| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 1mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| Other Sizes |
|
| 靶点 |
OX1 Receptor
|
|---|---|
| 体外研究 (In Vitro) |
在 SH-SY5Y 人多巴胺能神经母细胞瘤细胞中,食欲素 A(人、大鼠、小鼠)醋酸盐(0.1、1、10、100 nM;24 小时)以剂量依赖性方式刺激 BDNF 的表达[1]。时间依赖性地,orexin A(人、大鼠、小鼠)醋酸盐(1 nM;1、3、6、12、24 小时)会提高 SH-SY5Y 细胞中 TH、PI3K 和 BDNF 的表达[1]。
Orexin A(人、大鼠、小鼠)对 OX1R 具有高亲和力,在 [Ca2﹢]i 瞬时测定中具有 38 nM IC50 和 34 nM EC50 值 [1]。
食欲素受体的特性[1] 图2c显示了原始HFGAN72受体的推导氨基酸序列,我们现在称之为OX1受体(OX1R)。在各种类型的GPCR中,OX1R在结构上与某些神经肽受体最相似,最明显的是与Y2神经肽Y(NPY)受体(26%同一性),其次是TRH受体、胆囊收缩素A型受体和NK2神经激肽受体(分别为25%、23%和20%同一性。这与我们的假设一致,即OX1R是食欲素的受体,食欲素是另一类小调节肽。为了进一步表征它们的药理学相互作用,我们使用表达受体的转染细胞系进行了体外功能测定。模拟转染的CHO细胞没有表现出可检测到的放射性碘化[125I-Tyr17]特异性结合水平食欲素A。用含有人OX1R cDNA(CHO/OX1R)的表达载体稳定转染CHO细胞,赋予了结合[125I]食欲素-A的能力(图3A)。纳摩尔浓度的未标记的合成食欲素-A以剂量依赖的方式抑制了放射性配体结合,但未被测试的几种无关肽中的任何一种抑制,包括高达10μM的人NPY和内皮素-1(数据未显示)。根据LIGAND程序计算,置换50%的特异性放射性配体结合(IC50)所需的未标记的食欲素A浓度为20 nM(Munson和Rodbard 1980)。Orexin A还以剂量依赖的方式诱导CHO/OX1R细胞中[Ca2+]i的短暂增加(图3C),但在模拟转染的CHO细胞中未能诱导可检测到的[Ca2+]i瞬变。我们认为钙动员可能是由Gq类异三聚体G蛋白的激活引起的(Hepler等人,1994)。诱导半最大反应(EC50)所需的食欲素A的计算浓度为30 nM。我们在用稳定转染的HEK293细胞进行的放射性配体结合和[Ca2+]i瞬时测定中获得了类似的结果(数据未显示)。这些发现证实,食欲素A确实是OX1R的特异性、高亲和力激动剂。 为了进一步表征OX2R的功能,我们使用稳定转染的表达人OX2R cDNA的CHO细胞重复了竞争性放射性配体结合试验和[Ca2+]i瞬时剂量反应研究。结果表明,OX2R确实是人食欲素-B的高亲和力受体,在结合试验中IC50为36 nM,在[Ca2+]i瞬时试验中EC50为60 nM(图3B和图3D)。食欲素-A对该受体也有很高的亲和力,IC50值为38 nM,EC50值为34 nM,与食欲素-B的值相似。因此,我们得出结论,OX2R对食欲素-A和-B都是非选择性受体,而OX1R对食欲素A/Orexin A具有选择性 在辐射杂交图谱中,与人类OX1R和OX2R基因连锁最紧密的MIT标记是STS标记D1S195和D1S443,以及WI-5448和CHLC。分别为GATA74F07。这些标记之间的推断细胞遗传学位置为OX1R的1p33和OX2R的6cen(p11-q11)(准确的细胞遗传学位置通常难以从基因位于着丝粒附近的辐射杂交图谱中解释)。 |
| 体内研究 (In Vivo) |
Orexin A(人、大鼠、小鼠)醋酸盐(300 ng/小鼠;静脉注射;每天一次,持续 8 天)使纹状体多巴胺能纤维正常化,抑制纹状体中多巴胺及其代谢物的消耗,并减轻多巴胺能神经元和黑质中酪氨酸羟化酶(TH)表达的减少[1]。在 PPQ 诱导的小鼠腹部收缩范例和角叉菜胶诱导的热痛觉过敏模型中,醋酸食欲素 A(人、大鼠、小鼠)(10、30 mg/kg;静脉注射;单次)均具有镇痛特性 [2]。
食欲素 A(人、大鼠、小鼠)(3-30 mg/kg;静脉注射;测试前 5 分钟)在测试前 5 分钟给予 10 和 30 mg/kg 静脉注射时,反应潜伏期显着增加,从 24.8±2.0媒介物处理的小鼠中的时间分别为 35.0±3.7 秒和 45.7±4.5 秒[2]。在苯基对醌 (PPQ) 之前立即给予食欲素 A(人、大鼠、小鼠)(3、10 和 30 mg/kg;iv),并将载体中的第一次 PPQ 诱导的收缩潜伏期从 357.4±35.2 秒增加。在 10 mg/kg 剂量下治疗小鼠至 500.3±31.2 秒,在 30 mg/kg 剂量下治疗小鼠至 594.5±5.5 秒[2]。 动物模型:雌性小鼠(小鼠角叉菜胶诱导的热痛觉过敏试验)[2] 剂量:3、10和30 mg/kg 给药方式:静脉注射; 5 分钟pre-test 预测试结果:在 10 和 30 mg/kg 剂量下显着增加反应潜伏期。 |
| 酶活实验 |
放射性配体结合分析[1]
在Na125I(2000 Ci/mmol)存在下,通过氯胺-T氧化在Tyr17处标记合成的人Orexin A,并通过C18反相HPLC纯化单碘化肽,如所述(Takigawa等人,1995)。将表达人OX1R或OX2R的稳定转染CHO细胞系分别以每孔3×105个细胞的密度接种到12孔板上。过夜培养后,丢弃培养基,将细胞在20°C下与含有10-10M[125I]食欲素A和指定浓度未标记竞争对手的结合缓冲液(HEPES缓冲盐水/0.5%牛血清白蛋白)一起孵育90分钟。然后用冰冷的磷酸盐缓冲盐水洗涤细胞三次,在0.1 N NaOH中裂解,用γ计数器测定细胞结合的放射性。 原位杂交[1] 如上所述,产生编码前食欲素Gln33-Ser128的大鼠cDNA的0.29kb片段,并将其亚克隆到pBluescript II SK(+)载体中。在35S-CTP 存在的情况下,使用Maxiscript试剂盒 分别用T7和T3 RNA聚合酶产生有义和反义核糖探针。如所述对成年大鼠脑切片进行原位杂交(Benjamin等人,1997)。 |
| 细胞实验 |
蛋白质印迹分析[1]
