散射显著降低(0.1-1 nM)、细胞质pH值显著降低(0.1-1 nM)和Fluo3荧光显著增加(0.1-10 nM)。黑种草素(1 nM)略微但显著地增加了ROS,但没有显著改变神经酰胺的丰度。黑曲霉素对膜联蛋白V结合的影响显著减弱,但去除细胞外钙(2+)不会消除。nigericin诱导的[Ca(2+)]i和膜联蛋白V结合的增加再次被Na(+)/H(+)交换抑制剂cariporide(10μM)显著减弱,但没有被消除。黑种皮素引发红细胞下垂,这是一种与ROS形成平行的效应,部分依赖于Ca(2+)进入的刺激,并涉及cariporide敏感的Na(+)/H(+)交换器[3]。
|
| 细胞实验 |
细胞活力测定 [4]
细胞类型:金黄色葡萄球菌、表皮葡萄球菌、粪肠球菌、屎肠球菌、肺炎链球菌)和无乳链球菌 测试浓度: 0 μg/ml、0.05 μg/ml、0.125 μg/ml、0.25 μg/ml 孵育时间:24 小时 实验结果:表现出对这些临床 MDR 菌株的有效活性,MIC 值范围为 0.004-0.25 mg/ml。 蛋白质印迹分析[6] 细胞类型: MDA-MB-231 和 4T1 细胞 测试浓度: 0 μg/ml ,2 μg/ml,4 μg/ml 孵育时间:24 小时 实验结果:显示 caspase 1 蛋白水平增加和 N-GSDMD 。 细胞活力测定 [7] 细胞类型: H460 细胞 测试浓度: 0.5 μM、1 μM、2.5 μM 孵育持续时间:24 小时 实验结果:经典 Wnt 蛋白(LRP6、Wnt5a/b 和 β-)表达下调连环蛋白)信号通路。 人结直肠癌癌症细胞系HT29和SW480在规定的条件下用nigericin/尼格瑞辛或奥沙利铂处理。进行细胞活力测定和侵袭转移测定,以评估nigericin对CRC细胞的影响。采用球化试验和软琼脂集落形成试验来评估尼格瑞金对经上皮-间质转化(EMT)的CRC细胞的癌症干细胞特性的作用。 结果:与奥沙利铂相比,nigericin对HT29细胞系的毒性更大(IC50,12.92±0.25μmol vs 37.68±0.34μmol)。SW116细胞系也得到了类似的结果(IC50,15.86±0.18μmol vs 41.02±0.23μmol)。Boyden室试验表明,与载体处理组相比,nigericin/尼日利亚霉素处理组中通过聚偏二氟乙烯膜迁移的HT29细胞数量显著减少[11±2个细胞/高倍视野(HPF)vs 19.33±1.52个细胞/HPF,P<0.05)。与对照组相比,nigericin处理组侵入Matrigel涂层膜的HT29细胞数量也减少了(每HPF 6.66±1.52个细胞vs每HPF 14.66±1.51个细胞,P<0.05)。与对照组相比,nigericin还将CD133+细胞的比例从83.57%降低到63.93%(P<0.05)。与对照组相比,nigericin减少了球体的数量(0.14±0.01 vs 0.35±0.01,P<0.05),而奥沙利铂增加了球体的数目(0.75±0.02 vs 0.35±01;P<0.05)。与对照组相比,在标准软琼脂试验中,培养14天后,nigericin在非锚定条件下形成集落的能力也降低了(1.66±0.57 vs 7±1.15,P<0.05),而奥沙利铂组的集落数高于赋形剂处理的对照组(14.33±0.57 vs7±1.15,P<0.05)。我们进一步检测了经nigericin和奥沙利铂处理的细胞中E-钙粘蛋白和波形蛋白的表达。结果表明,与载体对照相比,用nigericin处理的HT29细胞诱导E-钙粘蛋白表达增加,波形蛋白表达减少。相比之下,与载体对照组相比,奥沙利铂下调了HT29细胞中E-cadherin的表达,上调了波形蛋白的表达。 结论:本研究表明,nigericin可以部分逆转细胞侵袭和转移过程中的EMT过程[4]。 |
| 动物实验 |
Animal/Disease Models: balb/c (Bagg ALBino) mouse orthotopically injected with 4T1 cells [6]
Doses: 0.025 mg/kg Route of Administration: subcutaneous injection Experimental Results: Shown almost complete inhibition of tumor growth with anti-PD-1 antibody. Animal/Disease Models: Staphylococcus aureus-infected mice USA300[4] Doses: 1 mg/kg Route of Administration: intraperitoneal (ip) injection Experimental Results: Major The bacterial load in the organs is diminished to 1,000-10,000 times. Deep-seated mouse biofilm infection model [6] A previously reported deep-seated mouse biofilm infection model (Conlon et al., 2013) was used with modifications. 100 μL of stationary-phase S. aureus USA300 (5 × 107 CFU) was injected to the thigh of each mouse. Starting at 24 h post-infection, mice were administrated with 200 µL of nigericin (1 mg/kg, dissolved in 20% (w/v) Kolliphor® HS 15), vancomycin (50 mg/kg), or vehicle intraperitoneally every 12 h for 3 days. Mice were sacrificed 4 days post-infection, and their infected thighs were homogenized, diluted, and plated on MH agar for determination of CFU. Murine wound infection [6] Murine wounds were generated as round lesions having a diameter of 1 cm on the back of each mouse. Each wound was then infected with 10 μL of 3 × 107 CFU/mL S. aureus