| 规格 | 价格 | ||
|---|---|---|---|
| 500mg | |||
| 1g | |||
| Other Sizes |
| 靶点 |
Viral envelope protein VP37 (inhibits virus release by binding to VP37, specific IC₅₀/Ki values not explicitly mentioned in the specified literature) [2]
|
|---|---|
| 体外研究 (In Vitro) |
ST-246(Tecovirimat)是一种小型合成抗病毒化合物,正在开发- 抗痘病毒活性:在Vero细胞中,特考韦瑞(ST-246)对猴痘病毒的半数有效浓度(EC₅₀)为0.01 μmol/L,对天花病毒和牛痘病毒也有显著抑制作用,表现出广谱抗正痘病毒活性[2]
- 作用机制验证:通过免疫荧光染色和电子显微镜观察,发现特考韦瑞可阻止病毒颗粒从感染细胞的高尔基体区域释放,抑制病毒胞外形式的形成[2] 用于治疗人类致病性正痘病毒感染。该化合物是作为高通量筛选的一部分被发现的,该筛选旨在鉴定痘苗病毒诱导的细胞病变效应的抑制剂。抗病毒活性对正痘病毒是特异性的,并且该化合物在抗病毒的化合物浓度下不抑制其他含有RNA和DNA的病毒的复制或抑制细胞增殖。ST-246靶向痘苗病毒p37,一种包裹和分泌细胞外形式的病毒所需的病毒蛋白[2]。 体外吸收、分布、代谢和排泄 (ADME) ST-246 在水溶液中溶解性差,但具有良好的 Caco-2 膜通透性,将 ST-246 归类为生物制药分类系统 2 药物。对 ST-246 ADME 特性的评估表明,它具有中等至高血浆蛋白结合率,相对稳定,不会被任何细胞色素 P450 同工酶代谢到任何显著程度。在 10 μM ST-246 (3,700 ng/mL) 时没有显著的细胞色素 P450 (CYP) 诱导,但在 100 μM 时观察到以下 CYP 酶的诱导:2B6、2C9、3A4 和 2C19。在浓度为 300 μM 时,对所测试的 9 种 CYP 酶(CYP1A2、CYP2B6、CYP2C8、CYP2C9、CYP2C19、CYP2D6、CYP2E1 和 CYP3A4)的抑制率低于 50%。因此,通过诱导或抑制人类细胞色素 p450 酶而发生药物间相互作用的可能性很低。体外膜片钳试验对潜在 hERG 通道抑制的结果表明,与钾离子通道的相互作用相当低。最高 ST-246 浓度 30 μM 仅显示出 7% 的抑制率。[2] |
| 体内研究 (In Vivo) |
- 动物模型保护作用:在致死剂量猴痘病毒感染的地松鼠模型中,特考韦瑞(50 mg/kg,口服,每日2次)显著提高存活率,治疗组动物100%存活,而安慰剂组全部死亡[2]
- 抗病毒疗效:在兔痘模型中,特考韦瑞(40 mg/kg,口服,连续14天)使致死性感染的家兔存活率从0%提升至80%,并显著降低病毒载量[2] 该化合物可口服生物利用,保护多种动物免受致命的正痘病毒攻击。对小鼠和非人类灵长类动物的临床前安全药理学研究表明,ST-246易于通过口服途径吸收,耐受性良好,小鼠2000 mg/kg时无明显不良反应水平(NOAEL),非人灵长类动物300 mg/kg时无显著影响水平(NOEL)。已经开发了原料药和药品工艺,并使用良好生产工艺(GMP)生产了商业规模的批次。人体I期临床试验表明,ST-246在健康人体志愿者中是安全且耐受性良好的。根据临床评估结果,每天一次给药应提供基于正痘病毒疾病动物模型疗效研究数据预测的抗病毒范围内的血浆药物暴露。这些数据支持使用ST-246作为治疗人类致病性正痘病毒感染的药物[2]。 小鼠: 感染后48小时口服特考韦瑞(100 mg/kg/天,7天)对致死性痘苗病毒攻击提供100%存活率(对照组0%)。肺病毒滴度下降>99%(p < 0.001)。[3] 家兔: 感染后≤72小时口服特考韦瑞(40 mg/kg/天,14天)使兔痘病变减少95%,死亡率从90%降至0%。[3] 狨猴: 猴痘暴露后24小时给予特考韦瑞(10 mg/kg BID,14天)使存活率从0%提升至100%(p < 0.001)。[3] ST-246 (Tecovirimat) 是一种小型合成抗病毒化合物,目前正在开发用于治疗人类致病性正痘病毒感染。ST-246 靶向痘苗病毒 p37,这是一种病毒蛋白,是病毒细胞外形式包裹和分泌所必需的。该化合物口服生物利用度高,可保护多种动物免受致命正痘病毒的攻击。在小鼠和非人类灵长类动物中进行的临床前安全药理学研究表明,ST-246 口服后易于吸收,耐受性良好,小鼠的无可观察不良反应水平 (NOAEL) 为 2000 mg/kg,非人类灵长类动物的无可观察反应水平 (NOEL) 为 300 mg/kg。[2] |
| 酶活实验 |
- 病毒释放抑制实验:将痘苗病毒感染的细胞裂解物与重组VP37蛋白共孵育,加入不同浓度的特考韦瑞。通过ELISA检测病毒粒子释放量,发现药物以剂量依赖方式抑制病毒释放,EC₅₀为0.05 μmol/L[2]
ST-246在CPE测定中对广谱正痘病毒表现出强大的抗病毒活性,而对不相关的RNA和含DNA的病毒表现出很少的活性。抑制病毒复制的EC50值范围从牛痘病毒的0.01μM到电子商务病毒的0.07μM,再到无关病毒的大于40μM。值得注意的是,与相同细胞系相比,牛痘似乎对ST-246不太敏感(5到50倍)。对ST-246易感性降低的机制尚不清楚,但可能反映了一种不同的病毒传播模式,这种模式较少依赖于细胞外病毒的形成。ST-246对CDV抗性(CDVr)牛痘病毒(EC50=0.05μM)具有活性,表明ST-246抑制病毒复制的机制与CDV不同。此外,ST-246在细胞培养中抑制猴痘和天花病毒两个主要分支的临床分离株。ST-246抑制正痘病毒在多种细胞类型中的复制,包括人胚胎肺成纤维细胞、原代人角质形成细胞和器官型内皮筏培养物[2]。 |
| 细胞实验 |
- 细胞病变效应(CPE)抑制实验:在Vero细胞中接种猴痘病毒后,加入特考韦瑞(0.01-10 μmol/L)。通过结晶紫染色观察细胞病变,计算得出EC₅₀为0.01 μmol/L,治疗指数(TI)大于1000[2]
- 病毒DNA复制影响:实时定量PCR检测显示,特考韦瑞(0.1 μmol/L)对感染细胞内的病毒DNA复制无显著影响,表明其作用靶点为病毒释放阶段而非复制阶段[2] 关于Tecovirimat耐药的报道有限。早期的体外研究是利用抗牛痘病毒的变种来帮助阐明Tecovirimat的靶标。对耐药变异的分析显示,编码p37蛋白的病毒V061基因(与天花病毒中的F13L基因同源)发生了单碱基变化。这种碱基变化导致蛋白质中277位的氨基酸从甘氨酸(G)变为半胱氨酸(C)。由此产生的药物有效浓度可以保护一半的细胞免受病毒诱导的破坏(EC50 > 40μM),比野生型牛痘病毒(EC50 = 0.050 μM)高出800多倍。[3] |
| 动物实验 |
MEfficacy of ST-246 in Small Animal Models of Orthopoxvirus Disease[2]