细胞类型: SH-SY5Y 细胞 测试浓度: 0.1、1、10、100 nM 孵育时间:24小时 实验结果:以剂量依赖性方式增加PI3K和TH的表达。 1 和 10 nM 剂量可显着诱导 BDNF 表达。 蛋白质印迹分析[1] 细胞类型: SH-SY5Y 细胞 测试浓度: 1 nM 孵育时间:1、3、6、12、24 h 实验结果:3 h后PI3K表达量迅速增加72.6%,维持在较高水平接下来的24小时内的水平。 BDNF蛋白水平升高,升高率为44.8%,TH蛋白水平在12 h时急剧升高48.5%。 细胞内钙瞬时测定[1] 如前所述,表达孤儿GPCR的稳定转染HEK293细胞在悬浮液中装载Fura-2 AM,并用CAF-110型细胞内离子分析仪在500μl比色皿中监测激动剂诱发的[Ca2+]i瞬变。对于体外药理学特征(图3),使用稳定转染的表达人OX1R或OX2R的CHO细胞进行相同的程序。 免疫组织化学[1] 通过用合成的食欲素A[14-33]、CRLYELLHGAGNHAGILTL酰胺免疫兔子,用3-马来酰亚胺基苯甲酸N-羟基琥珀酰亚胺酯与钥匙孔血蓝蛋白结合,在兔子体内产生抗食欲素-A抗血清。抗血清在Orexin A偶联的Sepharose CL-4B柱上进行亲和纯化,并用于免疫组织化学。将雄性Sprague-Dawley大鼠(约300 g)麻醉,并通过左心室用磷酸缓冲盐水(PBS)灌注。取出大脑,直接嵌入OCT化合物中,并在液氮中冷冻。低温恒温器切片(15μm)被切割并安装在硅烷涂层玻璃侧面。将切片用0.1M磷酸盐缓冲液(pH 7.2)中的4%多聚甲醛后固定1小时,并在PBS中洗涤三次。将切片与PBS中的1%牛血清白蛋白孵育1小时,然后在室温下与同一溶液中的亲和纯化抗血清孵育1小时。在PBS中洗涤三次后,将切片与FITC偶联的山羊抗兔IgG抗体在室温下孵育1小时。然后将载玻片在PBS中洗涤三次,并在荧光显微镜下检查。 |
| 动物实验 |
Animal/Disease Models: Male C57BL/6 mice (10weeks old; 22-26 g; MPTP-Induced Mouse Model of PD)[1].
Doses: 300 ng/ mouse Route of Administration: Intracerebroventricular injection; single daily for 8 days Experimental Results: Reversed MPTP-induced motor impairments via OX1R and increased the protein expression of BDNF in nigral dopaminergic neurons. Improved MPTP-induced impairments in spatial Learning and memory and protected dopaminergic neurons against MPTP- induced neurotoxicity. Attenuated the reduction of dopaminergic neurons in the substantia nigra and restored the reduction of dopaminergic fibers in the striatum. Animal/Disease Models: Female ICR mice (17-28 g; carrageenan-induced thermal hyperalgesia model)[2]. Doses: 10 , 30 mg/kg Route of Administration: intravenous (iv) injection; single; 5 min pre-test Experimental Results: Increased paw withdrawal latency to the thermal stimulus back to baseline levels. Animal/Disease Models: Male ICR mice (17-20 g; phenyl-p-quinone ( PPQ)-induced mouse abdominal constriction model)[2]. Doses: 3, 10, 30 mg/kg A Mouse abdominal constriction test [2] Male mice were randomly assigned into groups of ten and placed in Perspex cages for approximately 10 min for habituation. They were dosed with vehicle or Orexin A (1, 3, 10 and 30 mg/kg i.v.) immediately before administration of phenyl-p-quinone (PPQ, 0.25 mg/kg i.p.). The latency to first constriction was measured, after which they were immediately killed by cervical dislocation. A cut-off time of 600 s was used and any mice not responding in this time were killed once this time had elapsed. Mouse hotplate test [2] Male mice were randomly assigned to five groups of ten and given vehicle or orexin (1, 3, 10 or 30 mg/kg i.v.). Five minutes later they were placed on the hotplate maintained at 50°C and the latency to response was measured (licking or fanning of fore- or hindpaws). At this point mice were immediately removed from the thermal stimulus and killed by cervical dislocation. All dosing and testing were done blind. A cut-off time of 60 s was used to prevent tissue damage and any animal not responding within this time was removed from the thermal stimulus and killed as above. In a separate experiment, morphine (1.25, 2.5 or 5 mg/kg s.c.) was