| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 5mg |
|
||
| 10mg |
|
||
| 50mg |
|
||
| 100mg |
|
||
| Other Sizes |
|
| 靶点 |
Glucagon-like peptide-1 receptor (GLP-1R)
|
|---|---|
| 体外研究 (In Vitro) |
Orforglipron是一种肠促胰岛素,由小肠L细胞在营养物质通过消化道时产生,葡萄糖通过GLP-1受体给予。Orforglipron具有多种作用,包括延迟胃排空和抑制食物摄入[1]。
在这项研究中,研究人员报告了非肽GLP-1R激动剂LY3502970(OWL833)的发现和作用机制。LY3502970是一种部分激动剂,偏向于G蛋白激活,而不是GLP-1R上的β-arrestin募集。该分子对其他B类G蛋白偶联受体(GPCR)具有高度的效力和选择性,其药代动力学特征有利于口服给药。LY3502970与活性状态GLP-1R复合物的高分辨率结构揭示了上螺旋束中一个独特的结合囊,该化合物在其中被细胞外结构域(ECD)、细胞外环2和跨膜螺旋1、2、3和7结合。这种机制产生了一种独特的受体构象,可以解释化合物的部分激动作用和偏置信号。此外,LY3502970和ECD的灵长类特异性Trp33之间的相互作用告知了该分子的物种选择性活性[2]。 |
| 体内研究 (In Vivo) |
Orforglipron半钙水合物(血浆浓度0.94-4.8 nM,静脉注射30分钟;或0.05-0.1 mg/mL,灌胃,5天)在动物模型食蟹猴中呈剂量依赖性地抑制食物摄入、促进胰岛素分泌和降低血糖[1]。Orforglipron半钙水合物(0.05-1.35 mg/kg,灌胃)给药后2小时达Cmax,血浆药物暴露量的增加与剂量的增加大致成正比,表明Orforglipron半钙水合物以剂量依赖性方式在胃肠道吸收[1]。奥格列酮半钙水合物在食蟹猴体内的药代动力学分析[1] 途径 剂量 (mg/kg) Tmax (h) Cmax (ng/mL) AUC0-24h (ng·h/mL) ig 0.05 2.0 4.78 23.7 ig 0.15 2.0 20.7 135 ig 0.45 2.0 32.0 208 ig 1.35 2.0 148 1040.
在疗效研究中,口服LY3502970可降低人源化GLP-1R转基因小鼠的血糖,并对非人灵长类动物产生促胰岛素和低血糖作用,表明两种模型的作用大小与注射用艾塞那肽相当。这项工作共同确定了正在开发的用于治疗2型糖尿病的口服药物活性的分子基础,为非肽配体激活B类GPCR提供了见解。[2] 食蟹猴的药代动力学和功能。除了作为强效的Gs激活剂外,非肽GLP-1R激动剂还必须具有能够口服给药的药代动力学特性。因此,通过静脉注射或口服该化合物的研究,确定了LY3502970在大鼠和食蟹猴体内的药代动力学特征。大鼠(n=4)口服给药后的消除半衰期(T1/2)为10.4至12.4小时,食蟹猴(n=4,n=4)为3.4至4.6小时,经计算口服生物利用度分别为33%至43%和21%至28%。这与迄今为止批准的唯一一种肽GLP-1R激动剂片剂在人体内报告的0.4%至1%的口服生物利用度形成鲜明对比。这些数据表明,在没有基于肽的GLP-1R激动剂所需的复杂口服制剂的情况下,口服LY3502970可能是可行的[2]。 由于Trp33ECD在猴子GLP-1R中的存在以及该物种良好的药代动力学数据,在食蟹猴中测试了LY3502970,以评估该化合物增强葡萄糖刺激的胰岛素分泌和减少食物摄入的能力,这两者都是GLP-1R激动症的治疗标志。进行静脉葡萄糖耐量试验(IVGTT)以评估LY3502970增强胰岛素分泌的能力。静脉注射该化合物或艾塞那肽,然后持续输注,以在测试期间保持稳定的药物浓度。输注LY3502970或艾塞那肽40分钟后给予葡萄糖(图5A)。在葡萄糖给药之前,LY3502970和艾塞那肽均未刺激胰岛素分泌。葡萄糖输注后,载体处理对照组的血糖浓度升高,然后随着时间的推移逐渐下降。血清胰岛素水平略有升高,并在40分钟内保持升高状态。在实验期间,用LY3502970或艾塞那肽治疗显著增加了胰岛素浓度并降低了血糖(图5 B-E)。高剂量LY3502970(稳态浓度:9.1±0.8 nmol/L;平均值±SEM,n=7)对胰岛素分泌的影响与高剂量艾塞那肽(43.0±4.1 pmol/L;平均值?SEM,n=6)刺激的胰岛素分泌相当。这些结果表明,LY3502970可以通过促胰岛素机制降低高血糖,其程度与艾塞那肽相似[2]。 |
| 酶活实验 |
体外药理学。进行了cAMP积累、β-arrestin募集和受体结合试验,根据已发表方法: Nat. Commun. 7, 13384 (2016) and Nat. Chem. Biol. 16, 1105–1110 (2020).
|
| 动物实验 |
Animal/Disease Models:cynomolgus monkey model[1]
Doses: 0.9-4.8 nM; or 0.05-0.1 mg/mL Route of Administration: continuous i.v. administration for 30 minutes until a plasma concentration of 0.9-4.8 nM at steady state; i.g. for 5 days with dose of 0.05-0.1 mg/mL Experimental Results: Increased insulin secretion and decreased plasma-glucose. Suppressed food intake in a dose-dependent manner. Compound Formulation. LY3502970 was prepared in 10% polyethylene glycol 400 (PEG400)/10% propylene glycol (PG)/80% glycine buffer (100 mM glycine, 64 mM NaOH, pH 10) buffer. Exenatide was prepared in phosphate-buffered saline (PBS) containing 0.05 wt/vol% Tween80 buffer. The vehicle solutions without the test articles were used as controls.