USA300. Staring at 24 h post-infection, nigericin (0.025 μg per wound) or mupirocin (200 μg per wound), diluted in 0.1% EtOH, was applied to the wounds once daily for 9 days. The wounds were monitored at 1, 5- and 10-days post-infection. The wound tissues were excised and grounded, and aliquots of the grounded tissue were diluted in normal saline and plated on drug-free agar to determine CFU. A portion of the wound tissue was also subjected to hematoxylin and eosin (H&E) staining for histopathological analysis. Murine bloodstream infection model [6] Mice were infected by intravenous injection of 100 μL 1 × 108 CFU/mL S. aureus USA300. Starting at 4 h post-infection, nigericin (0.5, 1 mg/kg, dissolved in 20% (w/v) Kolliphor® HS 15), vancomycin (5 mg/kg), or vehicle (20% (w/v) Kolliphor® HS 15) in a volume of 200 µL was administrated via the intraperitoneal route every 12 h for 3 d. Survival curves were recorded during 3 days of treatment. For determining the bacterial loads of USA300, the mice were sacrificed 3 days post-infection, and their hearts, livers, spleens, lungs, and kidneys were homogenized, diluted, and plated on MH agar for determination of CFU. Six-to-eight-week old female immunocompetent BALB/c mice were used. Next, 5 × 105 4T1 cells were injected orthotopically into the left inguinal mammary fat pad of BALB/c mice. Mice were randomly divided into four groups and treated at the same time with indicated drugs. Nigericin (2 mg/kg) was injected subcutaneously every two days, and anti-PD-1 (250 μg/mouse) was injected intraperitoneally every week. Tumor volumes were monitored every three-to-four days. At the end of the experiment (after about 4 weeks), the mice were sacrificed via carbon dioxide euthanasia, and tumors were harvested for further analysis.[5] The S18 cells were injected near the scapula of the nude mice. Nine days after injection, the mice were randomly divided into four groups with six animals each (control, DDP, nigericin and DDP combined with nigericin). DDP (2.5 mg/kg) was injected intraperitoneally for five continuous days and nigericin (4 mg/kg) was administrated intraperitoneally every two days. Tumor length and width were measured with a vernier caliper every other day. Tumor volume was calculated using the formula V = 0.5 × (length × width2). The body weights of the mice were recorded every two days. Mice were humanely euthanized when the tumor volume reached 2000 mm3.[3] |
| 毒性/毒理 (Toxicokinetics/TK) |
mouse LD50 oral 190 mg/kg CRC Handbook of Antibiotic Compounds, Vols.1- , Berdy, J., Boca Raton, FL, CRC Press, 1980, 5(477), 1981
mouse LD50 intraperitoneal 2500 ug/kg Antibiotics and Chemotherapy, 1(594), 1951 |
| 参考文献 |
|
| 其他信息 |
Nigericin is a polyether antibiotic which affects ion transport and ATPase activity in mitochondria. It is produced by Streptomyces hygroscopicus. It has a role as an antimicrobial agent, an antibacterial agent, a potassium ionophore and a bacterial metabolite.