given 30 min pre-test and the experiment was repeated as above. In another experiment, Orexin A (30 mg/kg, i.v.) was dosed 15, 30 and 60 min pre-test and the latency to response was measured as above. In a separate experiment, a similar protocol was followed using a hotplate temperature of 55°C and a cut-off time of 40 s. The Orexin A receptor antagonist SB-284422, the 5-HT2B/2C receptor antagonist SB-228357 (1, 3, 10 and 30 mg/kg i.p.) and morphine (2.5, 5 and 10 mg/kg s.c.) were also given 30 min pre-test and latencies were measured as above. Mouse carrageenan-induced thermal hyperalgesia [2] Female mice were placed in the test apparatus for 10 min once a day for 3 days for habituation. Withdrawal latencies of the left and right hindfeet to a focused thermal stimulus (Hargreaves et al., 1988) were measured on a further 2 days and the last measurement was taken as a baseline. The intensity of the thermal stimulus was set to give a baseline withdrawal latency of approximately 9 s. The range for the experimental groups reported here was 10.3–10.5 s for test 1 and 8.9–9.3 s for test 2 for the orexin experiments, and 8.4–9.2 s for the morphine experiments. Carrageenan (2% w/v in saline, 0.25 ml) was injected into the plantar surface of the left foot and withdrawal latencies were measured 240 min post-carrageenan. Orexin A was given at 10 and 30 mg/kg i.v., and in a separate experiment at 3, 10 and 30 mg/kg, 5 min pre-plantar test. In another experiment, morphine (2.5, 5 and 10 mg/kg s.c.) was tested 30 min pre-plantar test. The orexin-A receptor antagonist SB-284422 and the 5-HT2B/2C receptor antagonist SB-228357 (1, 3, 10 and 30 mg/kg i.p.) were also given 30 min pre-test and latencies were measured as above. Rat ICV studies: hotplate test [2] Sprague–Dawley rats (Charles River, 250–300 g at the time of surgery) were implanted under anaesthesia (Domitor® (medetomidine HCl, 0.4 mg/kg s.c), Sublimaze® (fentanyl, 0.45 mg/kg i.p.) with an indwelling cannula directed towards either the left or right lateral ventricle (co-ordinates: ±1.6 mm from midline, 0.8 mm caudal from bregma, −4.1 mm from skull surface, incisor bar at −3.2 mm below zero) (Paxinos and Watson, 1986). Anaesthesia was reversed by Antisedan® (atipamezole HCl, 2.5 mg/kg s.c.) and post-operative analgesia was provided by Nubain® (nalbuphine HCl, 2 mg/kg s.c., Du Pont Pharmaceuticals, Letchworth Garden City, UK). All rats were singly housed after surgery and for the duration of the study to avoid damage to the guide and dummy cannulae. Rats were handled frequently during the studies to prevent the development of hyperactivity and aggression. Following 7 days recovery from surgery, during which rats were fed soaked food pellets, weighed and health-checked daily by a veterinary technician, correct cannula placement was verified by an intense drinking response to angiotensin II (100 ng ICV) (Simpson et al., 1978). At least 7 