| 规格 | 价格 | |
|---|---|---|
| 500mg | ||
| 1g | ||
| Other Sizes |
| 靶点 |
LSD1/lysine specific demethylase 1 (IC50 = 16 nM)
|
|---|---|
| 体外研究 (In Vitro) |
GSK-LSD1 DiHClide 的选择性比其他密切相关的 FAD 利用酶(包括 LSD2 和单胺氧化酶 MAO-A、MAO-B)高出 1000 倍以上[1]。 GSK-LSD1 可抑制 KDM1A/LSD1 酶活性。 GSK-LSD1 诱导 U2OS 细胞中 LC3-II 的形成。电子显微镜显示GSK-LSD1处理后自噬体的形成。 GSK-LSD1 通过改变基因表达模式有效抑制多种癌细胞系的增殖[2]。
|
| 体内研究 (In Vivo) |
为了评估LSD1在体内的抑制活性,用GSK-LSD1处理植入1×10~5 MLL-AF9原代AML细胞的次级受体小鼠。在14天的治疗窗口内,每天以0.5mg/kg的剂量给药。只有在确认外周血植入后才开始治疗(补充图1A,可在血液网站上获得)。治疗后,杀死一些小鼠,并使用流式细胞术检测GFP作为MLL-AF9等位基因负荷的读数进行分析。GSK-LSD1治疗的小鼠骨髓(图1A)、外周血和脾脏中GFP+细胞的比例较低(补充图1B-C)。在GSK-LSD1治疗的情况下,包括脾脏重量在内的其他疾病负担指标显著降低(补充图1E)。经GSK-LSD1治疗的小鼠血小板计数显著下降(P=0.003;补充图1D),这与LSD1耗竭的靶向效应一致。18经GSK-LSD1治疗3天后,骨髓细胞的免疫表型显示,共表达c-kit和Mac-1的更原始的GFP+白血病细胞减少(图1B)。与对照组小鼠(中位生存期39天)相比,GSK-LSD1治疗的小鼠存活率(中位存活期78天)也显著提高(图1C)。令人惊讶的是,一小部分接受治疗的小鼠在移植后248天也没有检测到疾病。为了证实LSD1抑制对存活的这种影响,我们对从单独用载体或GSK-LSD1治疗3天的白血病小鼠中采集的MLL-AF9细胞进行了连续移植。将同等数量的从载体或GSK-LSD1处理的小鼠中纯化的GFP+细胞注射到亚致死照射的小鼠体内。与载体处理的小鼠相比,移植了从GSK-LSD1处理的小鼠中获得的细胞的第三受体小鼠的存活率有所提高。虽然移植了载体处理细胞的受体小鼠的中位存活期为23天,但用GSK-LSD1处理的白血病细胞攻击的小鼠的中位数存活期为51天(图1D)。植入GSK-LSD1治疗的白血病细胞的小鼠中,只有50%死于AML。剩下的50%移植了GSK-LSD1处理细胞的小鼠在移植后308天内保持健康,没有出现白血病的迹象。这些数据表明,在MLL-AF9驱动的急性髓系白血病(AML)的侵袭性模型中,LSD1抑制具有强大的抗白血病活性,可提高总体生存率,偶尔可导致疾病完全根除。https://pmc.ncbi.nlm.nih.gov/articles/PMC5897868/
|
| 细胞实验 |
细胞周期分析
通过用GSKLSD1体外处理48小时的细胞的BrdU染色进行细胞周期分析。使用BrdU流动试剂盒(BD Biosciences)。简而言之,在暴露于GSK-LSD1 48小时后,根据制造商的说明将细胞暴露于10µM BrdU 20分钟。之后,收获细胞,使其透性,并用APC标记的抗BrdU抗体染色,而白血病细胞为GFP+(含有pMSCV-ML-AF9-IRES-GFP质粒)。使用SYTOX™蓝死细胞染色法进行DNA染色。SYTOX Blue信号是以线性模式采集的。https://pmc.ncbi.nlm.nih.gov/articles/PMC5897868/#sec12 通过在添加了15%FBS、IL-3、IL-6和mSCF的IMDM中培养细胞,并单独添加载体或浓度为0.5µM的GSK-LSD1,体外处理MLL-AF9白血病细胞48小时。同样,白血病细胞用浓度为1µM的DOT1L抑制剂EPZ4777处理6天。根据制造商的说明进行菌落形成试验。简而言之,将500个细胞/皿铺在MC3434甲基纤维素中,并在孵育6天后对菌落数量进行评分。对于每个组,对3个独立的培养皿进行评分,并至少进行两次菌落测定。在第0天将GSK-LSD1以0.5µM的浓度加入MC3434半固体培养基中,六天后对菌落进行评分。https://pmc.ncbi.nlm.nih.gov/articles/PMC5897868/#sec12 |
| 动物实验 |
For in vivo treatment experiments, GSK-LSD1 was administered via intraperitoneal injections at a dose of 0.5 mg/kg daily. Treatment was initiated only after peripheral blood engraftment of MLL-AF9 leukemia cells was confirmed at a minimum chimerism of 0.1-1% GFPpositive cells for syngeneic murine MLL-AF9 leukemia cells or 12.3% ± 2.7 hCD45-positive cells for xenotransplantation experiments. Mice were treated for 3 days (Figure 1B), 2 weeks (Figure 1C) or 6 weeks (Figure 1G). Cytological staining was performed on cytospin preparations of suspension cells from in vitro culture (Figures 1E, 5E, 6D+F) or from peripheral blood of mice (Figure 1J) using the Deep Quick Stain kit. https://pmc.ncbi.nlm.nih.gov/articles/PMC5897868/#sec12
|
| 参考文献 |
Biochim Biophys Acta. 2017 Aug 8;1864(12):2428-2437.; http://www.thesgc.org/chemical-probes/LSD1.
