| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 2mg |
|
||
| 5mg |
|
||
| 10mg |
|
||
| 25mg |
|
||
| 50mg |
|
||
| Other Sizes |
|
| 靶点 |
GLP-1 receptor
|
|---|---|
| 体外研究 (In Vitro) |
索马鲁肽在第 26 位赖氨酸处衍生化,与人 GLP-1 的不同之处在于两个氨基酸取代(Aib8、Arg34)。索马鲁肽对 GLP-1R 的亲和力为 0.38±0.06 nM[1]。与人 GLP-1 94% 序列相似的 GLP-1 类似物是索马鲁肽 [3]。
|
| 体内研究 (In Vivo) |
小型猪皮下给药后索马鲁肽的 MRT 为 63.6 小时,静脉给药后小型猪的血浆半衰期为 46 小时[1]。索马鲁肽可改善 1-甲基-4-苯基-1,2,3,6-四氢吡啶 (MPTP) 引起的运动障碍。索马鲁肽还通过挽救酪氨酸羟化酶(TH)水平的降低、减少脂质过氧化、减轻炎症、抑制细胞凋亡途径和增加自噬相关蛋白的表达来保护黑质和纹状体中的多巴胺能神经元。此外,索马鲁肽(一种长效 GLP-1 类似物)在大多数参数上均优于利拉鲁肽[2]。索马鲁肽通过促进胰岛素的释放来降低体重和血糖[3]。
|
| 酶活实验 |
HEK293‐SNAP‐GLP‐1R细胞在悬浮液中用SNAP‐Lumi4‐Tb(40 nM,Cisbio,Codelet,France)在室温下在完全培养基中培养1小时。在含有0.1%牛血清白蛋白和代谢抑制剂(20 mmol/L 2-脱氧葡萄糖和10 mmol/L NaN3)以防止GLP‐1R内化,如前所述,使用exendin(9‐39)和异硫氰酸荧光素(FITC)安装在K12位置,通过时间分辨förster共振能量转移(FRET)进行结合实验。[4]
|
| 细胞实验 |
Semagulide激活胰腺β细胞中的GLP-1受体,导致葡萄糖依赖性胰岛素释放。它还能减少胰高血糖素的分泌,减缓胃排空,促进饱腹感。
|
| 动物实验 |
Mice: Male C57BL/6 mice 10 weeks old (20-25 g) are used throughout the study. Six groups of mice are randomly assigned (n = 12 per group). The treatments were as follows: (i) saline alone was given to the control group; (ii) NN-2211 group received saline and NN-2211 (25 nmol/kg ip. once daily for 7 days); (iii) Semaglutide group received saline and Semaglutide (25 nmol/kg ip. once daily for 7 days); (iv) MPTP group received MPTP alone (once daily 20 mg/kg ip. for 7 days); (v) MPTP (once daily 20 mg/kg ip. for 7 days) was immediately followed by NN-2211 treated group (25 nmol/kg ip. once daily for 7 days). (vi) MPTP (20 mg/kg i.p. once daily for 7 days), which was immediately followed by the group treated with semaglutide (25 nmol/kg i.p. once daily for 7 days). Measure behavioral changes, neuronal damage, inflammatory markers, and other biomarkers at the conclusion of drug treatments. [2]
|
| 药代性质 (ADME/PK) |
Absorption: The Cmax of semaglutide was 10.9 nmol/L, with AUC of 3123.4 nmol h/L and a Tmax of 56 h in one clinical trial, achieved within 1-3 days. The absolute bioavailability is 89%. Steady-state concentration of the oral tablet is achieved in 4-5 weeks. Average steady state concentrations of semaglutide are the mean steady state concentrations after dosing at 0.5mg to 1mg range from 16 nmol/L to 30 nmol/L.