days later Orexin A (3, 10 and 30 μg/rat) was given ICV in a volume of 5 μl over 60 s. The injection needle (extending 1 mm from the end of the guide cannula) was left in place for a further 90 s to allow complete diffusion of the drug. Five minutes later rats were placed on the hotplate maintained at 50°C and the latency to response was measured (licking or fanning of fore- or hindpaws). At this point rats were immediately removed from the thermal stimulus and killed by cervical dislocation. All dosing and testing were done blind. A cut-off time of 60 s was used to prevent tissue damage and any animal not responding within this time was removed from the thermal stimulus and killed as above. Orexin A pharmacokinetics and brain penetration studies in the rat and mouse [2] The pharmacokinetics, oral bioavailability and steady-state brain penetration of Orexin A were investigated in the conscious rat. The steady-state brain penetration of orexin-A was investigated in the conscious mouse. Chronic cannulation of the jugular vein for blood sampling (both species) and the vena cava for drug administration (via cannulation of the femoral vein in the rat and via laparotomy in the mouse) was performed using methods described by Griffiths et al. (1996). The pharmacokinetic and oral bioavailability study in the rat (n=3) was conducted as a crossover design on two study days 3 days apart. On study day 1, Orexin A (6 mg/ml dissolved in normal saline) was infused at a target dose of 30 mg/kg administered over 30 min. On study day 2, orexin-A (3 mg/ml dissolved in purified water) was administered orally at a target dose of 30 mg/kg. Serial blood samples (50 μl) were collected over 10 h on both study days, diluted with an equal volume of water, mixed and then extracted immediately (see below). The brain penetration of Orexin A was evaluated under steady-state conditions after intravenous infusion of orexin-A to rats and mice (n=3, both species). Orexin A (2 mg/ml dissolved in normal saline) was infused at a target dose level of 10 mg/kg per h for 2 h. Serial blood samples (50 μl rats, 25 μl mice, prepared as described above) were obtained during the last hour of the infusion to establish steady-state blood concentrations and at 2 h the animals were killed, exsanguinated and had their brains removed. Whole brains were diluted with two volumes of water, homogenized and then extracted immediately (see below). Intracerebroventricular Administration of Orexins [1] Male Wistar rats (180–200 g on arrival) were housed under controlled lighting (12 hr light-dark cycle) and temperature (22°C) conditions. Food (standard chow pellets) and water were available ad libitum. Rats (200–220 g) were anesthetized with pentobarbital (50 mg/kg i.p.), positioned in a Koph Model 900 stereotaxic frame, and implanted with a guide cannula into the left lateral ventricle under sterile conditions using a MEDIBIO Optical