A polyether antibiotic which affects ion transport and ATPase activity in mitochondria. It is produced by Streptomyces hygroscopicus. (From Merck Index, 11th ed) Nigericin has been reported in Streptomyces, Streptomyces violaceusniger, and Streptomyces hygroscopicus with data available. A polyether antibiotic which affects ion transport and ATPase activity in mitochondria. It is produced by Streptomyces hygroscopicus. (From Merck Index, 11th ed) Multiple factors including tumor heterogeneity and intrinsic or acquired resistance have been associated with drug resistance in lung cancer. Increased stemness and the plasticity of cancer cells have been identified as important mechanisms of resistance; therefore, treatments targeting cancer cells independent of stemness phenotype would be much more effective in treating lung cancer. In this article, we have characterized the anticancer effects of the antibiotic Nigericin in cells displaying varying degrees of stemness and resistance to anticancer drugs, arising from (1) routine culture conditions, (2) prolonged periods of serum starvation. These cells are highly resistant to conventional anticancer drugs such as Paclitaxel, Hydroxyurea, Colchicine, Obatoclax, Wortmannin, and LY294002, and the multidrug-resistant phenotype of cells growing under prolonged periods of serum starvation is likely the result of extensive rewiring of signaling pathways, and (3) lung tumorspheres that are enriched for cancer stem-like cells. We found that Nigericin potently inhibited the viability of cells growing under routine culture conditions, prolonged periods of serum starvation, and lung tumorspheres. In addition, we found that Nigericin downregulated the expression of key proteins in the Wnt canonical signaling pathway such as LRP6, Wnt5a/b, and β-catenin, but promotes β-catenin translocation into the nucleus. The antitumor effects of Nigericin were potentiated by the Wnt activator HLY78 and by therapeutic levels of the US Food and Drug Administration-approved drug Digitoxin and its novel synthetic analog MonoD. We believe that Nigericin may be used in a co-therapy model in combination with other novel chemotherapeutic agents in order to achieve potent inhibition of cancers that display varying degrees of stemness, potentially leading to sustained anticancer effects. [1] The K(+),H(+) ionophore and antibiotic nigericin has been shown to trigger apoptosis and is thus considered for the treatment of malignancy. Cellular mechanisms involved include induction of oxidative stress, which is known to activate erythrocytic Ca(2+)-permeable unselective cation channels leading to Ca(2+) entry, increase in cytosolic Ca(2+) activity ([Ca(2+)]i) and subsequent stimulation of eryptosis, the suicidal erythrocyte death characterized by cell shrinkage and cell membrane scrambling with phosphatidylserine translocation to the erythrocyte surface. This study explored whether and how nigericin induces eryptosis. Phosphatidylserine exposure at the cell surface was estimated from annexin V binding, cell volume from forward scatter, [Ca(2+)]i from Fluo3 fluorescence, pHi from BCECF fluorescence, ceramide abundance utilizing antibodies and reactive oxygen species (ROS) formation from DCFDA-dependent fluorescence. A 48-hr exposure of human erythrocytes to nigericin significantly increased the percentage of annexin-V-binding cells (0.1-10 nM), significantly decreased forward scatter (0.1-1 nM), significantly decreased cytosolic pH (0.1-1 nM) and significantly increased Fluo3 fluorescence (0.1-10 nM). Nigericin (1 nM) slightly, but significantly, increased ROS, but did not significantly modify ceramide abundance. The effect of nigericin on annexin V binding was significantly blunted, but not abolished by removal of extracellular Ca(2+). The nigericin-induced increase in [Ca(2+)]i and annexin V binding was again significantly blunted but not abolished by the Na(+)/H(+) exchanger inhibitor cariporide (10 μM). Nigericin triggers eryptosis, an effect paralleled by ROS formation, in part dependent on stimulation of Ca(2+) entry, and involving the cariporide-sensitive Na(+)/H(+) exchanger.