Route of Elimination: This drug is mainly cleared by the kidneys, and is found excreted in both the urine and feces. The main elimination route is the urine by corresponding to 53% of an ingested radiolabeled dose, with 18.6% found in the feces. A smaller amount of 3.2% was found to be exhaled. Hepatic impairment does not appear to affect the clearance of this drug and dose adjustments are not required in patients with decreased liver function. Volume of Distribution: The volume of distribution of semaglutide is 8L to 9.4L. It crosses the placenta in rats. Clearance: The clearance rate of semaglutide is 0.039 L/h according to one clinical study. On the FDA label, semaglutide clearance is reported to be about 0.05 L/h in patients with type 2 diabetes mellitus. Metabolism / Metabolites: Semaglutide is cleaved at the peptide backbone, followed by β‐oxidation of the fatty acid chain. Naturally occurring GLP‐1 is quickly metabolized by dipeptidyl peptidase‐4 (DPP‐4) and other enzymes, which is ubiquitous in human tissues. Chemical structure modifications render semaglutide less susceptible to enzymatic degradation by gastrointestinal DPP‐4 enzymes. It is slowly and extensively metabolized, with about 83% of the administered dose measured in the plasma as unchanged drug. Neural endopeptidase (NEP) is another enzyme that metabolizes this drug. DPP-4 inactivates semaglutide, truncating the N-terminal segment while NEP hydrolyzes peptide bondsSix different metabolites of semaglutide have been identified in human plasma. The major metabolite, named P3, accounts for about 7.7% of an ingested dose. Biological Half-Life: One of the major properties of semaglutide is its long half-life of 168 h. The long half-life is attributed to its albumin binding. This lowers the renal clearance and protects semaglutide from metabolic breakdown. |
| 毒性/毒理 (Toxicokinetics/TK) |
Hepatotoxicity
In large clinical trials, serum enzyme elevations were no more common with semaglutide therapy than with placebo or comparator agents, and no instances of clinically apparent liver injury were reported. Indeed, treatment with semaglutide and other GLP-1 analogues is often associated with improvements in serum aminotransferase levels (and hepatic steatosis) making them possible treatments for nonalcoholic fatty liver. Since licensure, there have been no published case reports of hepatotoxicity due to semaglutide and the product label does not list liver injury as an adverse event. Thus, liver injury due to semaglutide must be rare, if it occurs at all. Likelihood score: E (unlikely cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation No information is available on the clinical use of semaglutide during breastfeeding. Because semaglutide is a peptide molecule with a molecular weight of 4113 daltons and is over 99% protein bound, the amount in milk is likely to be very low. Absorption by the infant is unlikely because the drug is probably destroyed in the infant's gastrointestinal tract. Until more data become available, semaglutide should be used with caution during breastfeeding, especially while nursing a newborn or preterm infant. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. View More
◈ What is semaglutide?
Protein Binding Semaglutide binds with high affinity to plasma albumin, promoting high levels of drug stability. It is more than 99% bound to albumin. |
| 参考文献 |
[3]. Semaglutide: First Global Approval. Drugs. 2018 Feb;78(2):275-284. |
| 其他信息 |
Novo Nordisk has developed a subcutaneous formulation of semaglutide (Ozempic®), a modified human glucagon-like peptide-1 (GLP-1) analogue, for the treatment of type 2 diabetes mellitus. It has been developed using Novo Nordisk's proprietary protein-acylation technology, and is administered using an injection device. Semaglutide lowers blood glucose by stimulating the release of insulin and also lowers body weight. Once-weekly subcutaneous semaglutide has recently been approved in the US, Puerto Rico and Canada, and has received a positive opinion in the EU for the treatment of patients with type 2 diabetes. It will be launched as the Ozempic® Pen, a pre-filled device. Semaglutide is also under regulatory review in Japan and Switzerland for the treatment of type 2 diabetes. Clinical development for obesity, non-alcoholic steatohepatitis and non-alcoholic fatty liver disease is underway worldwide. This article summarizes the milestones in the development of semaglutide leading to this first approval for type 2 diabetes.[3]
