| 规格 | 价格 | |
|---|---|---|
| 500mg | ||
| 1g | ||
| Other Sizes |

| 靶点 |
(1→3)-β-D-glucan synthase
|
|---|---|
| 体外研究 (In Vitro) |
当预先形成的白色念珠菌3153A生物膜暴露于卡泊芬净时,通过XTT还原试验评估的生物膜内细胞的代谢活性急剧降低(图1)。通过这种方法,卡泊芬净对生物膜内固着白色念珠菌3153A细胞的48小时MIC50为0.0625μg/ml。尽管用卡泊芬素处理不能实现生物膜的完全无菌,但实验表明,卡泊芬净浓度低至0.125μg/ml时,固着细胞的代谢活性降低了>97%。卡泊芬津对所有测试的白色念珠菌临床分离株(n=18)形成的生物膜也有活性,固着电池的MIC50在0.0625和0.125μ/ml之间,而氟康唑对所有分离株的固着细胞MIC50≥64μg/ml。与XTT测定一致,在卡泊芬净处理的生物膜内的细胞中仅检测到残余代谢活性,其显示出死细胞的弥漫性绿色荧光模式特征(图3B)。为了证实SEM结果,CLSM证明卡泊芬净处理产生的生物膜菌丝较少,并且还显示出整体生物膜结构的轻微扭曲。如图4所示,与未处理(对照)孔中的细胞相比,用卡泊芬净包衣导致粘附细胞的代谢活性显著降低(高达60%)。总之,这些发现表明卡泊芬净在体外对白色念珠菌生物膜表现出强大的活性,值得进一步研究用于治疗生物膜相关感染。[3]
|
| 体内研究 (In Vivo) |
卡泊芬净(1-8 mg/kg;腹腔注射;每日一次,持续 7 天)进入小鼠的中枢神经系统,并达到减少大脑中念珠菌负担的浓度 [1]。卡泊芬净(0.41-41 μM;腹腔注射;5 周;雄性 C57BL/6 小鼠)是一种安全的抗真菌药物,小鼠玻璃体浓度范围为 0.41 至 4.1 μM [2]。
|
| 酶活实验 |
棘白菌素MK-0991,原名L-743872,是一种水溶性脂肽,已在临床前研究中证明对念珠菌、烟曲霉和卡氏肺孢子虫具有有效活性。对MK-0991进行了广泛的体外生物学评估,以更好地确定这种新型化合物的潜在活性。使用MK-0991对大约200个念珠菌、新生隐球菌和曲霉菌临床分离株进行药敏试验,以确定MIC和最小杀真菌浓度MF(s)。对40个白色念珠菌临床分离株,90%的分离株被抑制的MFC为0.5微克/毫升。对念珠菌和新生隐球菌分离株的抗真菌药物耐药性菌株进行的敏感性测试表明,这些分离株的MK-0991 MFC与易感分离株的MFC相当。MK-0991对白色念珠菌和热带假丝酵母分离株的生长动力学研究表明,该化合物在0.06至1微克/毫升(MIC的0.25至4倍)的浓度下,在3至7小时内表现出杀真菌活性(即活力降低99%)。MK-0991与两性霉素B的药物组合研究发现,该组合在体外对白色念珠菌、新生隐球菌或烟曲霉没有拮抗作用。对0-50%的人或小鼠混合血清的研究证实,真菌对MK-0991的易感性不受人或小鼠血清存在的显著影响。耐药性诱导研究的结果表明,反复暴露(40代)MK-0991不会改变白色念珠菌的易感性。用MK-0991对洗涤和未洗涤的人或小鼠红细胞进行的红细胞溶血研究表明,该化合物的溶血潜力最小。临床前研究的这些有利结果支持MK-0991在人类身上的进一步研究。[4]
|
| 细胞实验 |
用卡泊芬净涂布微量滴定板的孔对白色念珠菌生物膜形成的影响。使用改良的测定法,其中微量滴定板的孔直接用卡泊芬净预涂,以研究该药物防止生物膜形成的能力。简言之,将无菌PBS中不同浓度的200μl体积的卡泊芬净加入微量滴定板的选定孔中,并在4°C下孵育过夜。孵育后,吸取过量的卡泊芬净,并在无菌PBS中洗涤平板一次。白色念珠菌3153A细胞在PBS中清洗,并以每毫升106个细胞的浓度重悬在RPMI 1640中。然后在96孔微量滴定板上接种悬浮液(每孔100μl),并在37°C下孵育24小时,以形成生物膜。在无菌PBS中抽吸和洗涤孔的内容物三次,并通过XTT还原测定和光学显微镜评估生物膜形成的程度。对于XTT测定,卡泊芬净的抑制作用表示为卡泊芬素处理的孔与对照(塑料)孔相比的光密度(OD)的百分比。采用Student t检验进行统计分析。P值<0.05被认为具有统计学意义。使用Prism 3.00版Window进行分析。[3]
|
| 动物实验 |
Animal/Disease Models: DBA/2N mice deficient in complement component 5 [1]
Doses: 1, 2, 4 and 8 mg/kg Route of Administration: intraperitoneal (ip) injection; one time/day for 7 days Experimental Results: diminished concentration of Candida load in the brain. Animal/Disease Models: Male C57BL/6 mice [2] Doses: 0.41, 1.2, 2.5, 4.1 and 41 μM Route of Administration: intraperitoneal (ip) injection; continued for 5 weeks Experimental Results: ERG waveform changed from 0.41 μM to 4.1 μM, no significant change . |
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
92% tissue distribution within 36-48 hours after intravenous infusion After single intravenous administration of [3H] caspofungin acetate, excretion of caspofungin and its metabolites in humans was 35% of dose in feces and 41% of dose in urine. 12 mL/min [After single IV administration] Elimination: Fecal: 35% as drug or metabolites. Renal: 41% as drug (approximately 1.4% unchanged) or metabolites. In dialysis: Not removed by hemodialysis. Following administration of a single 70 mg irradiated dose, approximately 92% of the administered radioactivity was distributed into tissues within 36 to 48 hours. Distribution into red blood cells in minimal. Caspofungin crosses the placenta in rats and rabbits and was detected in the plasma of fetuses of pregnant animals who were dosed with caspofungin. Caspofungin is distributed into milk in rats; not known whether caspofungin is distributed into milk in humans. For more Absorption, Distribution and Excretion (Complete) data for CASPOFUNGIN (13 total), please visit the HSDB record page. Metabolism / Metabolites Metabolized slowly by hydrolysis and N-acetylation Slowly metabolized by hydrolysis and N-acetylation; also undergoes spontaneous chemical degradation and further hydrolysis to constitutive amino acids and their degredates, including dihydroxyhomotyrosine and N-acetyl-dihydroxyhomotyrosine. Caspofungin is slowly metabolized in the liver via hydrolysis and N-acetylation; 35 and 41% of the parent drug and metabolites were excreted in feces and urine, respectively, following a single IV radiolabeled dose. The metabolism, excretion, and pharmacokinetics of caspofungin were investigated after administration of a single intravenous dose to mice, rats, rabbits, and monkeys. ... Excretion of radioactivity in all species studied was slow, and low levels of radioactivity were detected in daily urine and fecal samples throughout a prolonged collection period. Although urinary profiles indicated the presence of several metabolites (M0, M1, M2, M3, M4, M5, and M6), the majority of the total radioactivity was associated with the polar metabolites M1 [4(S)-hydroxy-4-(4-hydroxyphenyl)-L-threonine] and M2 (N-acetyl-4(S)-hydroxy-4-(4-hydroxyphenyl)-L-threonine). Caspofungin was thus primarily eliminated by metabolic transformation; however, the rate of metabolism was slow. ... Caspofungin is slowly metabolized by hydrolysis and N-acetylation. Caspofungin also undergoes spontaneous chemical degradation to an open-ring peptide compound, L-747969. At later time points (> or = 5 days postdose), there is a low level (< or = 7 picomoles/mg protein, or < or = 1.3% of administered dose) of covalent binding of radiolabel in plasma following single-dose administration of (3)H caspofungin acetate, which may be due to two reactive intermediates formed during the chemical degradation of caspofungin to L-747969. Additional metabolism involves hydrolysis into constitutive amino acids and their degradates, including dihydroxyhomotyrosine and N-acetyl-dihydroxyhomotyrosine. These two tyrosine derivatives are found only in urine, suggesting rapid clearance of these derivatives by the kidneys. /Caspofungin acetate/ ... Following a 1 hr IV infusion of 70 mg of (3)HCaspofungin acetate to healthy subjects, excretion of drug-related material was very slow, such that 41 and 35% of the dosed radioactivity was recovered in urine and feces, respectively, over 27 days. Plasma and urine samples collected around 24 hr postdose contained predominantly unchanged caspofungin acetate, together with trace amounts of a peptide hydrolysis product, M0, a linear peptide. However, at later sampling times, M0 proved to be the major circulating component, whereas corresponding urine specimens contained mainly the hydrolytic metabolites M1 and M2, together with M0 and unchanged MK-0991, whose cumulative urinary excretion over the first 16 days postdose represented 13, 71, 1, and 9%, respectively, of the urinary radioactivity. The major metabolite, M2, was highly polar and extremely unstable under acidic conditions when it was converted to a less polar product identified as N-acetyl-4(S)-hydroxy-4-(4-hydroxyphenyl)-L-threonine gamma-lactone. Derivatization of M2 in aqueous media led to its identification as the corresponding gamma-hydroxy acid, N-acetyl-4(S)-hydroxy-4-(4-hydroxyphenyl)-L-threonine. Metabolite M1, which was extremely polar, eluting from HPLC column just after the void volume, was identified by chemical derivatization as des-acetyl-M2. Thus, the major urinary and plasma metabolites of MK-0991 resulted from peptide hydrolysis and/or N-acetylation. /Caspofungin acetate/ Biological Half-Life 9-11 hours Initial: 9 TO 11 hours (beta phase). Additional: 40 to 50 hours (gamma phase). After administration of a single intravenous dose to mice, rats, rabbits, and monkeys, caspofungin had a ... long terminal elimination half-life (11.7 hr to 59.7 hr) in all preclinical species. |
