| 规格 | 价格 | ||
|---|---|---|---|
| 500mg | |||
| 1g | |||
| Other Sizes |
| 体外研究 (In Vitro) |
伊布利特是 IKr 的强抑制剂,在心房肿瘤肌细胞 (AT-1) 细胞中,+20 mV 时的 EC50 值为 20 nM [1]。它在表达 HERG+MDR1*1 的细胞中阻断 IKr 的程度与在单独表达 HERG 的细胞中的阻断程度相同(IC50:22.5 nM vs 27.4 nM)。另一方面,表达 MDR1*7 的细胞表现出对伊布利特的显着耐药性(IC50:105.3 nM vs 27.4 nM)[2]。
|
|---|---|
| 体内研究 (In Vivo) |
在体内和体外,伊布利特都能延长心脏复极时间[1]。伊布利特输注可导致单形性和多形性非持续性室性心动过速[3]。 0.01、0.02和0.05mg/kg iv的三个累积剂量在10分钟内施用。
|
| 动物实验 |
Animal/Disease Models: 15 adult mongrel dogs, both male and female [1]
Doses: 0.01, 0.02 and 0.05 mg/kg Route of Administration: intravenous (iv) (iv)injection; injection administration. Results for each 10-minute infusion: Action potential duration (APD90) at 90% prolongation was Dramatically longer in patients with congestive heart failure (CHF) treated with ibutilide (0.01 mg/kg) compared with controls. An increase in left and right ventricular APD90 dispersion was observed in CHF at 0.01 mg/kg but not in the control group. |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Rapid after intravenous injection In healthy male volunteers, about 82% of a 0.01 mg/kg dose of [14C] ibutilide fumarate was excreted in the urine (about 7% of the dose as unchanged ibutilide) and the remainder (about 19%) was recovered in the feces. 11 L/kg 29 mL/min/kg Sixteen adult patients with atrial fibrillation or atrial flutter requiring conversion to normal sinus rhythm: six patients who had New York Heart Association (NYHA) class II or III heart failure due to left ventricular dysfunction (mean +/- SD left ventricular ejection fraction (LVEF) 30 +/- 9%); 10 patients who did not have left ventricular dysfunction (mean +/- SD LVEF 54 +/- 5% in six of these 10 patients) served as controls. All patients received a single dose of ibutilide 1.0 mg administered intravenously over 10 minutes. Blood samples were obtained through an indwelling catheter in the contralateral arm before ibutilide administration, at the end of the infusion, and at 5, 15, 30, 45 minutes and 1, 1.5, 2, 3, 4, 6, 8, 10, 12, 24, and 48 hours after the infusion. Serum ibutilide concentrations were determined by using high-performance liquid chromatography and mass spectrometry. No significant differences were noted between the heart failure and normal left ventricular function groups in the following parameters: maximum serum ibutilide concentration (median (interquartile range) 3.8 (2.3-5.7) vs 5.8 (3.1-14.4) ug/L, p=0.31), area under the serum concentration-time curve from time zero extrapolated to infinity (mean +/- SD 11.0 +/- 9.4 vs 13.2 +/- 10.6 ug*hr/L, p=0.88), steady-state volume of distribution (1380 +/- 334 vs 1390 +/- 964 L, p=0.99), systemic clearance (129 +/- 60 vs 125 +/- 81 L/hr, p=0.92), or half-life (12.5 +/- 10.7 vs 12.4 +/- 8.6 hrs, p=0.99). The pharmacokinetics of ibutilide do not appear to be altered in patients with NYHA class II or III heart failure due to left ventricular systolic dysfunction. In healthy male volunteers, about 82% of a 0.01 mg/kg dose of (14)C ibutilide fumarate was excreted in the urine (about 7% of the dose as unchanged ibutilide) and the remainder (about 19%) was recovered in the feces. After intravenous infusion, ibutilide plasma concentrations rapidly decrease in a multiexponential fashion. The pharmacokinetics of ibutilide are highly variable among subjects. Ibutilide has a high systemic plasma clearance that approximates liver blood flow (about 29 mL/min/kg), a large steady-state volume of distribution (about 11 L/kg) in healthy volunteers, and minimal (about 40%) protein binding. Ibutilide is also cleared rapidly and highly distributed in patients being treated for atrial flutter or atrial fibrillation. The elimination half-life averages about 6 hours (range from 2 to 12 hours). The pharmacokinetics of ibutilide are linear with respect to the dose of Corvert over the dose range of 0.01 mg/kg to 0.10 mg/kg. The enantiomers of ibutilide fumarate have pharmacokinetic properties similar to each other and to ibutilide fumarate. Metabolism / Metabolites Primarily hepatic. Eight metabolites of ibutilide were detected in metabolic profiling of urine. These metabolites are thought to be formed primarily by o-oxidation followed by sequential b-oxidation of the heptyl side chain of ibutilide. Of the eight metabolites, only the o-hydroxy metabolite possesses class III electrophysiologic properties similar to that of ibutilide in an in vitro isolated rabbit myocardium model. Eight metabolites of ibutilide were detected