| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 100g |
|
||
| 500g |
|
||
| Other Sizes |
| 体外研究 (In Vitro) |
对于生命科学相关的研究,碳酸钠(99.5%)是一种生化试剂,可用作有机物质或生物材料。
|
|---|---|
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Elimination: Renal; carbon dioxide formed is eliminated via lungs. Excess sodium bicarbonate is emptied rapidly into small intestine where it is absorbed. It is eliminated principally in the urine and effectively alkalizes it. ... /It/ is completely absorbed orally and usually is excreted within 3-4 hr. Oral: Onset of action: Rapid; Duration: 8-10 minutes. I.V: Onset of action: 15 minutes; duration: 1-2 hours. For more Absorption, Distribution and Excretion (Complete) data for Sodium bicarbonate (8 total), please visit the HSDB record page. Metabolism / Metabolites Excessive use can cause systemic alkalosis /in animals/, but body usually splits bicarbonate radical into water and carbon dioxide ... Sodium bicarbonate rapidly reacts with hydrochloric acid to form sodium chloride, carbon dioxide, and water; excess bicarbonate that does not neutralize gastric acid rapidly empties into the small intestine and is absorbed. |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
IDENTIFICATION AND USE: Sodium bicarbonate is a white crystalline powder or granules. It is used in manufacturing many sodium salts, as a source of carbon dioxide, ingredient of baking powder, and effervescent salts and beverages, in fire extinguishers, cleaning compounds. It is also used in analytical chemistry for pH adjustment. It is used in aquaculture as an anesthetic for fish in the United States. Sodium bicarbonate is used in the treatment of metabolic acidosis associated with many conditions. It is also used in veterinary medicine. HUMAN STUDIES: Risks of acute and chronic oral bicarbonate ingestion include metabolic alkalosis, hypernatremia, hypertension, gastric rupture, hyporeninemia, hypokalemia, hypochloremia, intravascular volume depletion, and urinary alkalinization. Abrupt cessation of chronic excessive bicarbonate ingestion may result in hyperkalemia, hypoaldosteronism, volume contraction, and disruption of calcium and phosphorus metabolism. The anticoagulant effects of sodium bicarbonate was investigated in fresh human whole blood obtained from normal healthy volunteers. Prothrombin and thrombin clotting time determination indicated that bicarbonate can interfere with the clotting process. ANIMAL STUDIES: Sodium bicarbonate was irritating to the rabbit eye. It was slightly irritating when tested on the skin of rabbits. Sodium bicarbonate was evaluated for teratological effects, maximum dose levels were as follows: mice, 580 mg/kg; rats, 340 mg/kg; and rabbits, 330 mg/kg. No effects were found in any of these species. The mutagenicity of sodium bicarbonate was assessed in Salmonella/microsome assays using Salmonella typhimurium strains TA 92, TA 94, TA 98, TA 100, TA 1535 and TA 1537 with metabolic activation, and it was negative. ECOTOXICITY STUDIES: Several histological anomalies, including increased incidence of necrotic cells, suggested that fish were adversely affected as a result of exposure to >450 mg NaHCO3/L. Toxicity Data LC (rat) = > 900 mg/m3 Interactions Concurrent use /of citrates/ with sodium bicarbonate may promote the development of calcium stones in patients with uric acid stones, due to sodium ion opposition to the hypocalciuric effect of the alkaline load; may also cause hypernatremia. Chronic administration of bicarbonate with milk or calcium may cause the milk-alkali syndrome which is characterized by hypercalcemia, renal insufficiency, metabolic alkalosis, nausea, vomiting, headache, mental confusion, and anorexia. During the acute phase of the milk-alkali syndrome, the condition is reversible when the calcium and alkali are withdrawn. However, in patients with chronic milk-alkali syndrome, reduced renal function may persist even after calcium and alkali are discontinued. Patients with a salt-losing nephropathy have an increased risk of developing the milk-alkali syndrome. Concurrent use /of anticholinergics or other medications with anticholinergic action/ with sodium bicarbonate may decrease absorption, reducing the effectiveness of the anticholinergic; doses of these medications should be spaced 1 hour apart from doses of sodium bicarbonate; also, urinary excretion may be delayed by alkalinization of the urine, thus potentiating the side effects of the anticholinergic Antacids may alkalinize the urine and counteract the effect of urinary acidifiers /such as ammonium chloride, ascorbic acid and potassium or sodium phosphates/; frequent use of antacids, especially in high doses, is best avoided by patients receiving therapy to acidify the urine. For more Interactions (Complete) data for Sodium bicarbonate (17 total), please visit the HSDB record page. Non-Human Toxicity Values LD50 Rat oral 4,220 mg/kg LD50 Mouse oral 3360 mg/kg |
| 其他信息 |
Sodium bicarbonate appears as odorless white crystalline powder or lumps. Slightly alkaline (bitter) taste. pH (of freshly prepared 0.1 molar aqueous solution): 8.3 at 77 °F. pH (of saturated solution): 8-9. Non-toxic.
