| 规格 | 价格 | |
|---|---|---|
| 500mg | ||
| 1g | ||
| Other Sizes |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Absorbed following oral administration. A pharmacokinetic study with mianserin HCl was performed in six healthy male subjects. The subjects were treated on different occasions intravenously with a constant-rate infusion of 5 mg mianserin HCl in 1 hr, orally with a single dose of 60 mg as two tablets of 30 mg each and with 60 mg as an oral solution. The wash-out period between treatments was 1 month. Blood samples were taken at predetermined times over a period of 120 hr following dosing. The mianserin concentration in the plasma samples was determined and the results were pharmacokinetically analyzed. The intravenous data could be adequately described by a 3-compartment model and the oral data by a 2-compartment model, both with first-order transfer and elimination rate constants. The mean plasma clearance of mianserin was found to be 19 +/- 2 L/hr (mean +/- SEM), the kinetic volume of distribution 444 +/- 250 L, the steady-state volume of distribution 242 +/- 171 L and the elimination half-life 33 +/- 5 hr. The absolute bioavailability in terms of extent of absorption was 22 +/- 3% for the solution and 20 +/- 3% for the tablets. The mean peak level for the solution was 79 +/- 11 ng/mL and for the tablets 54 +/- 5 ng /mL; mean peak time for the solution was 1.1 +/- 0.2 hr and for the tablets 1.4 +/- 0.2 hr. The mean absorption half-life for the solution was 0.43 +/- 0.13 hr and for the tablets 0.39 +/- 0.11 hr. We studied mianserin kinetics after a single (60 mg) dose in eight inpatients suffering from depression. There was a considerable interpatient variability in plasma levels. Mean peak plasma levels (+/- SEM) were 114 +/- 26 ng/ml and were reached between 1 and 3 hr. The decline of mianserin levels in plasma was biphasic. The mean elimination t 1/2 was 21.6 +/- 3.1 hr and ranged from 10.7 to 40.8 hr. The estimated first-pass loss ranged from 26% to 48% (mean, 37%) and was lower than that reported for tertiary amine tricyclic antidepressants. The mean apparent volume of distribution (15.7 +/- 2.2 L/kg; 9.7 to 28.8 L/kg) was in the range of that for imipramine but somewhat lower than for maprotiline. Apparent total body clearance ranged from 0.33 to 0.81 L/hr/kg (mean +/- SEM, 0.52 +/- 0.05 L/hr/kg) and was of the order of that after maprotiline. Our results indicate that mianserin kinetics are in most respects similar to those of tertiary amine tricyclic antidepressants (e.g., imipramine) and the tetracyclic maprotiline. Metabolism / Metabolites Hepatic. Mianserin metabolism was studied in female humans, rabbits, and rats. ... In human females, unchanged mianserin, 8-hydroxymianserin and mianserin-2-oxide were isolated and identified in urine. The two metabolites were over 60 percent of the total urinary radioactivity; conjugated and unconjugated mianserin accounted for approximately 35 percent. In rabbits, mianserin was metabolized largely as 8-hydroxymianserin and an unidentified ester of 8-hydroxymianserin; only about 2.4 percent was unchanged mianserin. Small amounts of 2-formyldesmethylmianserin were isolated. The principal metabolite in rats was 8-hydroxydesmethylmianserin. Rats metabolized mianserin principally to 8-hydroxy compounds and to a lesser extent to demethylated metabolites. The authors conclude that mianserin is metabolized by three main pathways: 8-hydroxylation, demethylation, and 