| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| 250mg | |||
| Other Sizes |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Oral bioavailability is nearly complete, at approximately 90%, and peak serum concentrations (Cmax) of, on average, 2.50 µg/mL are reached at 0.75 hours (Tmax). The AUC following an orally administered dose of 300mg was found to be approximately 11 µg•hr/mL. Systemic exposure from the administration of vaginal suppository formulations is 40-fold to 50-fold lower than that observed following parenteral administration and the Cmax observed following administration of vaginal cream formulations was 0.1% of that observed following parenteral administration. Approximately 10% of clindamycin bioactivity is excreted in the urine and 3.6% in the feces, with the remainder excreted as inactive metabolites. Clindamycin is widely distributed in the body, including into bone, but does not distribute into cerebrospinal fluid. The volume of distribution has been variably estimated between 43-74 L. The plasma clearance of clindamycin is estimated to be 12.3-17.4 L/h, and is reduced in patients with cirrhosis and altered in those with anemia. Clindamycin is nearly completely absorbed following oral admin. Peak plasma concn of 2 to 3 ug/mL are attained within 1 hr after the ingestion of 150 mg. The presence of food in stomach does not reduce absorption. The half-life of the antibiotic is about 2.9 hr, and the modest accumulation of drug is thus expected if it is given at 6-hr intervals. Clindamycin is widely distributed in many fluids and tissues, including bone. Significant concn are not attained in cerebrospinal fluid, even when the meninges are inflamed. Concn sufficient to treat cerebral toxoplasmosis are achievable .. The drug readily crosses the placental barrier. 90% or more of clindamycin is bound to plasma proteins. Clindamycin accumulates in polymorphonuclear leukocytes, alveolar macrophages, and in abscesses. Half-life ... is lengthened only slightly in patients with markedly impaired renal function ... Clindamycin is distributed into many body tissues and fluids including saliva, ascites fluid, pleural fluid, synovial fluid, bone, and bile. However, even in the presence of inflamed meninges, only small amounts of the drug diffuse into CSF. The concentration of clindamycin in synovial fluid and bone is reported to be 60-80% of concurrent serum concentrations of the drug; the degree of penetration does not appear to be affected by joint inflammation. Clindamycin readily crosses the placenta, and cord blood concentrations of the drug have been reported to be 46% of concurrent maternal blood concentrations. Clindamycin is distributed into milk. For more Absorption, Distribution and Excretion (Complete) data for CLINDAMYCIN (24 total), please visit the HSDB record page. Metabolism / Metabolites Clindamycin undergoes hepatic metabolism mediated primarily by CYP3A4 and, to a lesser extent, CYP3A5. Two inactive metabolites have been identified - an oxidative metabolite, clindamycin sulfoxide, and an N-demethylated metabolite, N-desmethylclindamycin. Clindamycin is partially metabolized to bioactive and inactive metabolites. The major bioactive metabolites are clindamycin sulfoxide and N-demethyl-clindamycin which are excreted in urine, bile, and feces. Within 24 hours, approximately 10% of an oral dose of clindamycin is excreted in urine and 3.6% is excreted in feces as active drug and metabolites; the remainder is excreted as inactive metabolites. Only about 10% of the clindamycin admin is excreted unaltered in urine, and small quantities are found in feces ... Clindamycin is inactivated by metabolism to N-demethylclindamycin and clindamycin sulfoxide, which are excreted in the urine and bile. Clindamycin has known human metabolites that include N-desmethyclindamycin and clindamycin sulfoxide. Biological Half-Life The elimination half-life of clindamycin is about 3 hours in adults and 2.5 hours in children. Half-life is increased to approximately 4 hours in the elderly. The serum half-life of clindamycin is 2-3 hours in adults and children with normal renal function. The serum half-life is increased slightly in patients with markedly reduced renal or hepatic function. In neonates, the serum half-life depends on gestational and chronologic age and body weight. The serum half-life of clindamycin reportedly averages 8.7 and 3.6 hours in premature and full-term neonates, respectively, and about 3 hours in infants 4 weeks to 1 year of age; serum half-life was longer in infants weighing less than 3.5 kg than in heavier infants. The half-life of ... /clindamycin/ is about 2.9 hr ... Following intravaginal application of 2% clindamycin cream, the systemic half-life of the drug appears to be about 1.5-2.6 hours. Following intravaginal administration of clindamycin suppositories, the apparent elimination half-life averaged about 11 hours (range: 4-35 hours). |