Brain Tracer (Ikeda and Matsushita 1980). The coordinates used to map the correct positioning of the implants were: 6.1 mm anterior to the lambda, 1.5 mm lateral from the midline, and ∼3.4 mm (guided by MEDIBIO) ventral to the skull surface, with the incisor bar set 3.3 mm below the interauricular line. Rats were then housed singly under the same conditions as above for a recovery period of at least 7 days, and body weights were monitored daily for the duration of the study. After recovery from surgery, rats were transferred to grid-floor cages and fed with powdered chow so that food intake measurements could be made. The rats were acclimated to the new environment at least for 1 day. The position of the cannula was verified by central administration of human NPY (3 nmol in sterile water); for a positive test, at least 8 g of food was eaten over a 4 hr period postinjection. Only positively testing animals (n = 8–10) were used. The studies were conducted according to a multidose, crossover design, with the order of dosing determined using the Latin square principle, leaving at least one rest day between administrations. All doses were delivered in a volume of 5 μl in sterile water over 30 s, and the injector remained in position for a further 30 s to ensure complete dispersal of the peptide. All intracerebroventricular administrations began at 2 h into light cycle, and food intake was measured at 1, 2, and 4 h intervals. All peptides were dissolved in sterile water, initially at 6 mM, and diluted in water as needed. Water alone was used for the vehicle control. |
| 药代性质 (ADME/PK) |
Short half-life and lack of brain penetration of orexin-A [2]
Non-compartmental pharmacokinetic parameters for orexin-A following intravenous and oral administration to the rat are shown in Table 2. Following intravenous administration of orexin-A to rats to a target dose of 30 mg/kg, the compound was slowly cleared (CLb, 17 ml/min per kg) and had a small volume of distribution (<0.2 l/kg, suggesting minimal tissue distribution) resulting in a short terminal half-life of less than 0.2 h. Following oral administration of orexin-A, all blood concentrations were non-detectable and therefore oral bioavailability in the rat was effectively zero. The relatively short duration of action (<30 min) is mirrored by the pharmacokinetic profile, with a terminal half-life of 12 min for orexin-A in rat. Moreover, orexin-A has similar efficacy to morphine (%MPE=23.9–82.1%), with a %MPE of between 29.4 and 136.2%, depending on the type of test, dose used and the species involved. Importantly, its analgesic efficacy does not appear to involve activation of endogenous opiate systems as shown by the lack of effect of naloxone on the orexin-A-mediated responses. |
| 参考文献 | |
| 其他信息 |
Neuropeptide hormones that play a role in regulating a variety of behavioral and physiological processes in response to motivational stimuli.