| 毒性/毒理 (Toxicokinetics/TK) |
Effects During Pregnancy and Lactation
◉ Summary of Use during Lactation No information is available on the use of caspofungin during breastfeeding. Because caspofungin is 97% bound to plasma proteins and has poor oral bioavailability, it is unlikely to reach the milk and be absorbed by the infant. Caspofungin can safely be given intravenously to infants of aged 3 months or older. Any amount absorbed from milk is likely to be far less than an infant dose. If caspofungin is required by the mother, it is not a reason to discontinue breastfeeding. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk Relevant published information was not found as of the revision date. Protein Binding 97% Interactions ... In this study the efficacies of caspofungin and meropenem - separately and together - in mice with disseminated candidiasis were studied. Immunocompetent mice were infected intravenously with 2x10(6) CFU of Candida albicans. At 24 hr postinfection, intraperitoneal therapy was initiated and was continued for 7 days. Therapy groups included those given caspofungin (0.5, 1.25, 5 mg/kg/day), meropenem (20 mg/kg/day), and a combination of the two drugs. ... Kidney CFU counts showed that mice that had received both drugs had lower residual burdens. Caspofungin was effective at doses of 0.5, 1.25, 5 mg/kg compared to infected untreated controls. In vitro, MICs of caspofungin and meropenem were <0.075 ug/mL and >64 ug/mL, respectively. Synergism was observed with the combination. Histopathology showed that the degree of inflammation was 25% less and tubular necrosis was more restricted in combined therapy than monotherapy. The results indicate that concurrent caspofungin and meropenem therapy may be beneficial. Concomitant use /with tacrolimus/ may result in decreased tacrolimus blood concentrations; monitoring of tacrolimus concentrations is recommended, and dosage adjustments may be required. Potential pharmacokinetic interaction (reduction in caspofungin plasma concentrations.). Coadministration of caspofungin with inducers or mixed inducer/inhibitors of drug clearance such as efavirenz, nelfinavir, nevirapine, phenytoin, rifampin, dexamethasone, or carbamazepine may result in clinically important reductions in plasma caspofungin concentrations. ... The potential for interactions between caspofungin and nelfinavir or rifampin was evaluated in two parallel-panel studies. In study A, healthy subjects received a 14-day course of caspofungin alone (50 mg administered intravenously [IV] once daily) (n = 10) or with nelfinavir (1,250 mg administered orally twice daily) (n = 9) or rifampin (600 mg administered orally once daily) (n = 10). In study B, 14 subjects received a 28-day course of rifampin (600 mg administered orally once daily), with caspofungin (50 mg administered IV once daily) coadministered on the last 14 days, and 12 subjects received a 14-day course of caspofungin alone (50 mg administered IV once daily). The