in metabolic profiling of urine. These metabolites are thought to be formed primarily by omega-oxidation followed by sequential beta-oxidation of the heptyl side chain of ibutilide. Of the eight metabolites, only the omega-hydroxy metabolite possesses class III electrophysiologic properties similar to that of ibutilide in an in vitro isolated rabbit myocardium model. The plasma concentrations of this active metabolite, however, are less than 10% of that of ibutilide. Biological Half-Life 6 hours (ranges from 2-12 hours) The elimination half-life averages about 6 hours (range from 2 to 12 hours). Sixteen adult patients with atrial fibrillation or atrial flutter requiring conversion to normal sinus rhythm: six patients who had New York Heart Association (NYHA) class II or III heart failure due to left ventricular dysfunction (mean +/- SD left ventricular ejection fraction (LVEF) 30 +/- 9%); 10 patients who did not have left ventricular dysfunction (mean +/- SD LVEF 54 +/- 5% in six of these 10 patients) served as controls. All patients received a single dose of ibutilide 1.0 mg administered intravenously over 10 minutes. ... No significant differences were noted between the heart failure and normal left ventricular function groups in the following parameters: ... half-life (12.5 +/- 10.7 vs 12.4 +/- 8.6 hrs, p=0.99). |
| 毒性/毒理 (Toxicokinetics/TK) |
Protein Binding
40% Interactions Supraventricular arrhythmias may mask the cardiotoxicity associated with excessive digoxin levels. Therefore, it is advisable to be particularly cautious in patients whose plasma digoxin levels are above or suspected to be above the usual therapeutic range. Coadministration of digoxin did not have effects on either the safety or efficacy of ibutilide in the clinical trials. The potential for proarrhythmia may increase with the administration of ibutilide fumarate injection to patients who are being treated with drugs that prolong the QT interval, such as phenothiazines, tricyclic antidepressants, tetracyclic antidepressants, and certain antihistamine drugs (H1 receptor antagonists). Class Ia antiarrhythmic drugs (Vaughan Williams Classification), such as disopyramide, quinidine, and procainamide, and other class III drugs, such as amiodarone and sotalol, should not be given concomitantly with ibutilide fumarate injection or within 4 hours postinfusion because of their potential to prolong refractoriness. In the clinical trials, class I or other class III antiarrhythmic agents were withheld for at least 5 half-lives prior to ibutilide infusion and for 4 hours after dosing, but thereafter were allowed at the physician's discretion. Ibutilide is a class III antiarrhythmic agent indicated for cardioversion of atrial fibrillation and atrial flutter to sinus rhythm (SR). The most serious complication of ibutilide is torsades de pointes (TdP). Magnesium has been successfully used for the treatment of TdP, but its use as a prophylactic agent for this arrhythmia has not yet been established. The present study investigated whether high dose of magnesium would increase the safety and efficacy of ibutilide administration. A total of 476 patients with atrial fibrillation or atrial flutter who were candidates for conversion to SR were divided into 2 groups. Group A consisted of 229 patients who received ibutilide to convert atrial fibrillation or atrial flutter to SR. Group B consisted of 247 patients who received an intravenous infusion of 5 g of magnesium sulfate for 1 hour followed by the administration of ibutilide. Then, another 5 g of magnesium were infused for 2 additional hours. Of the patients in groups A and B, 154 (67.3%) and 189 (76.5%), respectively, were converted to SR (p = 0.033). Ventricular arrhythmias (sustained, nonsustained ventricular tachycardia, and TdP) occurred significantly more often in group A than in group B (7.4% vs 1.2%, respectively, p = 0.002). TdP developed in 8 patients (3.5%) in group A and in none (0%) in group B (p = 0.009). The administration of magnesium (despite the high doses used) was well tolerated. In conclusion, the administration of high doses of magnesium probably makes ibutilide a much safer agent, and magnesium increased the conversion efficacy of ibutilide. |
| 参考文献 |
[1]. Ibutilide, a methanesulfonanilide antiarrhythmic, is a potent blocker of the rapidly activating delayed rectifier K+ current (IKr) in AT-1 cells. Concentration-, time-, voltage-, and use-dependent effects. Circulation. 1995 Mar 15;91(6):1799-806.