|
| 其他信息 |
Epigenetic factors and related small molecules have emerged to be strongly involved in autophagy process. Here we report that 2-PCPA and GSK-LSD1, two inhibitors of histone H3K4 demethylase KDM1A/LSD1, induce autophagy in multiple mammalian cell lines. The two small molecules induce accumulation of LC3II, formation of autophagosome and autolysosome, and SQSTM1/p62 degradation. 2-PCPA treatment inhibits cell proliferation through cell cycle arrest but does not inducing cell death. Exogenous expression of KDM1A/LSD1 impaired the autophagic phenotypes triggered by 2-PCPA. The autophagy induced by 2-PCPA requires LC3-II processing machinery. But depletion of BECN1 and ULK1 with siRNA did not affect the LC3-II accumulation triggered by 2-PCPA. 2-PCPA treatment induces the change of global gene expression program, including a series of autophagy-related genes, such as SQSTM1/p62. Taken together, our data indicate that KDM1A/LSD1 inhibitors induce autophagy through affecting the expression of autophagy-related genes and in a BECN1-independent manner.Biochim Biophys Acta. 2017 Aug 8;1864(12):2428-2437
Epigenetic regulators are recurrently mutated and aberrantly expressed in acute myeloid leukemia (AML). Targeted therapies designed to inhibit these chromatin-modifying enzymes, such as the histone demethylase lysine-specific demethylase 1 (LSD1) and the histone methyltransferase DOT1L, have been developed as novel treatment modalities for these often refractory diseases. A common feature of many of these targeted agents is their ability to induce myeloid differentiation, suggesting that multiple paths toward a myeloid gene expression program can be engaged to relieve the differentiation blockade that is uniformly seen in AML. We performed a comparative assessment of chromatin dynamics during the treatment of mixed lineage leukemia (MLL)-AF9-driven murine leukemias and MLL-rearranged patient-derived xenografts using 2 distinct but effective differentiation-inducing targeted epigenetic therapies, the LSD1 inhibitor GSK-LSD1 and the DOT1L inhibitor EPZ4777. Intriguingly, GSK-LSD1 treatment caused global gains in chromatin accessibility, whereas treatment with EPZ4777 caused global losses in accessibility. We captured PU.1 and C/EBPα motif signatures at LSD1 inhibitor-induced dynamic sites and chromatin immunoprecipitation coupled with high-throughput sequencing revealed co-occupancy of these myeloid transcription factors at these sites. Functionally, we confirmed that diminished expression of PU.1 or genetic deletion of C/EBPα in MLL-AF9 cells generates resistance of these leukemias to LSD1 inhibition. These findings reveal that pharmacologic inhibition of LSD1 represents a unique path to overcome the differentiation block in AML for therapeutic benefit.https://pmc.ncbi.nlm.nih.gov/articles/PMC5897868/#sec12 |
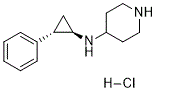
| CAS号 |
1431367-51-9
|
|---|---|
| 相关CAS号 |
1431368-48-7 (rel-free base) 1821798-25-7 (2HCl) 2102933-95-7 (rel-2HCl) 1431368-50-1 1431367-49-5 (rel-HCl) 1431367-51-9 (HCl) |
| PubChem CID |
61815034
|
| 外观&性状 |
Typically exists as solid at room temperature
|
| 别名 |
CHEMBL3945250; 1431368-48-7; GSK-LSD1 HCl; SCHEMBL14880456; 1431367-51-9;
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。