coadministration/administration alone geometric mean ratio for the caspofungin area under the time-concentration profile calculated for the 24-hr period following dosing [AUC(0-24)] was as follows (values in parentheses are 90% confidence intervals [CIs]): 1.08 (0.93-1.26) for nelfinavir, 1.12 (0.97-1.30) for rifampin (study A), and 1.01 (0.91-1.11) for rifampin (study B). The shape of the caspofungin plasma profile was altered by rifampin, resulting in a 14 to 31% reduction in the trough concentration at 24 hr after dosing (C(24h)), consistent with a net induction effect at steady state. Both the AUC and the C(24hr) were elevated in the initial days of rifampin coadministration in study A (61 and 170% elevations, respectively, on day 1) but not in study B, consistent with transient net inhibition prior to full induction. The coadministration/administration alone geometric mean ratio for the rifampin AUC(0-24) on day 14 was 1.07 (90% CI, 0.83-1.38). Nelfinavir does not meaningfully alter caspofungin pharmacokinetics. Rifampin both inhibits and induces caspofungin disposition, resulting in a reduced C(24hr) at steady state. An increase in the caspofungin dose to 70 mg, administered daily, should be considered when the drug is coadministered with rifampin. For more Interactions (Complete) data for CASPOFUNGIN (9 total), please visit the HSDB record page. |
| 参考文献 |
[1]. Flattery AM, et, al. Efficacy of caspofungin in a juvenile mouse model of central nervous system candidiasis. Antimicrob Agents Chemother. 2011 Jul;55(7):3491-7.
[2]. Mojumder DK, et, al. Evaluating retinal toxicity of intravitreal caspofungin in the mouse eye. Invest Ophthalmol Vis Sci. 2010 Nov;51(11):5796-803. [3]. Antimicrob Agents Chemother. 2002 Nov; 46(11): 3591–3596. [4]. Antimicrob Agents Chemother.1997 Nov;41(11):2326-32 |
| 其他信息 |
Caspofungin (brand name Cancidas worldwide) is an antifungal drug and the first member of a new drug class called the echinocandins, as coined by Merck & Co., Inc. It is typically administered intravenously. It shows activity against infections with Aspergillus and Candida, and works by inhibiting β(1,3)-D-Glucan of the fungal cell wall.
Caspofungin is an antimycotic echinocandin lipopeptide, semisynthetically derived from a fermentation product of the fungus Glarea lozoyensis. Caspofungin inhibits 1,3-beta-glucan synthase, resulting in decreased synthesis of beta(1,3)-D-glucan (an essential component of the fungal cell wall), weakening of the fungal cell wall, and fungal cell wall rupture. This agent is active against Aspergillus and Candida species. A cyclic lipopeptide echinocandin and beta-(1,3)-D-glucan synthase inhibitor that is used to treat internal or systemic MYCOSES. See also: Caspofungin (annotation moved to). Drug Indication For the treatment of esophageal candidiasis and invasive aspergillosis in patients who are refractory to or intolerant of other therapies. FDA Label Treatment of invasive candidiasis in adult or paediatric patients; treatment of invasive aspergillosis in adult or paediatric patients who are refractory to or intolerant of amphotericin B, lipid formulations of amphotericin B and / or itraconazole. Refractoriness is defined as progression of infection or failure to improve after a minimum of seven days of prior therapeutic doses of effective antifungal therapy; empirical therapy for presumed fungal infections (such as Candida or Aspergillus) in febrile, neutropaenic adult or