In patients with type 2 diabetes who were at high cardiovascular risk, the rate of cardiovascular death, nonfatal myocardial infarction, or nonfatal stroke was significantly lower among patients receiving semaglutide than among those receiving placebo, an outcome that confirmed the noninferiority of semaglutide. [2] Semaglutide is a polypeptide that contains a linear sequence of 31 amino acids joined together by peptide linkages. It is an agonist of glucagon-like peptide-1 receptors (GLP-1 AR) and used for the treatment of type 2 diabetes. It has a role as a hypoglycemic agent, a glucagon-like peptide-1 receptor agonist, an anti-obesity agent, a neuroprotective agent and an appetite depressant. It is a polypeptide and a lipopeptide. Semaglutide is a glucagon-like peptide 1 (GLP-1) analog used to manage type 2 diabetes along with lifestyle changes, such as dietary restrictions and increased physical activity. Other members of this drug class include [Exenatide] and [Liraglutide]. Semaglutide was developed by Novo Nordisk and approved by the FDA for subcutaneous injection in December 2017. The tablet formulation was approved for oral administration in September 2019. Semaglutide works by binding to and activating the GLP-1 receptor, thereby stimulating insulin secretion and reducing blood glucose. The subcutaneous injection is administered once weekly and the tablet is administered once a day. Semaglutide offers a competitive advantage over other drugs used to manage diabetes, which may require several daily doses. Clinical trials have determined that this drug reduces glycosylated hemoglobin (HbA1c) levels and reduces body weight, proving to be effective for patients with type 2 diabetes. In June 2021, semaglutide was approved by the FDA for chronic weight management in adults with general obesity or overweight who have at least one weight-related condition, marking semaglutide as the first approved drug for such use since 2014. The use of semaglutide in weight management is also approved by Health Canada and the EMA. On May 31, 2023, the FDA issued a warning regarding the use of compounded semaglutide after receiving adverse event reports. The use of salt forms of semaglutide, including semaglutide sodium and semaglutide acetate, has not been proven to be safe or effective. View More
Semaglutide is a GLP-1 Receptor Agonist. The mechanism of action of semaglutide is as a Glucagon-like Peptide-1 (GLP-1) Agonist.
Semaglutide is indicated to improve glycemic control in adults diagnosed with type 2 diabetes mellitus, and is used as an adjunct to diet and exercise. However, semaglutide is not a suitable first-line drug for diabetes that has not been controlled by diet and exercise. In addition, it has not been studied in patients with pancreatitis. Semaglutide is not intended for use in patients with type 1 diabetes or to treat diabetic ketoacidosis. Semaglutide is indicated for chronic weight management in adults with obesity or overweight with at least one weight-related condition (such as high blood pressure, type 2 diabetes, or high cholesterol), for use in addition to a reduced-calorie diet and increased physical activity.. Semaglutide it is also indicated for chronic weight management in pediatric patients aged 12 years and older with an initial BMI at the 95th percentile or greater for age and sex. Semaglutide reduces HbA1c, systolic blood pressure, and body weight. After 12 weeks of treatment, semaglutide decreased fasting and postprandial glucose by increasing insulin production and decreasing glucagon secretion (which is normally associated with increases in blood sugar). Semaglutide also lowers fasting triglycerides and VLDL cholesterol, exerting beneficial effects on cardiovascular health. Semaglutide has been