|---|---|
| 毒性/毒理 (Toxicokinetics/TK) |
Hepatotoxicity
Clindamycin has been linked to two forms of hepatotoxicity: transient serum aminotransferase elevations usually occurring after several days of high intravenous doses; and, an acute, idiosyncratic liver injury that arises within 1 to 3 weeks of starting therapy and is typically mild and self-limited. High doses of intravenous clindamycin can be accompanied by elevations in serum ALT levels in the range of 2 to 10 times the upper limit of normal starting after 5 to 15 days of therapy in a manner similar to what occurs with intravenous oxacillin therapy (Case 1). Symptoms, jaundice, and alkaline phosphatase elevations are mild if they occur at all (Case 2), and aminotransferase levels rapidly fall into the normal range (in 1 to 2 weeks) upon stopping clindamycin or switching to lower doses or to oral formulations with which it rarely occurs. Clindamycin therapy has also been linked to a clinically apparent, idiosyncratic liver injury that arises between 1 to 3 weeks after starting either oral or parenteral therapy (Case 3). The pattern of serum enzyme elevations is typically hepatocellular or mixed, but can be cholestatic. Allergic manifestations such as rash, fever and eosinophilia are typical, but often are not prominent and are not present in all cases. Autoantibodies are generally not present. The acute liver injury may accompany other signs of hypersensitivity such as Stevens Johnson syndrome or other severe skin reactions. The liver injury is usually mild-to-moderate in severity and resolves rapidly with stopping. However, fatal instances have been reported. Likelihood score: B (highly likely cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Clindamycin has the potential to cause adverse effects on the breastfed infant's gastrointestinal flora. If oral or intravenous clindamycin is required by a nursing mother, it is not a reason to discontinue breastfeeding, but an alternate drug may be preferred. Monitor the infant for possible effects on the gastrointestinal flora, such as diarrhea, candidiasis (thrush, diaper rash) or rarely, blood in the stool indicating possible antibiotic-associated colitis. Vaginal application is unlikely to cause infant side effects, although about 30% of a vaginal dose is absorbed. Infant side effects are unlikely with topical administration for acne; however, topical application to the breast may increase the risk of diarrhea if it is ingested by the infant. Only water-miscible cream, foam, gel or liquid products should be applied to the breast because ointments may expose the infant to high levels of mineral paraffins via licking. ◉ Effects in Breastfed Infants Bloody stools in a 5-day-old breastfed infant were possibly caused by concurrent maternal clindamycin 600 mg intravenously every 6 hours and gentamicin 80 mg intravenously every 8 hours. The infant's stools were reported to have normal flora and the stools became guaiac negative 24 hours after discontinuation of breastfeeding. On day 6 of age, the infant resumed breastfeeding after discontinuation of maternal antibiotics with no further difficulties. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. ◈ What is clindamycin? Clindamycin is an antibiotic used to treat or prevent bacterial infections. It can be taken by mouth (oral), used on the skin (topical), or given by IV (intravenous or by needle into a vein).Sometimes when people find out they are pregnant, they think about changing how they take their medication, or stopping their medication altogether. However, it is important to talk with your healthcare providers before making any changes to how you take this medication. Your healthcare providers can talk with you about the benefits of treating your condition and the risks of untreated illness during pregnancy. ◈ I take clindamycin. Can it make it harder for me to get pregnant? It is not known if clindamycin can make it harder to get pregnant. ◈ Does taking clindamycin increase the chance for miscarriage? Miscarriage is common and