Sodium hydrogencarbonate is an organic sodium salt and a one-carbon compound. It has a role as an antacid and a food anticaking agent. It contains a hydrogencarbonate. Sodium bicarbonate is a white, crystalline powder that is commonly used as a pH buffering agent, an electrolyte replenisher, systemic alkalizer and in topical cleansing solutions. Sodium Bicarbonate is the monosodium salt of carbonic acid with alkalinizing and electrolyte replacement properties. Upon dissociation, sodium bicarbonate forms sodium and bicarbonate ions. Ion formation increases plasma bicarbonate and buffers excess hydrogen ion concentration, resulting in raised blood pH. Soda is a beverage consisting of carbonated water and a flavoring. A white, crystalline powder that is commonly used as a pH buffering agent, an electrolyte replenisher, systemic alkalizer and in topical cleansing solutions. See also: Bicarbonate Ion (has active moiety); Sodium Cation (has active moiety); Omeprazole; Sodium Bicarbonate (component of) ... View More ... Drug Indication Sodium bicarbonate is used for the treatment of metabolic acidosis which may occur in severe renal disease, uncontrolled diabetes, circulatory insufficiency due to shock or severe dehydration, extracorporeal circulation of blood, cardiac arrest and severe primary lactic acidosis. Also is indicated in severe diarrhea which is often accompanied by a significant loss of bicarbonate. Further indicated in the treatment of certain drug intoxications, including barbiturates (where dissociation of the barbiturateprotein complex is desired), in poisoning by salicylates or methyl alcohol and in hemolytic reactions requiring alkalinization of the urine to diminish nephrotoxicity of blood pigments. Mechanism of Action Sodium bicarbonate is a systemic alkalizer, which increases plasma bicarbonate, buffers excess hydrogen ion concentration, and raises blood pH, thereby reversing the clinical manifestations of acidosis. It is also a urinary alkalizer, increasing the excretion of free bicarbonate ions in the urine, thus effectively raising the urinary pH. By maintaining an alkaline urine, the actual dissolution of uric acid stones may be accomplished. Sodium bicarbonate acts as an antacid and reacts chemically to neutralize or buffer existing quantities of stomach acid but has no direct effect on its output. This action results in increased pH value of stomach contents, thus providing relief of hyperacidity symptoms. [PharmGKB] Therapeutic Uses Sodium bicarbonate is used in the treatment of metabolic acidosis associated with many conditions including severe renal disease (e.g., renal tubular acidosis), uncontrolled diabetes (ketoacidosis), extracorporeal circulation of the blood, cardiac arrest, circulatory insufficiency caused by shock or severe dehydration, ureterosigmoidostomy, lactic acidosis, alcoholic ketoacidosis, use of carbonic anhydrase inhibitors, and ammonium chloride administration. In metabolic acidosis, the principal disturbance is a loss of proton acceptors (e.g., loss of bicarbonate during severe diarrhea) or accumulation of an acid load (e.g., ketoacidosis, lactic acidosis, renal tubular acidosis). The specific role of sodium bicarbonate therapy in the treatment of diabetic ketoacidosis has not been established. Because correction of the underlying metabolic disorder generally results in correction of acid-base abnormalities and because of the potential risks of sodium bicarbonate therapy in the treatment of this disorder, administration of sodium bicarbonate is generally reserved for the treatment of severe acidosis (e.g., arterial pH less than 7-7.15 or serum bicarbonate concentration of 8 mEq/L or less). Rapid correction of acidosis with sodium bicarbonate in patients with diabetic ketoacidosis may cause hypokalemia, paradoxical acidosis in cerebrospinal fluid (CSF) since carbon dioxide diffuses more rapidly into CSF than does bicarbonate, and lactic acidosis since increased pH increases hemoglobin-oxygen affinity which, when combined with erythrocyte 2,3-diphosphoglycerate (2,3-DPG) deficiency in these patients, results in peripheral tissue hypoxia. However, the benefits and risks of sodium bicarbonate therapy in ketoacidosis have not been fully determined, and additional controlled studies of the safety and efficacy of the drug