shown to cause medullary thyroid cell carcinoma in rodents. While its clinical relevance to humans is unknown, the FDA advises not to administer this drug in those with a personal or family history of medullary thyroid carcinoma. Semaglutide also poses a risk of pancreatitis and dehydration. Patients must be adequately hydrated while on semaglutide and are advised to seek medical attention immediately in cases of abdominal pain radiating to the back. Because this drug delays gastric emptying, it is important to monitor for the efficacy or adverse effects of other drugs that are administered orally. Mechanism of Action: Mechanism of glycemic control** GLP-1 is a physiological hormone that promotes glycemic control via several different mechanisms, including insulin secretion, slowing gastric emptying, and reducing postprandial glucagon secretion. The homeostasis of glucose is dependent on hormones such as insulin and amylin, which are secreted by the beta cells of the pancreas. Semaglutide is 94% similar to human GLP-1. Analogs of this hormone such as semaglutide stimulate the synthesis of insulin by stimulating pancreatic islet cells and reducing glucagon secretion. They directly bind with selectivity to the GLP-1 receptor, causing various beneficial downstream effects that reduce blood glucose in a glucose-dependent fashion. **Mechanism of cardiovascular benefit and weight loss** In hypercholesterolemia, semaglutide is believed to reduce the progression of atherosclerosis via decreased gut permeability and decreased inflammation. Weight loss is believed to occur via the reduction of appetite and food cravings after semaglutide administration. Hepatotoxicity: In large clinical trials, serum enzyme elevations were no more common with semaglutide therapy than with placebo or comparator agents, and no instances of clinically apparent liver injury were reported. Indeed, treatment with semaglutide and other GLP-1 analogues is often associated with improvements in serum aminotransferase levels (and hepatic steatosis) making them possible treatments for nonalcoholic fatty liver. Since licensure, there have been no published case reports of hepatotoxicity due to semaglutide and the product label does not list liver injury as an adverse event. Thus, liver injury due to semaglutide must be rare, if it occurs at all. |
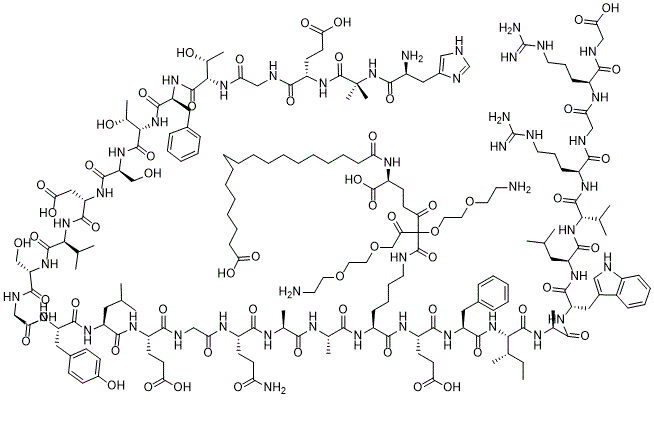
| 分子式 |
C189H292F3N45O61
|
|---|---|
| 分子量 |
4227.66
|
| 相关CAS号 |
910463-68-2 (Semaglutide free base); 1997361-85-9 (Semaglutide acetate); 2924330-56-1 (sodium)
|
| 序列 |
H-His-Aib-Glu-Gly-Thr-Phe-Thr-Ser-Asp-Val-Ser-Ser-Tyr-Leu-Glu-Gly-Gln-Ala-Ala-Lys-Glu-Phe-Ile-Ala-Trp-Leu-Val-Arg-Gly-Arg-Gly-OH
|
| 短序列 |
HXEGTFTSDV SSYLEGQAAK EFIAWLVRGR G
|
| 外观&性状 |
White to off-white solid powder
|
| 别名 |
NNC 0113-0217 TFA; NNC 0113-0217; NNC-0113-0217; NNC-0113 0217
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
|
|||
|---|---|---|---|---|
| 溶解度 (体内实验) |
如何溶解多肽,详情请参考右上角《产品说明书》第3页:“多肽溶解指南”。
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。 注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 0.2365 mL | 1.1827 mL | 2.3654 mL | |
| 5 mM | 0.0473 mL | 0.2365 mL | 0.4731 mL | |
| 10 mM | 0.0237 mL | 0.1183 mL | 0.2365 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
| NCT Number | Recruitment | interventions | Conditions | Sponsor/Collaborators | Start Date | Phases |
| NCT05649137 | Active Recruiting |
Drug: Semaglutide Drug: Placebo |
Obesity Diabetes Mellitus, Type 2 |
Novo Nordisk A/S | January 4, 2023 | Phase 3 |
| NCT05646706 | Active Recruiting |
Drug: Semaglutide Drug: Placebo |
Obesity | Novo Nordisk A/S | January 4, 2023 | Phase 3 |
| NCT05302596 | Active Recruiting |
Drug: Semaglutide Pen Injector |
Obesity Aging |
State University of New York at Buffalo |
September 1, 2022 | Phase 4 |
| NCT05564117 | Active Recruiting |
Drug: Semaglutide Drug: Placebo semaglutide |
Overweight Obesity |
Novo Nordisk A/S | October 11, 2022 | Phase 3 |
| NCT04560998 | Active Recruiting |
Drug: Semaglutide Drug: Placebo (semaglutide) |
Diabetes Mellitus, Type 2 Peripheral Arterial Disease |
Novo Nordisk A/S | October 1, 2020 | Phase 3 |
|
|
|