[2] Pharmacokinetics. [2] LY3502970 was administered orally at doses of 0.05, 0.15, or 0.45 mg/kg or i.v. at 0.15 mg/kg to 8-wk-old male rats (n = 4 rats/group) or oral doses of 0.04, 0.12, or 0.36 mg/kg or i.v. at 0.12 mg/kg to 3-y-old male cynomolgus monkeys (n = 4 monkeys/group). Blood was collected predose and 30 min and 1, 2, 3, 4, 6, 8, 12, 16, and 24 h after administration in orally dosing group. Blood samples were also collected predose and 2, 10, and 30 min and 1, 2, 4, 8, 12, 16, and 24 h after i.v. administration. Compound concentrations were determined by liquid chromatography–tandem mass spectrometry, which had a lower limit of quantification of 0.1 ng/mL. Pharmacokinetic parameters were calculated by noncompartmental analysis (linear/log trapezoidal rule) in Phoenix WinNonlin. Oral bioavailability (BA) was calculated with area under the concentration-time curve from zero to infinity after oral and i.v. administration by BA (%) = AUCinf, by mouth, orally (p.o.)/AUCinf, i.v. × 100.[2] Glucose Tolerance Tests. [2] Mice fasted overnight were orally dosed with vehicle or LY3502970, followed 5 h later by an intraperitoneal injection of glucose (2 g/kg). Blood glucose concentrations were measured over time up to 120 min after glucose administration using glucometers. Data were used to calculate the area under the curve (AUC) (n = 5 mice/group). Male cynomolgus monkeys (3.9 to 7.5 kg) were administered atropine sulfate i.v. (0.5 mg Tanabe, 0.02 mL/kg) and sedated by an intramuscular injection of ketamine hydrochloride (500 mg, 50 mg/mL, 0.2 mL/kg). Animals were then anesthetized by inhalation of isoflurane (Isoflu, 0.5 to 2.0%) using a ventilator. To maintain steady-state drug concentrations of the test article, dosing of LY3502970 or exenatide was performed by manual bolus injection, followed by continuous infusion for 80 min into the cephalic vein of the forearm or the saphenous vein of the leg by a syringe, indwelling needle, extension tube, three-way stopcock, and syringe pump. Low and high doses were 1,800 and 5,400 ng/kg, respectively, for LY3502970 and 4.2 and 13.4 ng/kg for exenatide. Dosing volumes were 2 mL/kg for the bolus administration, and the infusion rates for low- and high-dose LY3502970 were 1,280 and 3,840 ng⋅kg−1⋅h−1 and were 6.5 and 21.8 ng⋅kg−1⋅h−1 for low- and high-dose exenatide. Infusion volume was 2.7 mL/kg at a speed of 2 mL⋅kg−1⋅h−1. Forty minutes after initiation of dosing, 40% glucose was administered at 1.25 mL⋅kg−1⋅min−1 via the cephalic or saphenous vein. Blood was collected from the femoral vein 5 min before and after dosing and then at 5, 10, 15, 20, 30, and 40 min following administration of 40% glucose. The studies were conducted at intervals of 7 or 24 d (days 8, 15, 22, 29, 36, and 60) using a 7 × 6 cross-over design.