| 规格 | 价格 | |
|---|---|---|
| 500mg | ||
| 1g | ||
| Other Sizes |
| 体外研究 (In Vitro) |
药物化合物包括碳、氢和其他元素的稳定重同位素,在药物开发过程中主要作为定量示踪剂。由于氘化可能会影响药物的药代动力学和代谢特性,因此值得关注[1]。
|
|---|---|
| 毒性/毒理 (Toxicokinetics/TK) |
Effects During Pregnancy and Lactation
◉ Summary of Use during Lactation Because of the low reported levels of progesterone in breastmilk, even with the high-dose products, amounts ingested by the infant are small and would not be expected to cause any adverse effects in breastfed infants. The progesterone vaginal ring available in some countries produces maternal blood levels that are lower than those of ovulating women. Most studies indicate that progesterone is not detrimental to milk production or duration of nursing. No special precautions appear to be required. In Russia, a progesterone gel (Progestogel - Besins Healthcare; not available in the US) has been used topically as a one-time application to the breasts to treat postpartum breast engorgement when more conservative measures have failed. A subsequent study failed to detect any decrease in breast hardness 20 minutes after application of progesterone gel in mothers with engorgement. The safety and efficacy of this use have not been well studied and the manufacturer of Progestogel recommends avoiding its use during lactation. ◉ Effects in Breastfed Infants Eighty-four women had 6 subdermal implants containing 100 mg each of progesterone inserted between days 30 to 35 postpartum as a contraceptive. Compared to women who received either a placebo or a Copper T intrauterine device, there were no differences in the growth rates of their infants over the first 6 months postpartum. One hundred ninety-two mothers who received 6 subdermal implants containing 100 mg each of progesterone inserted on postpartum day 60 as a contraceptive. The weight gain of 60 infants who were exclusively breastfed for 6 months was compared to that of infants whose mothers received either placebo (n = 68 at day 30) or a Copper T (n = 64 at day 30 and n = 49 at day 60) intrauterine device. No differences were found in the average weight gains among the 3 groups of infants at 6 months of age. Vaginal rings that released progesterone were inserted at about 60 days postpartum in 128 women. The 2 types of rings released progesterone either 7.5 mg daily decreasing to 4.5 mg at 90 days or 15 mg daily decreasing to 7 mg daily at 90 days. Over the first 12 months postpartum, no differences in weight gain were found between the exclusively breastfed infants of mothers who received the progesterone rings and control mothers who received a Copper T intrauterine device for contraception. One hundred twenty breastfeeding women used a vaginal ring that released about 10 mg daily of progesterone for 90 days, starting during weeks 5 to 7 postpartum. No differences were found in the growth of breastfed infants or in developmental milestones compared to the normal population values. One hundred eighty-seven breastfeeding women used a vaginal ring that released about 10 mg daily of progesterone, starting at about day 57 postpartum. No differences were found in weight gain during the first 6 months of use compared to infants whose mothers received either a Copper T intrauterine device, an oral progestin-only contraceptive or levonorgestrel implant. A study comparing 100 women who received vaginal ring that released about 10 mg daily of progesterone to those who received a Copper T intrauterine device between days 29 and 64 postpartum found no differences in weight gain of their breastfed infants over the first year postpartum. Two hundred eighty-five women who received a vaginal ring that released about 10 mg daily of progesterone were compared to 262 women who received a Copper T intrauterine device beginning between weeks 5 and 9 postpartum. No differences in the weight gain of breastfed infants were seen between the 2 groups during the 14-month observation period. A study comparing progesterone ring (n = 459) to the copper-T IUD (n = 330) in postpartum women found no adverse