paediatric patients. Treatment of invasive candidiasis in adult or paediatric patients. Treatment of invasive aspergillosis in adult or paediatric patients who are refractory to or intolerant of amphotericin B, lipid formulations of amphotericin B and/or itraconazole. Refractoriness is defined as progression of infection or failure to improve after a minimum of 7 days of prior therapeutic doses of effective antifungal therapy. Empirical therapy for presumed fungal infections (such as Candida or Aspergillus) in febrile, neutropaenic adult or paediatric patients. Mechanism of Action Caspofungin inhibits the synthesis of beta-(1,3)-D-glucan, an essential component of the cell wall of Aspergillus species and Candida species. beta-(1,3)-D-glucan is not present in mammalian cells. The primary target is beta-(1,3)-glucan synthase. Caspofungin inhibits the synthesis of beta(1,3)-d-glucan, an integral component of the fungal cell wall that is not present in mammalian cells. Caspofungin acetate ... /belongs to a class of drugs/ referred to as echinocandins, which inhibit the formation of beta(1,3)-D-glucans in the fungal cell wall. Resistance is conferred by mutations in the FKS1 gene, which codes for a large subunit of (1,3)beta-glucan synthase. /Caspofungin acetate/ Caspofungin acetate, the active ingredient of cancidas, inhibits the synthesis of alpha(1,3)-D-glucan, an essential component of the cell wall of susceptible Aspergillus species and Candida species. (1,3)-D-glucan is not present in mammalian cells. Caspofungin has shown activity against Candida species and in regions of active cell growth of the hyphae of Aspergillus fumigatus. /Caspofungin acetate/ Therapeutic Uses Caspofungin is indicated for the empirical therapy for presumed fungal infections in febrile, neutropenic patients. /Included in US product labeling/ Caspofungin is indicated for the treatment of candidemia and the following Candidiasis infections: esophageal, intra-abdominal and abscesses, peritonitis, and plural space infections. /Included in US product labeling/ Caspofungin is indicated in the tretment of invasive aspergillosis in patients who are refractory t or intolerant of other therapies, including amphotericin B (lipid and non-lipid formulations) and/or itraconazole. /Included in US product labeling/ /Expl Ther/ ... Azole-resistant isolates of Candida albicans remain susceptible to caspofungin ... /Caspofungin acetate/ is active in experimental animal infection with C. albicans, Aspergillus fumigatus, Pneumocystis carinii, and Histoplasma capsulatum. Clinical trials are in progress with iv formulations of caspofungin ... in patients with deep candidiasis, and with neutropenia and fever not responding to antibacterial therapy. /Caspofungin acetate/ For more Therapeutic Uses (Complete) data for CASPOFUNGIN (8 total), please visit the HSDB record page. Drug Warnings Adverse effects occurring in 2% or more of patients with invasive aspergillosis receiving caspofungin acetate in an open-label, noncomparative clinical study include fever, infused vein complications, nausea, vomiting, or flushing. Fever, phlebitis/thrombophlebitis, infused vein complication, headache, nausea, pain (unspecified), rash, anemia, abdominal pain, diarrhea, vomiting, facial edema, flu-like illness, myalgia, paresthesia, induration, chills, and pruritus reported in clinical studies for uses other than aspergillosis. The following postmarketing adverse