2-oxide formation. /Mianserin HCl/ To measure steady-state plasma concentrations of mianserin and its major active metabolite, desmethylmianserin, and to analyze the effects of various clinical factors on these plasma concentrations, steady-state plasma concentrations of mianserin and desmethylmianserin were measured in 76 depressed patients, ages 20-70 yr, receiving 30 mg/day mianserin at bedtime for 3 wk with doses increased up to 60 mg/day if needed. There were considerable interindividual variations in the steady-state plasma concentrations of these compounds; the plasma concentrations of mianserin plus desmethylmianserin were within the therapeutic range in only 43% of the patients. With advancing age, the plasma concentrations of mianserin increased significantly, while those of mianserin plus desmethylmianserin remained unchanged. Sex, smoking, and coadministration of benzodiazepines did not affect the drug's metabolism. There was no evidence that the kinetics of these compounds were nonlinear with increasing doses. Mianserine has known human metabolites that include 8-Hydroxymianserin, Desmethylmianserin, and Mianserin N-oxide. Biological Half-Life 10-17 hours The pharmacokinetics of mianserin hydrochloride have been determined in eight normal healthy volunteers, mean age 27, and 14 elderly patients, mean age 76. Mianserin was administered to volunteers by intravenous infusion (0.011 mg/kg/min for 15 min) and, on another occasion, by mouth, in a single dose of 30 mg. Elderly patients received a single oral dose of 40-60 mg. The terminal elimination half-life was significantly prolonged in the elderly. In young subjects it was 9.6 +/- 1.9 (s.d.) hr. In the elderly it was 27 +/- 13.1 (s.d.) hr. Apparent oral clearance was significantly reduced in the elderly. In young subjects it was 87.1 +/- 32 (s.d.) hr. In the elderly, it was 38.1 +/- 14.8 (s.d.) hr. These kinetic differences may have an important bearing on the sedative effects of mianserin. |
|---|---|
| 毒性/毒理 (Toxicokinetics/TK) |
Effects During Pregnancy and Lactation
◉ Summary of Use during Lactation Mianserin is not approved for marketing in the United States by the U.S. Food and Drug Administration, but is available in other countries. Limited information indicates that maternal doses up to 60 mg daily produce low levels in milk and would not be expected to cause any adverse effects in breastfed infants, especially if the infant is older than 2 months. Until more data are available, mianserin should be used with careful monitoring during breastfeeding. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk An observational study looked at outcomes of 2859 women who took an antidepressant during the 2 years prior to pregnancy. Compared to women who did not take an antidepressant during pregnancy, mothers who took an antidepressant during all 3 trimesters of pregnancy were 37% less likely to be breastfeeding upon hospital discharge. Mothers who took an antidepressant only during the third trimester were 75% less likely to be breastfeeding at discharge. Those who took an antidepressant only during the first and second trimesters did not have a reduced likelihood of breastfeeding at discharge. The antidepressants used by the mothers were not specified. A retrospective cohort study of hospital electronic medical records from 2001 to 2008 compared women who had been dispensed an antidepressant during late gestation (n = 575) to those who had a psychiatric