can occur in any pregnancy for many different reasons. One study involving 249 women who had a vaginal bacterial infection found that clindamycin treatment reduced the chances of late miscarriage. ◈ Does taking clindamycin increase the chance of birth defects? Every pregnancy starts out with about a 1 in 33 (3%) chance of having a birth defect. This is called the background chance. It is unlikely that using clindamycin increases the chance of birth defects. Several human studies as well as animal studies have not shown an increased chance of birth defects.When clindamycin is used on the skin (topical use), only small amounts pass through skin and get into the bloodstream. This means a pregnancy would be exposed to only a very small amount of the medicine. Since available information about vaginal and oral clindamycin (both higher absorptions compared to topical use) does not find an increased chance of birth defects, it is also unlikely that using topical clindamycin increases the chance of birth defects. ◈ Does taking clindamycin in pregnancy increase the chance of other pregnancy related problems? Several studies have not found an increased chance of other pregnancy-related problems such as low birth weight (weighing less than 5 pounds, 8 ounces [2500 grams] at birth). One study involving 249 women who had a vaginal bacterial infection found that clindamycin treatment reduced the chances of preterm delivery (birth before week 37). ◈ Does taking clindamycin in pregnancy affect future behavior or learning for the child? Studies have not been done to see if clindamycin can cause behavior or learning issues for the child. ◈ Breastfeeding while taking clindamycin: Clindamycin gets into breastmilk in small amounts when women are given clindamycin orally (by mouth) or intravenously (IV). In those situations, clindamycin might cause some gastrointestinal (GI) effects in a breastfeeding (e.g. nausea, diarrhea, stomach pain, vomiting, diaper rash, thrush, or rarely bloody stools). Topical application (to the skin) has minimal absorption into the body and are unlikely to end up in breast milk in amounts that might cause side effects in a nursing baby. If you notice any symptoms in your child, contact their healthcare provider. Be sure to talk to your healthcare provider about all of your breastfeeding questions. ◈ If a male takes clindamycin, could it affect fertility or increase the chance of birth defects? Studies have not been done to see if clindamycin could affect male fertility (ability to get partner pregnant) or increase the chance of birth defects above the background risk. In general, exposures that fathers or sperm donors have are unlikely to increase the risks to a pregnancy. For more information, please see the MotherToBaby fact sheet Paternal Exposures at https://mothertobaby.org/fact-sheets/paternal-exposures-pregnancy/. Protein Binding Clindamycin protein binding is concentration-dependent and ranges from 60-94%. It is bound primarily to alpha-1-acid glycoprotein in the serum. |
| 参考文献 | |
| 其他信息 |
Clindamycin is a semi-synthetic lincosamide antibiotic used in the treatment of a variety of serious infections due to susceptible microorganisms as well as topically for acne vulgaris. It has a relatively narrow spectrum of activity that includes anaerobic bacteria as well as gram-positive cocci and bacilli and gram-negative bacilli. Interestingly, clindamycin appears to carry some activity against protozoans, and has been used off-label in the treatment of toxoplasmosis, malaria, and babesiosis. Clindamycin is derived from, and has largely replaced, [lincomycin], a naturally occurring lincosamide and the eponymous member of this antibiotic class, due to its improved properties over the parent compound. The name lincomycin is derived from Lincoln, Nebraska, where it was first isolated from Streptomyces lincolnensis found in a soil sample.