The hypothalamus plays a central role in the integrated control of feeding and energy homeostasis. We have identified two novel neuropeptides, both derived from the same precursor by proteolytic processing, that bind and activate two closely related (previously) orphan G protein-coupled receptors. These peptides, termed orexin-A and -B, have no significant structural similarities to known families of regulatory peptides. prepro-orexin mRNA and immunoreactive orexin-A are localized in neurons within and around the lateral and posterior hypothalamus in the adult rat brain. When administered centrally to rats, these peptides stimulate food consumption. prepro-orexin mRNA level is up-regulated upon fasting, suggesting a physiological role for the peptides as mediators in the central feedback mechanism that regulates feeding behavior.[1] The hypothalamic peptide orexin-A and the orexin-1 receptor are localized in areas of the brain and spinal cord associated with nociceptive processing. In the present study, localization was confirmed in the spinal cord and demonstrated in the dorsal root ganglion for both orexin-A and the orexin-1 receptor. The link with nociception was extended when orexin-A was shown to be analgesic when given i.v. but not s.c. in mouse and rat models of nociception and hyperalgesia. The efficacy of orexin-A was similar to that of morphine in the 50 degrees C hotplate test and the carrageenan-induced thermal hyperalgesia test. However, involvement of the opiate system in these effects was ruled out as they were blocked by the orexin-1 receptor antagonist SB-334867 but not naloxone. Orexin-1 receptor antagonists had no effect in acute nociceptive tests but under particular inflammatory conditions were pro-hyperalgesic, suggesting a tonic inhibitory orexin drive in these circumstances. These data demonstrate that the orexinergic system has a potential role in the modulation of nociceptive transmission.[2] |
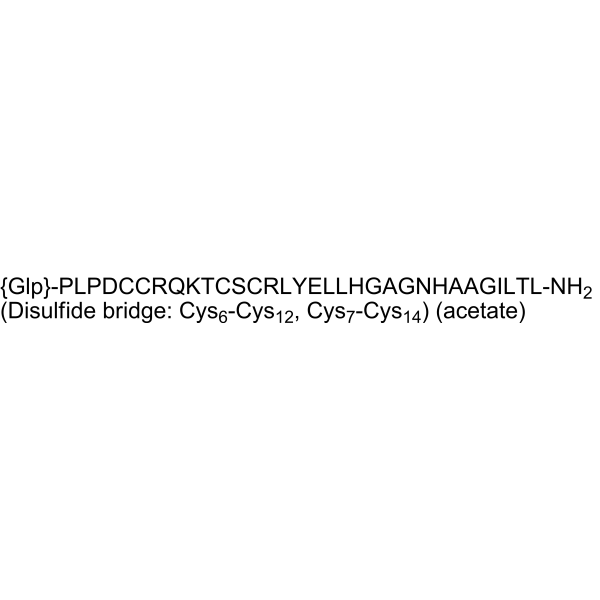
| 分子式 |
C152H243N47O44S4.XC2H4O2
|
|---|---|
| 分子量 |
3561.10 (free base)
|
| 相关CAS号 |
Orexin A (human, rat, mouse);205640-90-0;Orexin A (human, rat, mouse) (TFA)
|
| 外观&性状 |
Solid powder
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: (1). 本产品在运输和储存过程中需避光。 (2). 请将本产品存放在密封且受保护的环境中(例如氮气保护),避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
H2O :≥ 50 mg/mL
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。