effects on infant breastfeeding or growth. ◉ Effects on Lactation and Breastmilk Eighty-four women had 6 subdermal implants containing 100 mg each of progesterone inserted between days 30 to 35 postpartum as a contraceptive. Compared to women who received either a placebo or a Copper T intrauterine device, no difference was found in the breastfeeding rates during the first 9 months postpartum. At 1 year postpartum, more women in the Copper T group were breastfeeding than in the progesterone or placebo groups. Vaginal rings that released progesterone were inserted at about 60 days postpartum in 246 women. The 3 types of rings released progesterone either 5, 10 or 15 mg daily. Control women received a Copper T intrauterine device. At 6 and 12 months postpartum there was no significant difference in the percentage of infants who were breastfed between the progesterone and Copper T groups. One hundred twenty breastfeeding women used a vaginal ring that released about 10 mg daily of progesterone, starting during weeks 5 to 7 postpartum. The rate of weaning was greater in the progesterone ring group than in groups of women who received levonorgestrel or norethindrone implants for postpartum contraception. In a multicenter study, 802 women who received a vaginal ring that released about 10 mg daily of progesterone were compared to 734 women who received a Copper T intrauterine device beginning at day 29 to 63 postpartum. No differences were found in the rate of breastfeeding between the 2 groups over the first year postpartum. Two hundred eighty-five women who received a vaginal ring that released about 10 mg daily of progesterone were compared to 262 women who received a Copper T intrauterine device beginning between weeks 5 and 9 postpartum. No differences in the breastfeeding rates were seen between the 2 groups during the 14-month observation period. An observational study followed 192 women who used a vaginal ring that released 10 mg of progesterone daily beginning between days 54 and 64 postpartum. All subjects used the vaginal ring for at least 4 months; 90% were still using it at 6 months and 73% were using it at 9 months postpartum. The duration of breastfeeding and infant growth were similar to reference groups. A double-blind placebo-controlled trial randomized 46 postpartum women who were abstinent former smokers to oral micronized progesterone 200 mg twice a day or placebo for 4 weeks to assess smoking abstinence rates. Entry into the study occurred only after breastfeeding was well established. No statistical difference was found in the number of days of breastfeeding between the groups. A study comparing progesterone ring (n = 459) to the copper-T IUD (n = 330) in postpartum women found that lactation amenorrhea lasted longer (405 days) with the progesterone ring than with the IUD (120 days). A transgender woman took and spironolactone 50 mg twice daily to suppress testosterone, domperidone 10 mg three times daily, increasing to 20 mg four times daily, oral micronized progesterone 200 mg daily and oral estradiol to 8 mg daily and pumped her breasts 6 times daily to induce lactation. After 3 months of treatment, estradiol regimen was changed to a 0.025 mg daily patch and the progesterone dose was lowered to 100 mg daily. Two weeks later, she began exclusively breastfeeding the newborn of her partner. Breastfeeding was exclusive for 6 weeks, during which the infant's growth, development and bowel habits were normal. The patient continued to partially breastfeed the infant for at least 6 months. A transgender woman was taking spironolactone 100 mg twice daily, progesterone 200 mg daily and estradiol 5 mg daily. She was started on domperidone 10 mg three times daily to increase milk supply. She was able to pump 3 to 5 ounces of milk daily one month after starting. The dose of domperidone was increased to 30 mg three times daily after 8 weeks because of a decreased milk supply. Her milk supply returned to 3 to 5 ounces of milk daily. By 6 months, her milk supply had decreased to