[2] Food Consumption Studies. [2] Eight male cynomolgus monkeys (7.5 to 9.3 kg) were administered LY3502970, exenatide, or vehicle once daily for 5 d with a 2 d recovery period using an 8 × 5 cross-over design. Food consumption during the 90 min period following presentation of food was measured in animals previously administered LY3502970, exenatide, or vehicle as follows: 1) LY3502970 at 0.05 or 0.1 mg/kg by oral administration 180 min before feeding, 2) exenatide at 0.3 or 0.6 µg/kg by s.c. injection 30 min before feeding, or 3) the matched vehicle administered at the appropriate time. |
| 参考文献 | |
| 其他信息 |
Since peptide-based GLP-1R agonists exhibit an anorexigenic effect as part of their overall ability to improve metabolic control, LY3502970 was orally administered to monkeys to examine the ability of the compound to reduce feeding. Following LY3502970 or exenatide treatment, food consumption was measured for 90 min. For these studies, LY3502970 was administered orally 180 min before feeding, and exenatide was s.c. injected 30 min prior to food availability, in line with the time of maximum concentration observed (Tmax) in monkey pharmacokinetic studies. Dosing was conducted once daily for 5 d with a 2 d recovery period. LY3502970 at 0.05 and 0.1 mg/kg decreased food consumption from the first to the fifth days of dosing in a dose-dependent manner (Fig. 5F), similar to that observed for 0.3 and 0.6 µg/kg of exenatide (Fig. 5G). The mean LY3502970 and exenatide concentrations which decreased food consumption were 8.3 ± 0.8 nmol/L and 83.1 ± 4.5 pmol/L, respectively (mean ± SEM, n = 8). These results indicate that orally dosed LY3502970 can achieve a reduction of food intake similar to the injectable GLP-1R agonist, exenatide. Taken together, LY3502970 displays a preclinical pharmacodynamic profile similar to marketed peptide-based GLP-1R agonists and possesses pharmacokinetic properties compatible with oral dosing in humans. Consequently, LY3502970 is currently being evaluated in early stage clinical trials for its potential as an antidiabetic agent (identifier, NCT04426474).[2]