Clindamycin is a Lincosamide Antibacterial. The physiologic effect of clindamycin is by means of Decreased Sebaceous Gland Activity, and Neuromuscular Blockade. Clindamycin is a broad spectrum antibiotic used orally, topically and parenterally for bacterial infections due to sensitive organisms. Clindamycin has been linked to rare instances of acute liver injury. Clindamycin is a semisynthetic broad spectrum antibiotic produced by chemical modification of the parent compound lincomycin. Clindamycin dissociates peptidyl-tRNA from the bacterial ribosome, thereby disrupting bacterial protein synthesis. (NCI04) An antibacterial agent that is a semisynthetic analog of LINCOMYCIN. See also: Clindamycin Phosphate (has salt form); Clindamycin Hydrochloride (has salt form); Clindamycin Palmitate Hydrochloride (has salt form) ... View More ... Drug Indication In oral and parenteral formulations, clindamycin is indicated for the treatment of serious infections caused by susceptible anaerobic bacteria, as well as susceptible staphylococci, streptococci, and pneumococci. Used topically, it is indicated for the treatment of acne vulgaris and is available in combination with [benzoyl peroxide] or [tretinoin] for this purpose, or as a triple combination therapy with benzoyl peroxide and [adapalene]. Clindamycin is also indicated as a vaginal cream, suppository, or gel for the treatment of bacterial vaginosis in non-pregnant females. Clindamycin is used for antimicrobial prophylaxis against _Viridans_ group streptococcal infections in susceptible patients undergoing oral, dental, or upper respiratory surgery, and may be used for prophylaxis against bacterial endocarditis in penicillin-allergic patients at high risk of these infections. FDA Label Mechanism of Action Clindamycin inhibits bacterial protein synthesis by binding to 23S RNA of the 50S subunit of the bacterial ribosome. It impedes both the assembly of the ribosome and the translation process. The molecular mechanism through which this occurs is thought to be due to clindamycin's three-dimensional structure, which closely resembles the 3'-ends of L-Pro-Met-tRNA and deacylated-tRNA during the peptide elongation cycle - in acting as a structural analog of these tRNA molecules, clindamycin impairs peptide chain initiation and may stimulate dissociation of peptidyl-tRNA from bacterial ribosomes. The mechanism through which topical clindamycin treats acne vulgaris is unclear, but may be related to its activity against _Propionibacterium acnes_, a bacteria that has been associated with acne. Clindamycin may be bacteriostatic or bactericidal in action, depending on the concentration of the drug attained at the site of infection and the susceptibility of the infecting organism. Clindamycin palmitate hydrochloride and clindamycin phosphate are inactive until hydrolyzed to free clindamycin. This hydrolysis occurs rapidly in vivo. Clindamycin appears to inhibit protein synthesis in susceptible organisms by binding to 50S ribosomal subunits; the primary effect is inhibition of peptide bond formation. The site of action appears to be the same as that of erythromycin, chloramphenicol, and lincomycin. Clindamycin binds exclusively to the 50S subunit of bacterial ribosomes and suppresses protein synthesis. ... Clindamycin is not a substrate for macrolide efflux pumps, and strains that are resistant to macrolides by this mechanism are susceptible to clindamycin. |
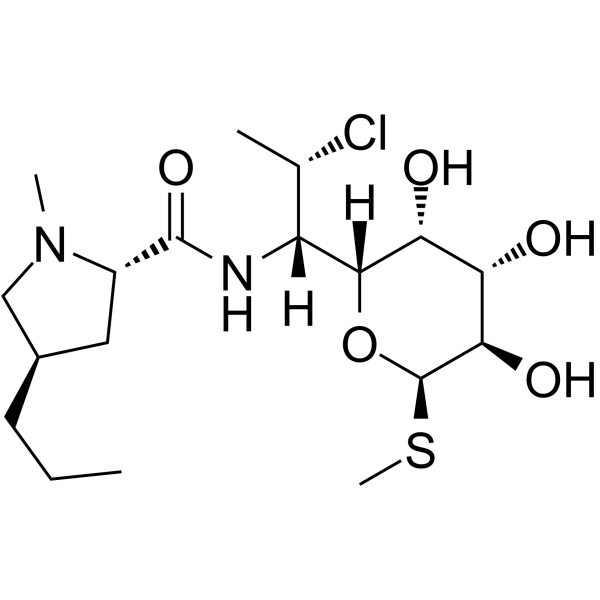
| 分子式 |
C18H33CLN2O5S
|
|---|---|
| 分子量 |
424.98
|
| 精确质量 |
424.179
|
| CAS号 |
18323-44-9
|
| 相关CAS号 |
Clindamycin hydrochloride;21462-39-5;Clindamycin phosphate;24729-96-2;Clindamycin-d3 hydrochloride;1356933-72-6;Clindamycin-13C,d3;2140264-63-5;Clindamycin hydrochloride monohydrate;58207-19-5
|
| PubChem CID |
446598
|
| 外观&性状 |
Yellow, amorphous solid
|
| 密度 |
1.3±0.1 g/cm3
|
| 沸点 |
628.1±55.0 °C at 760 mmHg
|
| 熔点 |
141 - 143ºC
|
| 闪点 |
333.6±31.5 °C
|
| 蒸汽压 |
0.0±4.2 mmHg at 25°C
|
| 折射率 |
1.574
|
| LogP |
1.83
|
| tPSA |
127.56
|
| 氢键供体(HBD)数目 |
4
|
| 氢键受体(HBA)数目 |
7
|
| 可旋转键数目(RBC) |
7
|
| 重原子数目 |
27
|
| 分子复杂度/Complexity |
502
|
| 定义原子立体中心数目 |
9
|
| SMILES |
CCC[C@@H]1C[C@H](N(C1)C)C(N[C@@H]([C@@H]2[C@H](O)[C@H](O)[C@@H](O)[C@@H](SC)O2)[C@@H](Cl)C)=O
|
| InChi Key |
KDLRVYVGXIQJDK-AWPVFWJPSA-N
|
| InChi Code |
InChI=1S/C18H33ClN2O5S/c1-5-6-10-7-11(21(3)8-10)17(25)20-12(9(2)19)16-14(23)13(22)15(24)18(26-16)27-4/h9-16,18,22-24H,5-8H2,1-4H3,(H,20,25)/t9-,10+,11-,12+,13-,14+,15+,16+,18+/m0/s1
|
| 化学名 |
(2S,4R)-N-((1S,2S)-2-chloro-1-((2R,3R,4S,5R,6R)-3,4,5-trihydroxy-6-(methylthio)tetrahydro-2H-pyran-2-yl)propyl)-1-methyl-4-propylpyrrolidine-2-carboxamide
|
| 别名 |
U-21251 U 21251 ClindamycinCleocin, Clinacin, Dalacin
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 本产品在运输和储存过程中需避光。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : ~125 mg/mL (~294.13 mM)
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.3531 mL | 11.7653 mL | 23.5305 mL | |
| 5 mM | 0.4706 mL | 2.3531 mL | 4.7061 mL | |
| 10 mM | 0.2353 mL | 1.1765 mL | 2.3531 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。