are necessary. Generally, when sodium bicarbonate is used in the treatment of diabetic ketoacidosis, the acidosis should only be partially corrected (e.g., to an arterial pH of about 7.2) to avoid rebound metabolic alkalosis as ketones are metabolized. Oral sodium bicarbonate is indicated to reduce uric acid crystallization as an adjuvant to uricosuric medication in gout. /Included in US product labeling/ Parenteral sodium bicarbonate is indicated in the treatment of certain drug intoxications, including barbiturates, and in poisoning by salicylates or methyl alcohol. /Included in US product labeling/ For more Therapeutic Uses (Complete) data for Sodium bicarbonate (29 total), please visit the HSDB record page. Drug Warnings Sodium bicarbonate is generally contraindicated in patients with metabolic or respiratory alkalosis, in patients with hypocalcemia in whom alkalosis may induce tetany, in patients with excessive chloride loss from vomiting or continuous GI suctioning, and in patients at risk of developing diuretic-induced hypochloremic alkalosis. Sodium bicarbonate should not be used orally as an antidote in the treatment of acute ingestion of strong mineral acids, since carbon dioxide gas forms during neutralization and may cause gastric distention and possible rupture. Sodium bicarbonate should be used with extreme caution in patients with congestive heart failure or other edematous or sodium-retaining conditions; in patients with renal insufficiency, especially those with severe insufficiency such as oliguria or anuria; and in patients receiving corticosteroids or corticotropin, since each gram of sodium bicarbonate contains about 12 mEq of sodium. IV administration of sodium bicarbonate may cause fluid and/or solute overload resulting in dilution of serum electrolytes, overhydration, congestive conditions, or pulmonary edema. The risk of dilutional conditions is inversely proportional to the electrolyte concentration administered, and the risk of solute overload and resultant congestive conditions with peripheral and/or pulmonary edema is directly proportional to the electrolyte concentration administered. Gastric distention and flatulence may occur when sodium bicarbonate is administered orally. Inadvertent extravasation of hypertonic solutions of sodium bicarbonate has reportedly caused chemical cellulitis because of their alkalinity, subsequently resulting in tissue necrosis, ulceration, and/or sloughing at the site of injection. Predisposing factors /contributing to milk-alkali syndrome/ are preexisting hypertension, sarcoidosis, dehydration and electrolyte imbalance due to vomiting or aspiration of gastric contents with inadequate iv fluid replacement, and renal dysfunction caused by primary renal disease. For more Drug Warnings (Complete) data for Sodium bicarbonate (14 total), please visit the HSDB record page. Pharmacodynamics Intravenous sodium bicarbonate therapy increases plasma bicarbonate, buffers excess hydrogen ion concentration, raises blood pH and reverses the clinical manifestations of acidosis. |
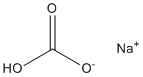
| 分子式 |
CHNAO3
|
|---|---|
| 分子量 |
84.0
|
| 精确质量 |
83.982
|
| CAS号 |
144-55-8
|
| 相关CAS号 |
7542-12-3 (unspecified hydrochloride salt)
|
| PubChem CID |
516892
|
| 外观&性状 |
White to off-white solid powder
|
| 密度 |
2.16 g/mL at 25 °C(lit.)
|
| 沸点 |
851°C
|
| 熔点 |
270 ºC
|
| 闪点 |
169.8ºC
|
| 蒸汽压 |
2.58E-05mmHg at 25°C
|
| 折射率 |
1.500
|
| tPSA |
60.36
|
| 氢键供体(HBD)数目 |
1
|
| 氢键受体(HBA)数目 |
3
|
| 可旋转键数目(RBC) |
0
|
| 重原子数目 |
5
|
| 分子复杂度/Complexity |
33.9
|
| 定义原子立体中心数目 |
0
|
| InChi Key |
UIIMBOGNXHQVGW-UHFFFAOYSA-M
|
| InChi Code |
InChI=1S/CH2O3.Na/c2-1(3)4;/h(H2,2,3,4);/q;+1/p-1
|
| 化学名 |
sodium;hydrogen carbonate
|
| 别名 |
Soda Mint Sodium hydrocarbonateSodium bicarbonate NSC-134031 NSC 134031 NSC134031Bicarbonate of soda
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
H2O : ~50 mg/mL (~595.17 mM)
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 11.9048 mL | 59.5238 mL | 119.0476 mL | |
| 5 mM | 2.3810 mL | 11.9048 mL | 23.8095 mL | |
| 10 mM | 1.1905 mL | 5.9524 mL | 11.9048 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
Neurovascular Regulation During Exercise in Humans With Chronic Kidney Disease: Sympatholysis in CKD
CTID: NCT05928936
Phase: Phase 2 Status: Recruiting
Date: 2024-09-19