| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 50mg |
|
||
| 100mg |
|
||
| 250mg |
|
||
| 500mg |
|
||
| 1g |
|
||
| Other Sizes |
| 靶点 |
MAO (monoamine oxidase)
1. Peroxynitrite (ONOO⁻)-mediated oxidative stress pathways [1] 2. Cell adhesion molecule L1 (mimics L1 function [2] |
|---|---|
| 体外研究 (In Vitro) |
过氧亚硝酸盐是血管内室中由超氧化物阴离子和一氧化氮产生的一种活性氮。过氧亚硝酸盐破坏血浆蛋白、红细胞和血小板的膜。这就解释了为什么过亚硝酸盐的过量生产会导致疾病和衰老。拮抗过氧亚硝酸盐的治疗方法可以延缓衰老和疾病进展。我们开发了一种体外测定法,可以研究过氧亚硝酸盐在血管内室中引起的氧化损伤。该测定将损伤与蛋白质羰基、3-硝基酪氨酸(3-NT)和硫代巴比妥酸反应物质的形成速率相关联。使用该测定法,我们评估了酚嗪(一种活性醛的清除剂)拮抗过氧亚硝酸盐作用的能力。在此,我们发现吩噻嗪显著降低了血浆和血小板中过氧亚硝酸盐引起的脂质过氧化损伤。此外,它还抑制了血浆和血小板蛋白中羰基和3-NT的形成。
1. 在经过氧亚硝酸盐(ONOO⁻,50 μM)处理的人血浆样本中,苯乙肼(Phenelzine)(10、50、100 μM)以浓度依赖性方式减轻氧化损伤:100 μM浓度下,与ONOO⁻处理对照组相比,脂质过氧化(以丙二醛MDA衡量)降低65%,蛋白羰基化(蛋白质氧化标志物)降低58%。[1] 2. 在小鼠神经母细胞瘤N2a细胞中,苯乙肼(Phenelzine)(5、10、20 μM)模拟L1功能:增加细胞黏附(20 μM时黏附细胞数较对照组增加2.3倍)并促进细胞存活(MTT实验显示20 μM时细胞活力为85%,而L1缺陷对照组为60%);Western blot检测显示其上调L1下游信号分子(如FAK、ERK1/2)的表达。[2] |
| 体内研究 (In Vivo) |
在小鼠中,与媒介物对照治疗的小鼠相比,在严重胸部压迫后立即腹膜内注射酚嗪,此后每天注射一次,持续6周,在脊髓损伤后4周和5周改善后肢功能,减少星形胶质细胞增生,促进轴突再生/发芽。Phenelzine的应用上调了脊髓中L1的表达,并刺激了脊髓组织中同源L1介导的细胞内信号级联。在炎症的急性期,经吩嗪治疗的小鼠损伤脊髓中的促炎细胞因子水平降低,如白细胞介素-1β、白细胞介素-6和肿瘤坏死因子-α[2]。
在T10脊髓挫伤损伤的C57BL/6小鼠中:苯乙肼(Phenelzine)(10 mg/kg,腹腔注射,每日1次,持续28天)促进功能恢复。苯乙肼处理组的BBB(Basso-Beattie-Bresnahan)运动功能评分从损伤后1天的3.2升至28天的11.5,而溶剂对照组从3.0升至7.8。组织学分析显示,损伤部位轴突密度(NF200阳性轴突)增加40%,胶质瘢痕形成(GFAP阳性星形胶质细胞)减少35%。[2] |
| 酶活实验 |
这项研究开发了一种体外测定法,可以研究过氧亚硝酸盐在血管内室中引起的氧化损伤。该测定将损伤与蛋白质羰基、3-硝基酪氨酸(3-NT)和硫代巴比妥酸反应物质的形成速率相关联。使用该测定法,本研究评估了酚嗪(一种活性醛的清除剂)拮抗过氧亚硝酸盐作用的能力。在此,本研究表明,吩噻嗪可显著降低血浆和血小板中过氧亚硝酸盐引起的脂质过氧化损伤[1]。
制备人血浆样本(PBS 1:10稀释),将血浆与苯乙肼(Phenelzine)(10、50、100 μM)在37°C孵育30分钟,随后加入过氧亚硝酸盐(50 μM)继续孵育1小时。检测抗氧化酶活性:采用比色法(560 nm吸光度)检测超氧化物歧化酶(SOD)活性,通过检测NADPH氧化(340 nm吸光度)检测谷胱甘肽过氧化物酶(GSH-Px)活性。与ONOO⁻处理对照组相比,100 μM苯乙肼使SOD活性增加42%,GSH-Px活性增加38%。[1] |
| 细胞实验 |
1. N2a细胞黏附实验:将N2a细胞(5×10⁴细胞/孔)接种于多聚赖氨酸预包被的24孔板,用苯乙肼(Phenelzine)(5、10、20 μM)处理后37°C孵育2小时。PBS洗涤未黏附细胞,4%多聚甲醛固定,结晶紫染色,显微镜下计数黏附细胞数。[2]
2. N2a细胞存活实验:将N2a细胞(1×10⁴细胞/孔)接种于96孔板,用苯乙肼(Phenelzine)(5、10、20 μM)处理48小时。加入MTT试剂(5 mg/mL)孵育4小时,DMSO溶解甲臜结晶,检测570 nm吸光度计算细胞活力。[2] 3. L1信号通路Western blot实验:裂解苯乙肼处理的N2a细胞,提取总蛋白并进行SDS-PAGE电泳,转印至PVDF膜,用抗FAK、磷酸化FAK(p-FAK)、ERK1/2、磷酸化ERK1/2(p-ERK1/2)及β-肌动蛋白(内参)抗体孵育,化学发光法检测信号并量化条带强度。[2] |
| 动物实验 |
In mice, intraperitoneal injection of phenelzine immediately after severe thoracic compression, and thereafter once daily for 6 weeks, improved hind limb function, reduced astrogliosis and promoted axonal regrowth/sprouting at 4 and 5 weeks after spinal cord injury compared to vehicle control-treated mice[2].
1. Spinal cord injury (SCI) model: Male C57BL/6 mice (8–10 weeks old) were anesthetized, and T10 spinal cord contusion injury was induced using an Infinite Horizon impactor (100 kdyn force). [2] 2. Grouping and treatment: Mice were randomized into vehicle control (0.9% saline + 1% DMSO) and Phenelzine groups. Phenelzine was dissolved in 0.9% saline + 1% DMSO and administered via intraperitoneal injection at 10 mg/kg once daily, starting 1 hour post-injury and continuing for 28 days. [2] 3. Outcome detection: BBB locomotor scores were evaluated every 7 days. On day 28, mice were sacrificed, spinal cords were harvested, fixed in 4% paraformaldehyde, sectioned, and stained with NF200 (axon marker) and GFAP (astrocyte marker) for histological