[2]. B F McBride, et al. Influence of the G2677T/C3435T haplotype of MDR1 on P-glycoprotein trafficking and Ibutilide-induced block of HERG. Pharmacogenomics J. 2009 Jun;9(3):194-201. [3]. S S Chugh, et al. Altered response to Ibutilide in a heart failure model. Cardiovasc Res. 2001 Jan;49(1):94-102. |
| 其他信息 |
Therapeutic Uses
Anti-Arrhythmia Agents Ibutilide fumarate injection is indicated for the rapid conversion of atrial fibrillation or atrial flutter of recent onset to sinus rhythm. Patients with atrial arrhythmias of longer duration are less likely to respond to ibutilide fumarate injection. The effectiveness of ibutilide has not been determined in patients with arrhythmias of more than 90 days in duration. /Included in US product label/ Ibutilide is administered as a rapid infusion (1 mg over 10 minutes) for the immediate conversion of atrial fibrillation or flutter to sinus rhythm. The drug's efficacy rate is higher in patients with atrial flutter (50-70%) than in those with atrial fibrillation (30-50%). In atrial fibrillation, the conversion rate is lower in those in whom the arrhythmia has been present for weeks or months compared with those in whom it has been present for days. Drug Warnings /BOXED WARNING/ LIFE-THREATENING ARRHYTHMIAS-APPROPRIATE TREATMENT ENVIRONMENT. Covert can cause potentially fatal arrhythmias, particularly sustained polymorphic ventricular tachycardia, usually in association with QT prolongation (torsades de pointes), but sometimes without documented QT prolongation. In registration studies, these arrhythmias, which require cardioversion, occurred in 1.7% of treated patients during, or within a number of hours of, use of Covert. These arrhythmias can be reversed if treated promptly. It is essential that Covert be administered in a setting of continuous ECG monitoring and by personnel trained in identification and treatment of acute ventricular arrhythmias, particularly polymorphic ventricular tachycardia. Patients with atrial fibrillation of more than 2 to 3 days' duration must be adequately anticoagulated, generally for at least 2 weeks. CHOICE OF PATIENTS. Patients with chronic atrial fibrillation have a strong tendency to revert after conversion to sinus rhythm and treatments to maintain sinus rhythm carry risks. Patients to be treated with Covert, therefore, should be carefully selected such that the expected benefits of maintaining sinus rhythm outweigh the immediate risks of Covert, and the risks of maintenance therapy, and are likely to offer an advantage compared with alternative management. Patients with chronic atrial fibrillation have a strong tendency to revert after conversion to sinus rhythm and treatments to maintain sinus rhythm carry risks. Patients to be treated with ibutilide fumarate injection, therefore, should be carefully selected such that the expected benefits of maintaining sinus rhythm outweigh the immediate risks of ibutilide fumarate injection, and the risks of maintenance therapy, and are likely to offer an advantage compared with alternative management. Clinical trials with ibutilide fumarate injection in patients with atrial fibrillation and atrial flutter did not include anyone under the age of 18. Safety and effectiveness of ibutilide in pediatric patients has not been established. FDA Pregnancy Risk Category: C /RISK CANNOT BE RULED OUT. Adequate, well controlled human studies are lacking, and animal studies have shown risk to the fetus or are lacking as well. There is a chance of fetal harm if the drug is given during pregnancy; but the potential benefits may outweigh the potential risk./ For more Drug Warnings (Complete) data for Ibutilide (11 total), please visit the HSDB record page. Pharmacodynamics Ibutilide prolongs the action potential duration and increases both atrial and ventricular refractoriness in vivo, i.e., class III electrophysiologic effects. Voltage clamp studies indicate that ibutilide, at nanomolar concentrations, delays repolarization by activation of a slow, inward current (predominantly sodium), rather than by blocking outward potassium currents, which is the mechanism by which most other class III antiarrhythmics act. |
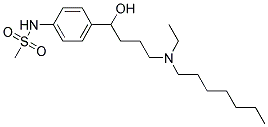
| 分子式 |
C20H36N2O3S
|
|---|---|
| 分子量 |
384.57644
|
| 精确质量 |
384.245
|
| CAS号 |
122647-31-8
|
| 相关CAS号 |
Ibutilide fumarate;122647-32-9
|
| PubChem CID |
60753
|
| 外观&性状 |
Colorless to light yellow oil
|
| 密度 |
1.099g/cm3
|
| 沸点 |
522.4ºC at 760mmHg
|
| 闪点 |
269.7ºC
|
| 蒸汽压 |
9.71E-12mmHg at 25°C
|
| LogP |
5.317
|
| tPSA |
78.02
|
| 氢键供体(HBD)数目 |
2
|
| 氢键受体(HBA)数目 |
5
|
| 可旋转键数目(RBC) |
14
|
| 重原子数目 |
26
|
| 分子复杂度/Complexity |
443
|
| 定义原子立体中心数目 |
0
|
| InChi Key |
ALOBUEHUHMBRLE-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C20H36N2O3S/c1-4-6-7-8-9-16-22(5-2)17-10-11-20(23)18-12-14-19(15-13-18)21-26(3,24)25/h12-15,20-21,23H,4-11,16-17H2,1-3H3
|
| 化学名 |
N-[4-[4-[ethyl(heptyl)amino]-1-hydroxybutyl]phenyl]methanesulfonamide
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 2.6002 mL | 13.0012 mL | 26.0024 mL | |
| 5 mM | 0.5200 mL | 2.6002 mL | 5.2005 mL | |
| 10 mM | 0.2600 mL | 1.3001 mL | 2.6002 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。