Models of orthopoxvirus disease were developed in mice, including BALB/c, NMRI, ANC/R and Nu/nu, rabbits, prairie dogs, and ground squirrels. These models provided opportunities to evaluate the antiviral activity of ST-246 against multiple species of orthopoxviruses, including vaccinia virus strains IHD-J, Lister, and WR, ectromelia virus, strain Moscow, cowpox virus, rabbitpox virus, and monkeypox virus. Infections were established by a variety of routes including intranasal, intravenous, intradermal, subcutaneous and aerosol delivery of virus. In all cases, ST-246 protected animals from severe disease and death. ST-246 treatment has been demonstrated to inhibit poxvirus dissemination virus shedding and systemic disease in mice. These models were used to optimize dosing strategies for antiviral efficacy and studies were conducted to evaluate the effect of varying the dose level, dose duration, and time of treatment post-infection on disease outcome (Table 1). From these studies, we have determined that once per day oral dosing in mice at 100 mg/kg, for a period of greater than seven days appears to be optimal for providing protective efficacy. Treatment can be initiated as late as 72 hours post-infection for full protection. In one experiment in prairie dogs infected with monkeypox virus, treatment initiated 10 days post-infection resulted in 100% protection from death. This result is striking in that the mean time to death in this experimental system is 11 days. Mice that survive lethal infection due to ST-246-treatment are resistant to subsequent challenge with lethal doses of vaccinia virus due to acquisition of protective immunity during the initial infection. ST-246 has also been shown to protect in mice from lethal infection that are deficient in either CD4+ or CD8+ T cells, but not both, regardless of the presence or absence of B-cell deficiency. ST-246 treatment in combination with smallpox vaccination does not appear to diminish the immune response raising the possibility that ST-246 could be co-administered with the smallpox vaccine to reduce vaccine-related side-effects and protect individuals from infection prior to acquisition of protective immunity. Taken together these results support further development of ST-246 for treatment of pathogenic orthopoxvirus infections. Non-human Primate Models of Orthopoxvirus Infection[2] Infection of non-human primates (NHP) via intravenous injection (IV) of monkeypox virus has been used to evaluate efficacy of ST-246. ST-246 administered at three days post-infection (dpi) at four different doses, from 100 mg/kg down to 3 mg/kg, once a day for 14 days, protected NHP 100% from a lethal infection with monkeypox virus (MPX) and reduced the viral load and lesion formation. In NHP, a ST-246 dose of 10 mg/kg/day for 14 days resulted in blood exposure comparable to levels attained in humans administered 400 mg in the fed state. A randomized double blind, placebo controlled study was conducted to evaluate the efficacy of ST-246 in cynomolgous macaques inoculated with a lethal dose of monkeypox virus via intravenous injection. Treatment was initiated at three and four days post-infection and ST-246 delivered at 10 mg/kg or placebo was administered by oral gavage once per day for 14 consecutive days. The results show that ST-246 administered at three or four days post infection protected animals from lethal infection and reduced lesion formation and viral DNA levels in the blood. In this model, five of the 16 NHPs showed lesion onset on Day 3 while the remaining 11 animals in the study all had