illness but did not receive an antidepressant (n = 1552) and mothers who did not have a psychiatric diagnosis (n = 30,535). Women who received an antidepressant were 37% less likely to be breastfeeding at discharge than women without a psychiatric diagnosis, but no less likely to be breastfeeding than untreated mothers with a psychiatric diagnosis. None of the mothers were taking mianserin. In a study of 80,882 Norwegian mother-infant pairs from 1999 to 2008, new postpartum antidepressant use was reported by 392 women and 201 reported that they continued antidepressants from pregnancy. Compared with the unexposed comparison group, late pregnancy antidepressant use was associated with a 7% reduced likelihood of breastfeeding initiation, but with no effect on breastfeeding duration or exclusivity. Compared with the unexposed comparison group, new or restarted antidepressant use was associated with a 63% reduced likelihood of predominant, and a 51% reduced likelihood of any breastfeeding at 6 months, as well as a 2.6-fold increased risk of abrupt breastfeeding discontinuation. Specific antidepressants were not mentioned. Protein Binding 90% |
| 参考文献 | |
| 其他信息 |
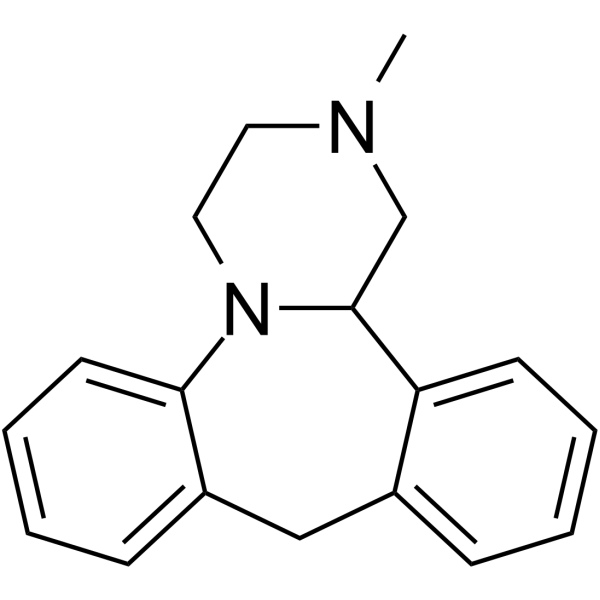
Mianserin is a dibenzoazepine (specifically 1,2,3,4,10,14b-hexahydrodibenzo[c,f]pyrazino[1,2-a]azepine) methyl-substituted on N-2. Closely related to (and now mostly superseded by) the tetracyclic antidepressant mirtazapinean, it is an atypical antidepressant used in the treatment of depression throughout Europe and elsewhere. It has a role as an antidepressant, a histamine agonist, a sedative, an alpha-adrenergic antagonist, an adrenergic uptake inhibitor, a serotonergic antagonist, a H1-receptor antagonist, an EC 3.4.21.26 (prolyl oligopeptidase) inhibitor and a geroprotector.
A tetracyclic compound with antidepressant effects. Mianserin was previously available internationally, however in most markets it has been phased out in favour of [mirtazapine]. A tetracyclic compound with antidepressant effects. It may cause drowsiness and hematological problems. Its mechanism of therapeutic action is not well understood, although it apparently blocks alpha-adrenergic, histamine H1, and some types of serotonin receptors. Drug Indication For the treatment of depression. Mechanism of Action Mianserin's mechanism of therapeutic action is not well understood, although it apparently blocks alpha-adrenergic, histamine H1, and some types of serotonin receptors. |
| 分子式 |
C18H20N2
|
|---|---|
| 分子量 |
264.3648
|
| 精确质量 |
264.163
|
| CAS号 |
24219-97-4
|
| 相关CAS号 |
Mianserin hydrochloride;21535-47-7
|
| PubChem CID |
4184
|
| 外观&性状 |
Typically exists as solid at room temperature
|
| 密度 |
1.18g/cm3
|
| 沸点 |
411.3ºC at 760mmHg
|
| 闪点 |
186.1ºC
|
| LogP |
3.086
|
| tPSA |
6.48
|
| 氢键供体(HBD)数目 |
0
|
| 氢键受体(HBA)数目 |
2
|
| 可旋转键数目(RBC) |
0
|
| 重原子数目 |
20
|
| 分子复杂度/Complexity |
342
|
| 定义原子立体中心数目 |
0
|
| SMILES |
CN(CC1)CC2N1C3=CC=CC=C3CC4=CC=CC=C24
|
| InChi Key |
UEQUQVLFIPOEMF-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C18H20N2/c1-19-10-11-20-17-9-5-3-7-15(17)12-14-6-2-4-8-16(14)18(20)13-19/h2-9,18H,10-13H2,1H3
|
| 化学名 |
5-methyl-2,5-diazatetracyclo[13.4.0.02,7.08,13]nonadeca-1(19),8,10,12,15,17-hexaene
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 3.7827 mL | 18.9136 mL | 37.8272 mL | |
| 5 mM | 0.7565 mL | 3.7827 mL | 7.5654 mL | |
| 10 mM | 0.3783 mL | 1.8914 mL | 3.7827 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。