about 5 mL daily, even though her serum prolactin was still elevated. A transgender woman had been taking estradiol 2 mg twice daily for 14 years. She began taking domperidone 10 mg four times daily and progesterone 100 mg daily 107 days prior to her partner’s due date. At the same time, the estradiol dosage was increased to 4 mg twice daily. At 94 days prior to the due date, the domperidone dosage was increased to 20 mg four times daily, the progesterone dose was increased to 200 mg daily and estrogen was changed to transdermal estradiol 25 mcg daily. Progesterone was discontinued 34 days prior to the due date. She pumped and stored milk beginning at 34 days prior to the due date and by 27 days postpartum, she was breastfeeding the infant twice daily, expressing 150 mL of milk daily and was able to decrease the domperidone dosage to 20 mg three times daily. Lower dosages reduced milk supply. A transgender woman was taking sublingual estradiol 4 mg twice daily, spironolactone 100 mg twice daily and progesterone 200 mg at bedtime for gender-affirming therapy. In order to prepare for the birth of the infant being carried by her partner, sublingual estradiol was increased to 6 mg twice daily and progesterone was increased to 400 mg at bedtime. Domperidone 10 mg twice daily was also started to increase serum prolactin levels and later increased to 20 mg 4 times daily. Before the delivery date, progesterone was stopped, spironolactone was decreased to 100 mg daily and estradiol was changed to 25 mcg per day transdermally. At day 59 postpartum, estradiol was changed to 2 mg per day sublingually and spironolactone was increased to 100 mg twice daily. The patient was able to produce up to 240 mL of milk daily containing typical macronutrient and oligosaccharide levels. A transgender woman who wished to breastfeed was given estradiol transdermal patch 150 mcg daily and progesterone 100 mg daily by mouth. Later estradiol spray 100 mcg and domperidone 10 mg 4 times daily were added. Domperidone dosage was then doubled to 20 mg 4 times daily and progesterone was doubled to 100 mg twice daily. After further adjustment of estradiol and progesterone dosages, 7 mL of milk was produced with pumping, but 2 weeks after the infant’s birth, lactation induction was discontinued at the patient’s request. A 50-year-old transgender woman wished to breastfeed her grandchild was taking baseline treatment with estradiol 0.3 mg transdermal patch every 72 hours and micronized progesterone 200 mg oral once daily. To initiate lactation, her estradiol dose was increased to a 0.4 mg transdermal patch every 72 hours and nipple stimulation was initiated. Later the patient’s progesterone was increased to 300 mg daily and metoclopramide oral 10 mg three times daily was initiated. She lactated for a total of two weeks and nursed the four-month-old infant on multiple occasions. Her peak milk production was 30 mL from her larger right breast, and 8 mL from her smaller left breast. |
| 参考文献 |
| 分子式 |
C21H30O2
|
|---|---|
| 分子量 |
314.46
|
| 精确质量 |
316.231
|
| CAS号 |
82938-07-6
|
| 相关CAS号 |
Progesterone;57-83-0
|
| PubChem CID |
163196495
|
| 外观&性状 |
White to off-white solid powder
|
| LogP |
3.9
|
| tPSA |
34.1
|
| 氢键供体(HBD)数目 |
0
|
| 氢键受体(HBA)数目 |
2
|
| 可旋转键数目(RBC) |
1
|
| 重原子数目 |
23
|
| 分子复杂度/Complexity |
589
|
| 定义原子立体中心数目 |
6
|
| SMILES |
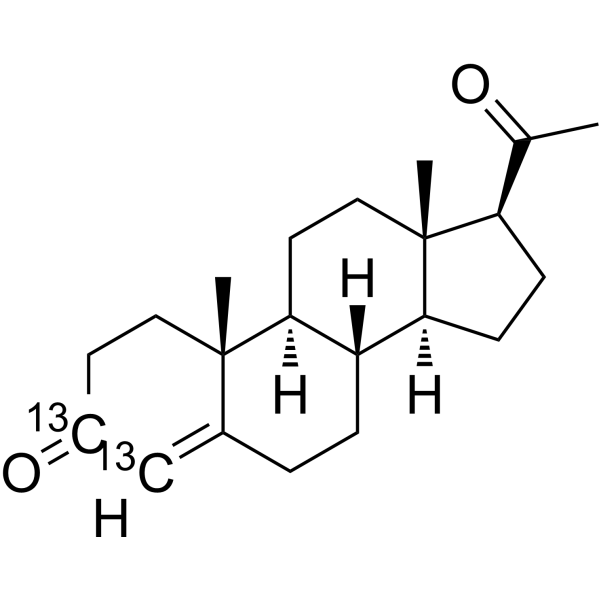
CC(=O)[C@H]1CC[C@@H]2[C@@]1(CC[C@H]3[C@H]2CCC4=[13CH][13C](=O)CC[C@]34C)C
|
| InChi Key |
RJKFOVLPORLFTN-PIWOXAIRSA-N
|
| InChi Code |
InChI=1S/C21H30O2/c1-13(22)17-6-7-18-16-5-4-14-12-15(23)8-10-20(14,2)19(16)9-11-21(17,18)3/h12,16-19H,4-11H2,1-3H3/t16-,17+,18-,19-,20-,21+/m0/s1/i12+1,15+1
|
| 化学名 |
(8S,9S,10R,13S,14S,17S)-17-acetyl-10,13-dimethyl-1,2,6,7,8,9,11,12,14,15,16,17-dodecahydrocyclopenta[a]phenanthren-3-one
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 3.1801 mL | 15.9003 mL | 31.8005 mL | |
| 5 mM | 0.6360 mL | 3.1801 mL | 6.3601 mL | |
| 10 mM | 0.3180 mL | 1.5900 mL | 3.1801 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。