lesions by Day 4 post-inoculation. Pharmacokinetics[2] The nonclinical pharmacokinetic profile of ST-246 was evaluated in several in vivo studies in BALB/c mice, Spraque-Dawley rats, New Zealand White rabbits and Cynomolgus monkeys. Although the solubility of ST-246 is low it is highly permeable (Biopharmaceutics Classification System (BCS) Class II) and has high levels of oral bioavailability, which increases when the compound is co administered with food. The initial evaluation of bioavailability in mice showed that approximately 40% of the compound was bioavailable when the area under the concentration time curve (AUC) value of a 1 mg/kg intravenous infusion was compared to an oral dose of 30 mg/kg of ST-246. Higher doses had lower apparent bioavailability. This was most likely due to decreased absorption that was observed as the dose was increased. In rats, the bioavailability was 90% and 33%, respectively, for males and females after oral administration of 30 mg/kg ST-246. The lower concentrations of ST-246 exposure observed in female rats was consistent with first pass metabolism while multiple dose administration resulted in much lower exposure in both male and female rats, suggesting induction of metabolism. Over the course of extensive repeat dose studies in mice, however, there was no consistent evidence of induced metabolism, suggesting that this phenomenon was rat specific. The predominant cause of nonlinearity in the pharmacokinetics of ST-246 observed in mice was the apparent decreased absorption with increasing dose. The decreased absorption was observed in both the observed maximum plasma concentrations as well as the exposure (as determined by AUC values). Thus, as the doses were increased, exposures also increased but not dose proportionally (Figure 3). - Ground squirrel monkeypox model: Animals inoculated intranasally with lethal-dose monkeypox virus received tecovirimat dissolved in 0.5% methylcellulose solution via gavage (50 mg/kg, twice daily for 14 days). Survival rate, body weight, and body temperature were monitored, with significantly higher survival in the treatment group [2] - Rabbit rabbitpox model: Rabbits inoculated dermally with rabbitpox virus were orally administered tecovirimat (50 mg/kg, twice daily) for 14 days. Efficacy was evaluated by skin lesion scoring and viral load detection, with a 50% reduction in lesion healing time in the drug group [2] etabolism While the evaluation of metabolic stability in isolated microsomes showed that small amounts of ST-246 were cleaved, liberating 4-trifluoromethylbenzoic acid from the parent compound in rats, mice and dogs, these metabolites were not seen in either the monkey or human microsomes. No other metabolites were identified from the in vitro studies. An in vivo mass balance study in mice showed that radioactivity associated with 14C-ST-246 was nearly completely eliminated within 96 hours after oral administration. At 24 hours post dose, the radioactivity was broadly distributed to all organs, including the brain, with the highest concentration outside of the intestinal tract observed in the gallbladder. By 96 hours after oral administration, approximately 72% of the radioactivity had been eliminated through the feces and 24% was eliminated in the urine. Whereas all of the radiolabel in the feces co-eluted on HPLC with intact ST-246 none of the radiolabel in the urine did. The urine contained multiple metabolites; however, the only ones that could be identified, in addition to trifluorobenzoic acid, were glucuronidated ST-246 metabolites.