events have been reported: Hepatobiliary: rare cases of clinically significant hepatic dysfunction Cardiovascular: swelling and peripheral edema Metabolic: hypercalcemia Possible histamine-mediated symptoms have been reported including reports of rash, facial swelling, pruritus, sensation of warmth, or bronchospasm. Anaphylaxis has been reported during administration of CANCIDAS. Caspofungin is distributed into milk in rats; not known whether caspofungin is distributed into milk in humans. Caution should be exercised if caspofungin is used in nursing women. For more Drug Warnings (Complete) data for CASPOFUNGIN (6 total), please visit the HSDB record page. Pharmacodynamics Caspofungin is an antifungal drug, and belongs to a new class termed the echinocandins. It is used to treat Aspergillus and Candida infection, and works by inhibiting cell wall synthesis. Antifungals in the echinocandin class inhibit the synthesis of glucan in the cell wall, probably via the enzyme 1,3-beta glucan synthase. There is a potential for resistance development to occur, however in vitro resistance development to Caspofungin by Aspergillus species has not been studied. |
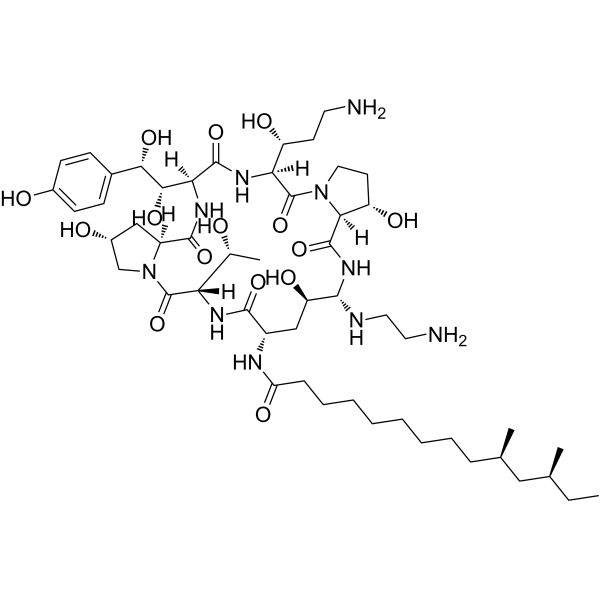
| 分子式 |
C52H88N10O15
|
|---|---|
| 分子量 |
1093.31
|
| 精确质量 |
1091.65
|
| 元素分析 |
C, 57.13; H, 8.11; N, 12.81; O, 21.95
|
| CAS号 |
162808-62-0
|
| 相关CAS号 |
Caspofungin diacetate;179463-17-3;Caspofungin-d4;1131958-73-0; 162808-62-0
|
| PubChem CID |
2826718
|
| 外观&性状 |
Typically exists as solid at room temperature
|
| 密度 |
1.36g/cm3
|
| 沸点 |
1408.1ºC at 760mmHg
|
| 闪点 |
805.4ºC
|
| 蒸汽压 |
0mmHg at 25°C
|
| 折射率 |
1.623
|
| LogP |
0.761
|
| tPSA |
400
|
| 氢键供体(HBD)数目 |
16
|
| 氢键受体(HBA)数目 |
18
|
| 可旋转键数目(RBC) |
23
|
| 重原子数目 |
77
|
| 分子复杂度/Complexity |
1900
|
| 定义原子立体中心数目 |
14
|
| SMILES |
CCC(CC(CCCCCCCCC(NC1CC(O)C(NC(C2C(O)CCN2C(C(NC(C(NC(C3CC(O)CN3C(C(NC1=O)C(O)C)=O)=O)C(O)C(O)C4=CC=C(O)C=C4)=O)C(O)CCN)=O)=O)NCCN)=O)C)C
|
| InChi Key |
JYIKNQVWKBUSNH-WVDDFWQHSA-N
|
| InChi Code |
InChI=1S/C52H88N10O15/c1-5-28(2)24-29(3)12-10-8-6-7-9-11-13-39(69)56-34-26-38(68)46(55-22-21-54)60-50(75)43-37(67)19-23-61(43)52(77)41(36(66)18-20-53)58-49(74)42(45(71)44(70)31-14-16-32(64)17-15-31)59-48(73)35-25-33(65)27-62(35)51(76)40(30(4)63)57-47(34)72/h14-17,28-30,33-38,40-46,55,63-68,70-71H,5-13,18-27,53-54H2,1-4H3,(H,56,69)(H,57,72)(H,58,74)(H,59,73)(H,60,75)/t28-,29+,30+,33+,34-,35-,36+,37-,38+,40-,41-,42-,43-,44-,45-,46-/m0/s1
|
| 化学名 |
(10R,12S)-N-((2R,6S,9S,11R,12S,14aS,15S,20S,23S,25aS)-20-((R)-3-amino-1-hydroxypropyl)-12-((2-aminoethyl)amino)-23-((1S,2S)-1,2-dihydroxy-2-(4-hydroxyphenyl)ethyl)-2,11,15-trihydroxy-6-((R)-1-hydroxyethyl)-5,8,14,19,22,25-hexaoxotetracosahydro-1H-dipyrrolo[2,1-c:2',1'-l][1,4,7,10,13,16]hexaazacyclohenicosin-9-yl)-10,12-dimethyltetradecanamide
|
| 别名 |
L 743872; MK0991; L743872; MK 0991; L-743872; MK-0991
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
May dissolve in DMSO (in most cases), if not, try other solvents such as H2O, Ethanol, or DMF with a minute amount of products to avoid loss of samples
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 0.9147 mL | 4.5733 mL | 9.1465 mL | |
| 5 mM | 0.1829 mL | 0.9147 mL | 1.8293 mL | |
| 10 mM | 0.0915 mL | 0.4573 mL | 0.9147 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。
Study of Rezafungin Compared to Caspofungin in Subjects With Candidemia and/or Invasive Candidiasis
CTID: NCT03667690
Phase: Phase 3 Status: Completed
Date: 2023-01-06