analysis. [2] |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Phenelzine is rapidly absorbed from the gastrointestinal tract. The decay of the drug action is not dependent on the pharmacokinetic parameters but on the rate of protein synthesis which restores the functional levels of monoamine oxidase. The mean Cmax is 19.8 ng/ml and it occurs after 43 minutes of dose administration. The elimination of the administered dose is mainly composed of the phenelzine metabolites, phenylacetic acid and parahydroxyphenylacetic acid that constitute 79% of the dose found in the urine in the first 96 hours. The volume of distribution of phenelzine is hard to determine as drugs from this kind penetrate the CNS very well into the tissue where their activity is desired. Following ip injection of 2.5 mg/kg bw phenelzine-1-(14)C sulfate to rats, 62% of the dose was recovered in the urine within 24 hours. Following a single 30 mg dose of Nardil (2 X 15 mg tablets), a mean peak plasma concentration (Cmax) of 19.8 ng/mL occurred at a time (Tmax) of 43 minutes post dose. Phenelzine is readily absorbed from the gastrointestinal tract. There is little excretion in the urine. Metabolism / Metabolites For the metabolic studies, it is assumed that phenelzine is acetylated. Some of the metabolites of phenelzine are phenylacetic acid, 2-phenylethylamine and 4-hydroxyphenylacetic acid as major metabolites and N-acetyl-phenelzine as a minor metabolite. Nardil is extensively metabolized, primarily by oxidation via monoamine oxidase. After oral administration of (13)C6-phenelzine, 73% of the administered dose was recovered in urine as phenylacetic acid and parahydroxyphenylacetic acid within 96 hours. Acetylation to N2-acetylphenelzine is a minor pathway. Following ip injection of 2.5 mg/kg bw phenelzine-1-(14)C sulfate to rats, 62% of the dose was recovered in the urine within 24 hours. The major excretion product was phenylacetic acid, which is also a metabolite of phenelzine in mice. The first enzyme involved in this elimination process is monoamine oxidase. Hepatic. Acetylation of phenelzine appears to be a minor metabolic pathway. Beta-phenylethylamine is a metabolite of phenelzine, and there is indirect evidence that phenelzine may also be ring-hydroxylated and N-methylated. Route of Elimination: NARDIL® is extensively metabolized, primarily by oxidation via monoamine oxidase. Half Life: 1.2-11.6 hours following single dose administration. Multiple-dose pharmacokinetics have not been studied. Biological Half-Life After administration phenelzine presents a very short half-life of 11.6 hours in humans. The mean apparent half-life, estimated from urinary excretion data in patients who received oral doses of 30 mg thrice daily, was 0.87 hours following the initial dose and 3.11 hours after 13 days of treatment. The mean elimination half-life after a single 30 mg dose is 11.6 hours. |
| 毒性/毒理 (Toxicokinetics/TK) |
Toxicity Summary