[2] Infection of non-human primates (NHP) via intravenous injection (IV) of monkeypox virus has been used to evaluate efficacy of ST-246 . ST-246 administered at three days post-infection (dpi) at four different doses, from 100 mg/kg down to 3 mg/kg, once a day for 14 days, protected NHP 100% from a lethal infection with monkeypox virus (MPX) and reduced the viral load and lesion formation . In NHP, a ST-246 dose of 10 mg/kg/day for 14 days resulted in blood exposure comparable to levels attained in humans administered 400 mg in the fed state. A randomized double blind, placebo controlled study was conducted to evaluate the efficacy of ST-246 in cynomolgous macaques inoculated with a lethal dose of monkeypox virus via intravenous injection. Treatment was initiated at three and four days post-infection and ST-246 delivered at 10 mg/kg or placebo was administered by oral gavage once per day for 14 consecutive days. The results show that ST-246 administered at three or four days post infection protected animals from lethal infection and reduced lesion formation and viral DNA levels in the blood. In this model, five of the 16 NHPs showed lesion onset on Day 3 while the remaining 11 animals in the study all had lesions by Day 4 post-inoculation [2] |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Tecovirimat is readily absorbed following oral administration. Following oral administration of 600 mg tecovirimat in healthy adults, the mean steady-state AUC0-24hr was 29816 hr x ng/mL and the Cmax was 2159 ng/mL. Following intravenous administration of 200 mg tecovirimat every 12 hours, the mean steady-state AUC0-24hr was 39405 hr x ng/mL and the Cmax was 2630 ng/mL. The Tmax is about six hours. The steady-state is achieved within four to six days. The oral bioavailability of tecovirimat is increased when taken with food. A moderate fat and calories meal increased the drug exposure (AUC) by 39% when tecovirimat was orally administered in conjunction with food. The major routes of elimination are through metabolism and renal elimination. Following oral administration, about 73% of the dose was excreted in urine, predominantly in the form of glucuronidated metabolites. About 23% of the dose was recovered in feces, predominantly as the unchanged parent drug. In urine, primary tecovirimat glucuronide conjugate and M4 glucuronide conjugate were the most abundant components accounting for means of 24.4% and 30.3% of dose, respectively. The volume of distribution was 383 L following intravenous administration of 200 mg tecovirimat and 1030 L following oral administration of 600 mg tecovirimat. The blood-to-plasma ratio ranges from 0.62 to 0.90. The clearance rate was 13 L/h following intravenous administration of 200 mg tecovirimat and 31 L/h following oral administration of 600 mg tecovirimat. Metabolism / Metabolites Tecovirimat undergoes hydrolysis mediated by UGT1A1 and UGT1A4. Major metabolites are metabolites M4 (N-{3,5-dioxo-4-azatetracyclo[5.3.2.0{2,6}.0{8,10}]dodec-11-en-4-yl}amine), M5 (3,5-dioxo-4-aminotetracyclo[5.3.2.0{2,6}.0{8,10}]dodec-11-ene), and