For the treatment-regimen estimand,4 each dose of orforglipron led to statistically significant A1C reductions. In the key secondary endpoint for body weight, 12 mg and 36 mg doses led to statistically significant reductions. A1C reduction: 1.2% (3 mg), 1.5% (12 mg), 1.5% (36 mg), 0.4% (placebo) Percent weight reduction: 4.5% (3 mg), 5.8% (12 mg), 7.6% (36 mg), 1.7% (placebo) Weight reduction: 4.2 kg (9.3 lbs; 3 mg), 5.2 kg (11.5 lbs; 12 mg), 7.2 kg (15.8 lbs; 36 mg), 1.5 kg (3.4 lbs; placebo) The overall safety profile of orforglipron in ACHIEVE-1 was consistent with the established GLP-1 class. The most commonly reported adverse events were gastrointestinal-related and generally mild to moderate in severity. The most common adverse events for participants treated with orforglipron (3 mg, 12 mg and 36 mg, respectively) were diarrhea (19%, 21% and 26%) vs. 9% with placebo, nausea (13%, 18% and 16%) vs. 2% with placebo, dyspepsia (10%, 20% and 15%) vs. 7% with placebo, constipation (8%, 17% and 14%) vs. 4% with placebo, and vomiting (5%, 7% and 14%) vs. 1% with placebo. Overall treatment discontinuation rates due to adverse events were 6% (3 mg), 4% (12 mg) and 8% (36 mg) for orforglipron vs. 1% with placebo. No hepatic safety signal was observed. The ACHIEVE-1 results will be presented at ADA's 85th Scientific Sessions and published in a peer-reviewed journal. More results from the ACHIEVE Phase 3 clinical trial program will be shared later this year, along with findings from the ATTAIN Phase 3 clinical trial program evaluating orforglipron for weight management. Lilly expects to submit orforglipron for weight management to global regulatory agencies by the end of this year, with the submission for the treatment of type 2 diabetes anticipated in 2026. About orforglipron Orforglipron (or-for-GLIP-ron) is an investigational, once-daily small molecule (non-peptide) oral glucagon-like peptide-1 receptor agonist that can be taken any time of the day without restrictions on food and water intake.5 Orforglipron was discovered by Chugai Pharmaceutical Co., Ltd. and licensed by Lilly in 2018. Chugai and Lilly published the preclinical pharmacology data of this molecule together.6 Lilly is running Phase 3 studies on orforglipron for the treatment of type 2 diabetes and for weight management in adults with obesity or overweight with at least one weight-related medical problem. It is also being studied as a potential treatment for obstructive sleep apnea and hypertension in adults with obesity. About ACHIEVE-1 and ACHIEVE clinical trial program ACHIEVE-1 (NCT05971940) is a Phase 3, 40-week, randomized, double-blind, placebo-controlled trial comparing the efficacy and safety of orforglipron 3 mg, 12 mg and 36 mg as monotherapy to placebo in adults with type 2 diabetes and inadequate glycemic control with diet and exercise alone. The trial randomized 559 participants across the U.S., China, India, Japan and Mexico in 1:1:1:1 ratio to receive either 3 mg, 12 mg or 36 mg orforglipron or