Although the exact mechanism of action has not been determined, it appears that the irreversible, nonselective inhibition of MAO by phenelzine relieves depressive symptoms by causing an increase in the levels of serotonin, norepinephrine, and dopamine in the neuron. Hepatotoxicity Phenelzine, like most monoamine oxidase inhibitors, can cause transient serum aminotransferase elevations in a proportion of patients. These elevations are usually mild, asymptomatic and self-limited and do not require dose modification. Phenelzine has also been associated with cases of acute, clinically apparent liver injury. The liver injury associated with MAO inhibitors typically arises 1 to 3 months after starting therapy and presents with a hepatocellular pattern of serum enzyme elevations. The acute hepatitis-like syndrome can be severe and even fatal. Cholestatic liver injury due to phenelzine has also been described (Case 1). Immunoallergic features (rash, fever, eosinophilia) are uncommon as is autoantibody formation. While few cases of phenelzine liver injury have been published, instances of severe jaundice and fatalities due to liver injury have been reported to the FDA and the sponsor. Likelihood score: C (probable rare cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Because of the lack of data on use during breastfeeding, other antidepressants are preferred during breastfeeding. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Phenelzine can elevate serum prolactin in some patients and has caused galactorrhea in nonpregnant, nonnursing patients. The clinical relevance of these findings in nursing mothers is not known. The prolactin level in a mother with established lactation may not affect her ability to breastfeed. Protein Binding Unchanged phenelzine presents a high protein binding which reduced its bioavailability. Interactions MAO inhibitors, including Nardil, are contraindicated in patients receiving guanethidine. Patients taking Nardil should not undergo elective surgery requiring general anesthesia. Also, they should not be given cocaine or local anesthesia containing sympathomimetic vasoconstrictors. The possible combined hypotensive effects of Nardil and spinal anesthesia should be kept in mind. Nardil should be discontinued at least 10 days prior to elective surgery. The concurrent administration of an MAO inhibitor and bupropion hydrochloride is contraindicated. At least 14 days should elapse between discontinuation of an MAO inhibitor and initiation of treatment with bupropion hydrochloride. /MAO inhibitors/ The combination of MAO inhibitors and tryptophan has been reported to cause behavioral and neurologic syndromes including disorientation, confusion, amnesia, delirium, agitation, hypomanic signs, ataxia, myoclonus, hyperreflexia, shivering, ocular oscillations, and Babinski signs. /MAO inhibitors/ For more Interactions (Complete) data for Phenelzine (9 total), please visit the HSDB record page. Non-Human Toxicity Values LD50 Mouse iv 160 mg/kg body weight LD50 Mouse oral 160 mg/kg body weight LD50 Mouse ip 135 mg/kg body weight LD50 Rat oral 210 mg/kg body weight In the spinal cord injury mouse model, Phenelzine (10 mg/kg, intraperitoneal injection for 28 days) did not cause significant toxicity: no abnormal weight loss (body weight change ±5% vs control), and histological examination of liver and kidney showed no obvious pathological damage (e.g., hepatocyte necrosis, renal tubular injury). [2] |
| 参考文献 |
[1]. Phenelzine reduces the oxidative damage induced by peroxynitrite in plasma lipids and proteins. Arch Physiol Biochem. 2018 Dec;124(5):418-423.