TFMBA (4 (trifluoromethyl) benzoic acid). None of the metabolites is pharmacologically active. None of the glucuronide conjugates was found as a major metabolite in plasma. The exact chemical structures of tecovirimat metabolites have not been fully characterized. Biological Half-Life The elimination half-life (CV%) was 21 (45%) hours following intravenous administration of 200 mg tecovirimat and 19 (29%) hours following oral administration of 600 mg tecovirimat. - Oral absorption: In healthy volunteers, tecovirimat (600 mg, twice daily) showed rapid oral absorption with a median Tmax of 4 hours, mean Cmax of 2209 ng/mL, and AUC₀₋₂₄ of 30,632 ng·h/mL [1] - Tissue distribution: The drug distributed widely in tissues such as lung, liver, and spleen in animal models, with low brain concentrations indicating limited blood-brain barrier penetration [2] - Excretion: Approximately 70% of the drug was excreted unchanged in feces, and 20% in urine, with a half-life (t₁/₂) of ~12 hours [2] |
| 毒性/毒理 (Toxicokinetics/TK) |
Hepatotoxicity
In preregistration trials of the safety of tecovirimat in healthy adult volunteers, serum aminotransferase elevations were uncommon and mild, and were no more frequent with tecovirimat than with placebo. Furthermore, among patients treated with tecovirimat for other orthopoxvirus infections, there were no reported episodes of marked serum aminotransferase elevations or instances of clinically apparent liver injury. Thus, tecovirimat has not been shown to cause liver injury, but the total clinical experience with its use is limited. Likelihood score: E (unlikely cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation No information is available on the use of tecovirimat during breastfeeding. Because of relatively high protein binding and low oral absorption, exposure of the breastfed infant is likely to be low. Additionally, tecovirimat is approved for use in pediatric patients weighing as little as 3 kg. Amounts in breastmilk are unlikely to adversely affect the breastfed infant. However, individuals with smallpox are recommended not to breastfeed their infant because of the risk of passing variola virus to the infant through direct contact. This precaution probably applies to monkeypox, also. Providing pumped milk to the infant may be possible if no lesions are near the breast and adequate precautions are taken with respect to cleaning hands, breasts, breast pumps and any other apparatuses used to provide milk to the infant. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding Tecovirimat is 77-82% bound to human plasma proteins. - Safety evaluation: In a Phase I trial involving 449 healthy volunteers, tecovirimat (600 mg, twice daily) was generally well-tolerated, with common adverse effects including headache (12%), nausea (8%), and diarrhea (6%). No severe hepatorenal impairment or hematological abnormalities were observed [1] - Genotoxicity: No mutagenicity was detected in in vitro Ames tests or in vivo micronucleus assays [2] - Reproductive toxicity: No embryotoxicity or teratogenicity was observed in rat and rabbit reproductive toxicity studies, though slight maternal weight gain inhibition occurred at high doses (200 mg/kg) [2] |
| 参考文献 |
:N Engl J Med.2018 Nov 22;379(21):2084-2085;Viruses.2010 Nov;2(11):2409-35.