placebo. The objective of the study was to demonstrate that orforglipron (3 mg, 12 mg, 36 mg) is superior in A1C reduction from baseline after 40 weeks, compared to placebo, in people with type 2 diabetes who have not taken any anti-diabetic medications for at least 90 days prior to visit 1, and are naïve to insulin therapy. Study participants had a HbA1c between ≥7.0% and ≤9.5% and a BMI of ≥23 kg/m2. All participants in the orforglipron treatment arms started the study at a dose of orforglipron 1 mg once-daily and then increased the dose in a step-wise approach at four-week intervals to their final randomized maintenance dose of 3 mg (via a 1 mg step), 12 mg (via steps at 1 mg, 3 mg and 6 mg) or 36 mg (via steps at 1 mg, 3 mg, 6 mg, 12 mg and 24 mg). Flexible dosing was not permitted. The ACHIEVE Phase 3 global clinical development program for orforglipron has enrolled more than 6,000 people with type 2 diabetes across five global registrational trials. The program began in 2023 with results anticipated later this year and into 2026.https://investor.lilly.com/news-releases/news-release-details/lillys-oral-glp-1-orforglipron-demonstrated-statistically |
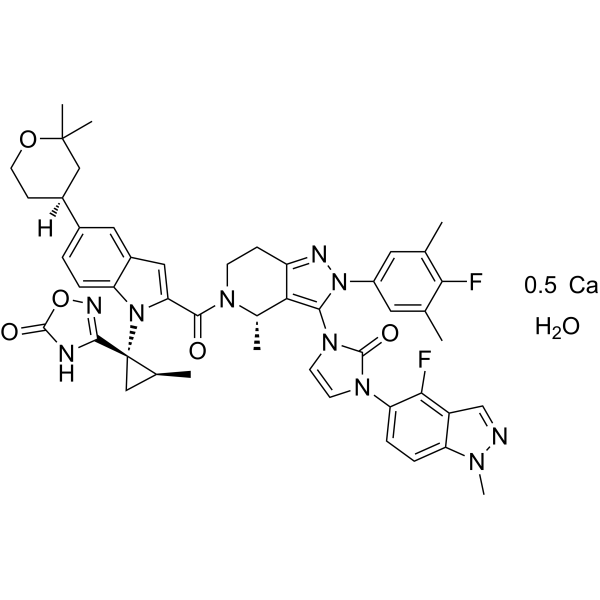
| 分子式 |
C48H50CAF2N10O6
|
|---|---|
| 分子量 |
941.05
|
| 精确质量 |
940.35087
|
| CAS号 |
3008544-96-2
|
| 相关CAS号 |
2212020-52-3 (free);2415797-61-2 (calcium); 3008544-96-2; 2212021-26-4 (calcium hydrate);
|
| PubChem CID |
171390963
|
| 外观&性状 |
White to off-white solid powder
|
| tPSA |
145Ų
|
| 氢键供体(HBD)数目 |
2
|
| 氢键受体(HBA)数目 |
11
|
| 可旋转键数目(RBC) |
7
|
| 重原子数目 |
67
|
| 分子复杂度/Complexity |
1950
|
| 定义原子立体中心数目 |
4
|
| SMILES |
[Ca].FC1C(C)=CC(=CC=1C)N1C(=C2C(CCN([C@H]2C)C(C2=CC3C=C([C@H]4CCOC(C)(C)C4)C=CC=3N2[C@@]2(C3=NOC(N3)=O)C[C@@H]2C)=O)=N1)N1C=CN(C2C=CC3=C(C=NN3C)C=2F)C1=O.O
|
| InChi Key |
XMVXKSTUSYLMQM-BJPQXFNBSA-N
|
| InChi Code |
InChI=1S/C48H48F2N10O5.Ca.H2O/c1-25-18-32(19-26(2)40(25)49)60-42(58-16-15-57(46(58)63)37-11-10-36-33(41(37)50)24-51-55(36)7)39-28(4)56(14-12-34(39)53-60)43(61)38-21-31-20-29(30-13-17-64-47(5,6)23-30)8-9-35(31)59(38)48(22-27(48)3)44-52-45(62)65-54-44;;/h8-11,15-16,18-21,24,27-28,30H,12-14,17,22-23H2,1-7H3,(H,52,54,62);;1H2/t27-,28-,30-,48-;;/m0../s1
|
| 别名 |
LY3502970 hemicalcium hydrate; GLP-1 receptor agonist 1 hemicalcium hydrate
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month 注意: 请将本产品存放在密封且受保护的环境中,避免吸湿/受潮。 |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
DMSO : 25 mg/mL (27.14 mM; with sonication)
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.0626 mL | 5.3132 mL | 10.6264 mL | |
| 5 mM | 0.2125 mL | 1.0626 mL | 2.1253 mL | |
| 10 mM | 0.1063 mL | 0.5313 mL | 1.0626 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。