[2]. Phenelzine, a small organic compound mimicking the functions of cell adhesion molecule L1, promotes functional recovery after mouse spinal cord injury. Restor Neurol Neurosci . 2018;36(4):469-483. |
| 其他信息 |
Therapeutic Uses
Antidepressive Agents, Monoamine Oxidase Inhibitors Phenelzine is used in the treatment of major depressive disorder. /Included in US product label/ Phenelzine has been used with some success in the management of bulimia nervosa. /NOT included in US product label/ Nardil should rarely be the first antidepressant drug used. Rather, it is more suitable for use with patients who have failed to respond to the drugs more commonly used for these conditions. Nardil has been found to be effective in depressed patients clinically characterized as "atypical," "nonendogenous," or "neurotic." These patients often have mixed anxiety and depression and phobic or hypochondriacal features. There is less conclusive evidence of its usefulness with severely depressed patients with endogenous features. Drug Warnings /BOXED WARNING/ Suicidality and Antidepressant Drugs: Antidepressants increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of Nardil or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction in risk with antidepressants compared to placebo in adults aged 65 and older. Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients of all ages who are started on antidepressant therapy should be monitored appropriately and observed closely for clinical worsening, suicidality, or unusual changes in behavior. Families and caregivers should be advised of the need for close observation and communication with the prescriber. Nardil is not approved for use in pediatric patients. Safety and efficacy of phenelzine in pediatric patients have not been established. The US Food and Drug Administration (FDA) has determined that antidepressants increase the risk of suicidal thinking and behavior (suicidality) in children and adolescents with major depressive disorder and other psychiatric disorders. However, FDA also states that depression and certain other psychiatric disorders are themselves associated with an increased risk of suicide. Anyone considering the use of phenelzine in a child or adolescent for any clinical use must balance the potential risk of therapy with the clinical need. Phenelzine shares the toxic potentials of other MAO inhibitors, and the usual precautions and contraindications associated with these drugs should be observed. Patients should be fully advised about the risks, especially hypertensive crisis and suicidal thinking and behavior (suicidality), associated with MAO inhibitor therapy. Nardil should not be used in patients who are hypersensitive to the drug or its ingredients, with pheochromocytoma, congestive heart failure, severe renal impairment or renal disease, a history of liver disease, or abnormal liver function tests. For more Drug Warnings (Complete) data for Phenelzine (19 total), please visit the HSDB record page. Pharmacodynamics The elimination of monoamine oxidase by phenelzine results in the elevation of brain amines such as 2-phenylethylamine which is a metabolite of phenelzine. These amines have then marked effects on the uptake and release of catecholamines and serotonin in nerve endings. Phenelzine is shown to elevate brain levels of the gamma-aminobutyric acid (GABA) and alanine (ALA) as well as to inhibit the activity of the transaminases that normally metabolize these amino acids. In preclinical studies, it has been shown to be neuroprotective in cerebral ischemia. 1. Phenelzine exerts antioxidant effects by scavenging peroxynitrite (ONOO⁻) and enhancing antioxidant enzyme activity, thereby reducing ONOO⁻-induced oxidative damage to plasma lipids and proteins. [1] 2. Phenelzine is a small-molecule mimetic of cell adhesion molecule L1; it activates L1-mediated signaling pathways (FAK/ERK) to promote neural cell adhesion, survival, and axon regeneration, facilitating functional recovery after spinal cord injury. [2] |
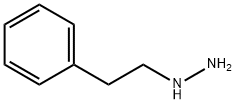
| 分子式 |
C8H12N2
|
|---|---|
| 分子量 |
136.20
|
| 精确质量 |
136.1
|
| 元素分析 |
C, 70.55; H, 8.88; N, 20.57
|
| CAS号 |
51-71-8
|
| 相关CAS号 |
51-71-8; 156-51-4 (sulfate);
|
| PubChem CID |
3675
|
| 外观&性状 |
Liquid
|
| 密度 |
1.0±0.1 g/cm3
|
| 沸点 |
281.4±19.0 °C at 760 mmHg
|
| 熔点 |
157-161ºC
Crystals; mp: 174 °C /Phenelzine hydrochloride/ < 25 °C |
| 闪点 |
143.7±25.1 °C
|
| 蒸汽压 |
0.0±0.6 mmHg at 25°C
|
| 折射率 |
1.550
|
| LogP |
1.14
|
| tPSA |
38.05
|
| 氢键供体(HBD)数目 |
2
|
| 氢键受体(HBA)数目 |
2
|
| 可旋转键数目(RBC) |
3
|
| 重原子数目 |
10
|
| 分子复杂度/Complexity |
77.3
|
| 定义原子立体中心数目 |
0
|
| SMILES |
NNCCC1=CC=CC=C1
|
| InChi Key |
RMUCZJUITONUFY-UHFFFAOYSA-N
|
| InChi Code |
InChI=1S/C8H12N2/c9-10-7-6-8-4-2-1-3-5-8/h1-5,10H,6-7,9H2
|
| 化学名 |
Hydrazine, (2-phenylethyl)-
|
| 别名 |
Phenelzine; 51-71-8; Phenethylhydrazine; 2-Phenylethylhydrazine; Nardil; Fenelzyne; Hydrazine, (2-phenylethyl)-; Fenelzyna;
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 7.3421 mL | 36.7107 mL | 73.4214 mL | |
| 5 mM | 1.4684 mL | 7.3421 mL | 14.6843 mL | |
| 10 mM | 0.7342 mL | 3.6711 mL | 7.3421 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。