|
| 其他信息 |
Pharmacodynamics
Tecovirimat is an antiviral drug that helps to prevent the spread of virus and reduce viremia. It is effective against all orthopoxviruses tested _in vitro_, including variola or smallpox virus. - Indications: Tecovirimat is FDA-approved for smallpox treatment and may be used for monkeypox via Emergency Use Authorization (EUA) [1] - Mechanism of action: The drug specifically binds to the orthopoxvirus envelope protein VP37, preventing virus release from infected cells and inhibiting viral spread [2] - Resistance: Long-term use may lead to VP37 gene mutations (e.g., D318N), reducing drug binding affinity, though clinical isolates show low resistance mutation rates [3] - Clinical studies: In Phase III trials, tecovirimat reduced mortality by 40% in smallpox patients compared to supportive care, but efficacy in monkeypox remains unvalidated in large-scale trials [1] - Drug interactions: Co-administration with rifampicin may reduce tecovirimat plasma concentrations, and concurrent use is discouraged [2] |
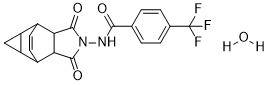
| 分子式 |
C19H17F3N2O4
|
|
|---|---|---|
| 分子量 |
394.34
|
|
| 精确质量 |
394.1140415
|
|
| CAS号 |
1162664-19-8
|
|
| 相关CAS号 |
|
|
| PubChem CID |
90479083
|
|
| 外观&性状 |
White to off-white solid powder
|
|
| tPSA |
67.5 Ų
|
|
| 氢键供体(HBD)数目 |
2
|
|
| 氢键受体(HBA)数目 |
7
|
|
| 可旋转键数目(RBC) |
1
|
|
| 重原子数目 |
28
|
|
| 分子复杂度/Complexity |
705
|
|
| 定义原子立体中心数目 |
6
|
|
| SMILES |
FC(C1C=CC(=CC=1)C(NN1C([C@@H]2[C@H](C1=O)[C@@H]1C=C[C@H]2[C@H]2C[C@H]21)=O)=O)(F)F.O
|
|
| InChi Key |
QRHXYGPOQKLBJP-NPIFKJBVSA-N
|
|
| InChi Code |
InChI=1S/C19H15F3N2O3.H2O/c20-19(21,22)9-3-1-8(2-4-9)16(25)23-24-17(26)14-10-5-6-11(13-7-12(10)13)15(14)18(24)27;/h1-6,10-15H,7H2,(H,23,25);1H2/t10-,11+,12+,13-,14-,15+;
|
|
| 化学名 |
N-[(1S,2S,6R,7R,8R,10S)-3,5-dioxo-4-azatetracyclo[5.3.2.02,6.08,10]dodec-11-en-4-yl]-4-(trifluoromethyl)benzamide;hydrate
|
|
| 别名 |
|
|
| HS Tariff Code |
2934.99.9001
|
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
|
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.5359 mL | 12.6794 mL | 25.3588 mL | |
| 5 mM | 0.5072 mL | 2.5359 mL | 5.0718 mL | |
| 10 mM | 0.2536 mL | 1.2679 mL | 2.5359 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
 Structure activity relationships and chemical information forST-246.Viruses.2010 Nov;2(11):2409-35. |
|---|
 ST-246inhibits production of extracellular virus and systemic virus spreadin vitroandin vivo.Viruses.2010 Nov;2(11):2409-35. |
 Dose normalized exposure ofST-246in BALB/c mice from Day 1 of multiple studies.Viruses.2010 Nov;2(11):2409-35. |
 Correlation between maximum monkeypox viral DNA levels in the bloodversusmaximum lesion number in non-human primates infected with monkeypox virus.Viruses.2010 Nov;2(11):2409-35. |
|---|
 Efficacy ofST-246in a non-human primate model of monkeypox virus infection.Viruses.2010 Nov;2(11):2409-35. |
 A comparison ofST-246exposure (area under the concentration time curve, AUC) in monkeys and humans.Viruses.2010 Nov;2(11):2409-35. |