[2] Nasopharyngeal carcinoma (NPC) is prevalent in southern China, northern Africa, and Alaska. The prognosis for NPC patients at early stage is good, while it is poor for patients at late stages. Cancer stem cells (CSCs) have been proposed to be associated with tumor initiation, relapse and metastasis, and the poor prognosis of NPC likely results from residual CSCs after therapy. Study on the therapy targeting CSCs in NPC remains poor, though it received intensive attentions in other cancers. Here, we used NPC cell lines with high and low proportion of CSCs as models to explore the effect of nigericin, an antibiotic, on CSCs. We found that nigericin could selectively target CSCs and sensitize CSCs in NPC to the widely used clinical drug cisplatin both in vitro and in vivo. Moreover, downregulation of the polycomb group protein Bmi-1 may contribute to the inhibitory effect of nigericin on CSCs. Furthermore, by using the in vitro NPC cell models, we found that nigericin could significantly decrease the migration and invasion abilities, which are known to be associated with CSCs. Taken together, our results suggest that nigericin can selectively target CSCs in NPC, which could be a candidate CSCs targeting drug for clinical evaluation.[3] Aim: To evaluate the effect of nigericin on colorectal cancer and to explore its possible mechanism. Methods: The human colorectal cancer (CRC) cell lines HT29 and SW480 were treated with nigericin or oxaliplatin under the conditions specified. Cell viability assay and invasion and metastasis assay were performed to evaluate the effect of nigericin on CRC cells. Sphere-forming assay and soft agar colony-forming assay were implemented to assess the action of nigericin on the cancer stem cell properties of CRC cells undergone epithelial-mesenchymal transition (EMT). Results: Compared with oxaliplatin, nigericin showed more toxicity for the HT29 cell line (IC50, 12.92 ± 0.25 μmol vs 37.68 ± 0.34 μmol). A similar result was also obtained with the SW116 cell line (IC50, 15.86 ± 0.18 μmol vs 41.02 ± 0.23 μmol). A Boyden chamber assay indicated that a significant decrease in the number of HT29 cells migrating through polyvinylidene fluoride membrane was observed in the nigericin-treated group, relative to the vehicle-treated group [11 ± 2 cells per high-power field (HPF) vs 19.33 ± 1.52 cells per HPF, P < 0.05]. Compared to the control group, the numbers of HT29 cells invading through the Matrigel-coated membrane also decreased in the nigericin-treated group (6.66 ± 1.52 cells per HPF vs 14.66 ± 1.52 cells per HPF, P < 0.05). Nigericin also reduced the proportion of CD133+ cells from 83.57% to 63.93%, relative to the control group (P < 0.05). Nigericin decreased the number of spheres relative to the control group (0.14 ± 0.01 vs 0.35 ± 0.01, P < 0.05), while oxaliplatin increased the number of spheres relative to the control group (0.75 ± 0.02 vs 0.35 ± 0.01; P < 0.05). Nigericin also showed a decreased ability to form colonies under anchorage-independent conditions in a standard soft agar assay after 14 d in culture, relative to the control group (1.66 ± 0.57 vs 7 ± 1.15, P < 0.05), whereas the colony numbers were higher in the oxaliplatin group relative to the vehicle-treated controls (14.33 ± 0.57 vs 7 ± 1.15, P < 0.05). We further detected the expression of E-cadherin and vimentin in cells treated with nigericin and oxaliplatin. The results showed that HT29 cells treated with nigericin induced an increase in E-cadherin expression and a decrease in the vimentin expression relative to vehicle controls. In contrast, oxaliplatin downregulated the expression of E-cadherin and upregulated the expression of vimentin in HT29 cells relative to vehicle controls. Conclusion: This study demonstrated that nigericin could partly reverse the EMT process during cell invasion and metastasis. [4] Although immune checkpoint inhibitors improved the clinical outcomes of advanced triple negative breast cancer (TBNC) patients, the response rate remains relatively low. Nigericin is an antibiotic derived from Streptomyces hydrophobicus. We found that nigericin caused cell death in TNBC cell lines MDA-MB-231 and 4T1 by inducing concurrent pyroptosis and apoptosis. As nigericin facilitated cellular potassium efflux, we discovered that it caused mitochondrial dysfunction, leading to mitochondrial ROS production, as well as activation of Caspase-1/GSDMD-mediated pyroptosis and Caspase-3-mediated apoptosis in TNBC cells. Notably, nigericin-induced pyroptosis could amplify the anti-tumor immune response by enhancing the infiltration and anti-tumor effect of CD4+ and CD8+ T cells. Moreover, nigericin showed a synergistic therapeutic effect when combined with anti-PD-1 antibody in TNBC treatment. Our study reveals that nigericin may be a promising anti-tumor agent, especially in combination with immune checkpoint inhibitors for advanced TNBC treatment. [5] Multidrug-resistant (MDR) bacteria pose a significant clinical threat to human health, but the development of antibiotics cannot meet the urgent need for effective agents, especially those that can kill persisters and biofilms. Here, we reported that nigericin showed potent bactericidal activity against various clinical MDR Gram-positive bacteria, persisters and biofilms, with low frequencies of resistance development. Moreover, nigericin exhibited favorable in vivo efficacy in deep-seated mouse biofilm, murine skin and bloodstream infection models. With Staphylococcus aureus, nigericin disrupted ATP production and electron transport chain; cell death was associated with altered membrane structure and permeability. Obtaining nigericin-resistant/tolerant mutants required multiple rounds of challenge, and, cross-resistance to members of several antimicrobial classes was absent, probably due to distinct nigericin action with the GraSR two-component regulatory system. Thus, our work reveals that nigericin is a promising antibiotic candidate for the treatment of chronic or recurrent infections caused by Gram-positive bacteria.[6] |
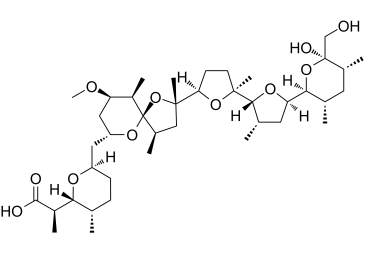
| 分子式 |
C40H68O11
|
|---|---|
| 分子量 |
746.94318
|
| 精确质量 |
746.458
|
| 元素分析 |
C, 66.27; H, 9.45; O, 24.28
|
| CAS号 |
28380-24-7
|
| 相关CAS号 |
Nigericin sodium salt;28643-80-3
|
| PubChem CID |
34230
|
| 外观&性状 |
White to off-white solid powder
|
| 密度 |
1.19g/cm3
|
| 沸点 |
779.9ºC at 760mmHg
|
| 熔点 |
245-255ºC
|
| 闪点 |
226.9ºC
|
| 折射率 |
1.543
|
| LogP |
4.37
|
| tPSA |
145.2
|
| 氢键供体(HBD)数目 |
3
|
| 氢键受体(HBA)数目 |
11
|
| 可旋转键数目(RBC) |
9
|
| 重原子数目 |
51
|
| 分子复杂度/Complexity |
1230
|
| 定义原子立体中心数目 |
19
|
| SMILES |
C[C@H]1CC[C@@H](O[C@H]1[C@@H](C)C(=O)O)C[C@@H]2C[C@H]([C@H]([C@@]3(O2)[C@@H](C[C@@](O3)(C)[C@H]4CC[C@@](O4)(C)[C@H]5[C@H](C[C@@H](O5)[C@@H]6[C@H](C[C@H]([C@@](O6)(CO)O)C)C)C)C)C)OC
|
| InChi Key |
MOYOTUKECQMGHE-PDEFJWSRSA-M
|
| InChi Code |
InChI=1S/C40H68O11.Na/c1-21-11-12-28(46-33(21)26(6)36(42)43)17-29-18-30(45-10)27(7)40(48-29)25(5)19-38(9,51-40)32-13-14-37(8,49-32)35-23(3)16-31(47-35)34-22(2)15-24(4)39(44,20-41)50-34/h21-35,41,44H,11-20H2,1-10H3,(H,42,43)/q+1/p-1/t21-,22-,23-,24+,25+,26+,27+,28+,29+,30+,31+,32+,33+,34-,35+,37-,38-,39-,40+/m0./s1
|
| 化学名 |
sodium
(R)-2-((2R,3S,6R)-6-(((2S,4R,5R,7R,9R,10R)-2-((2S,2'R,3'S,5R,5'R)-5'-((2S,3S,5R,6R)-6-hydroxy-6-(hydroxymethyl)-3,5-dimethyltetrahydro-2H-pyran-2-yl)-2,3'-dimethyloctahydro-[2,2'-bifuran]-5-yl)-9-methoxy-2,4,10-trimethyl-1,6-dioxaspiro[4.5]decan-7-yl)methyl)-3-methyltetrahydro-2H-pyran-2-yl)propanoate
|
| 别名 |
Azalomycin M; Antibiotic K178; nigericin; Azalomycin M; 28380-24-7; Helixin C; Antibiotic X-464; Antibiotic K-178; UNII-RRU6GY95IS; RRU6GY95IS; Helexin C; Antibiotic X464; Polyetherin A
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.3388 mL | 6.6940 mL | 13.3880 mL | |
| 5 mM | 0.2678 mL | 1.3388 mL | 2.6776 mL | |
| 10 mM | 0.1339 mL | 0.6694 mL | 1.3388 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。