| 规格 | 价格 | 库存 | 数量 |
|---|---|---|---|
| 100mg |
|
||
| Other Sizes |
|
| 体外研究 (In Vitro) |
Cl 链霉素可降低通道活性和 Ca2+ 进入的有效部分[3]。
|
|---|---|
| 药代性质 (ADME/PK) |
Absorption, Distribution and Excretion
Due to poor oral absorption, aminoglycosides including streptomycin are administered parenterally. Streptomycin is available as an intramuscular injection, and in some cases may be administered intravenously. A peak serum concentration of 25-50 mcg/mL is achieved within 1 hour after intramuscular administration of 1 gram of streptomycin. Approximately 50% of streptomycin is eliminated in the urine within 24 hours after intravenous or intramuscular administration. Following intramuscular injection of 1 g of streptomycin as the sulfate, a peak serum level of 25 to 50 ug/mL is reached within 1 hour, diminishing slowly to about 50 percent after 5 to 6 hours. Appreciable concentrations are found in all organ tissues except the brain. Significant amounts have been found in pleural fluid and tuberculous cavities. Streptomycin passes through the placenta with serum levels in the cord blood similar to maternal levels. Small amounts are excreted in milk, saliva, and sweat. Streptomycin is not absorbed from the GI tract. Streptomycin is rapidly absorbed after IM injection. Following IM administration of a single 1-g dose of streptomycin in adults with normal renal function, peak serum streptomycin concentrations are attained within 1 hour and range from 25-50 ug/mL; serum concentrations decrease 50% by 5-6 hours after the dose. In one study in premature infants, mean peak serum concentrations of about 29 ug/mL were attained within 2 hours following IM administration of streptomycin 10-11 mg/kg; serum concentrations averaged 11 ug/mL at 12 hours. For more Absorption, Distribution and Excretion (Complete) data for Streptomycin (16 total), please visit the HSDB record page. Metabolism / Metabolites Aminoglycosides are not metabolized and are excreted unchanged in the urine primarily by glomerular filtration. /Aminoglycosides/ Biological Half-Life Streptomycins serum half-life is estimated to be 2.5 hours. The plasma elimination half-life of streptomycin is usually 2-3 hours in adults with normal renal function and has been reported to range up to 110 hours in adults with severe renal impairment. The plasma elimination half-life of streptomycin has been reported to range from 4-10 hours in premature and newborn infants. In patients with impaired hepatic and renal function, the plasma elimination half-life has been reported to be more prolonged than in patients with renal impairment alone. |
| 毒性/毒理 (Toxicokinetics/TK) |
Hepatotoxicity
Intravenous and intramuscular therapy with streptomycin has been linked to mild and asymptomatic elevations in serum alkaline phosphatase, but therapy rarely affects aminotransferase levels or bilirubin and changes typically resolve rapidly once streptomycin is stopped. Only isolated case reports of acute liver injury with jaundice have been associated with streptomycin therapy and always in combination with other antituberculosis medications which are more clearly hepatotoxic, such as isoniazid, pyrazinamide and rifampin. Streptomycin and the aminoglycosides are not mentioned in large case series of drug induced liver disease and acute liver failure; thus, hepatic injury from streptomycin must be exceedingly rare, if it occurs at all. Likelihood score: E (unlikely cause of clinically apparent liver injury). Effects During Pregnancy and Lactation ◉ Summary of Use during Lactation Similar to other aminoglycoside antibiotics, streptomycin is poorly excreted into breastmilk. Newborn infants apparently absorb small amounts of aminoglycosides, but serum levels are far below those attained when treating newborn infections and systemic effects of streptomycin are unlikely. Older infants would be expected to absorb even less streptomycin Monitor the infant for possible effects on the gastrointestinal flora, such as diarrhea, candidiasis (e.g., thrush, diaper rash) or rarely, blood in the stool indicating possible antibiotic-associated colitis. ◉ Effects in Breastfed Infants Relevant published information was not found as of the revision date. ◉ Effects on Lactation and Breastmilk One observational study found no inhibition of lactation by streptomycin. |
| 参考文献 | |
| 其他信息 |
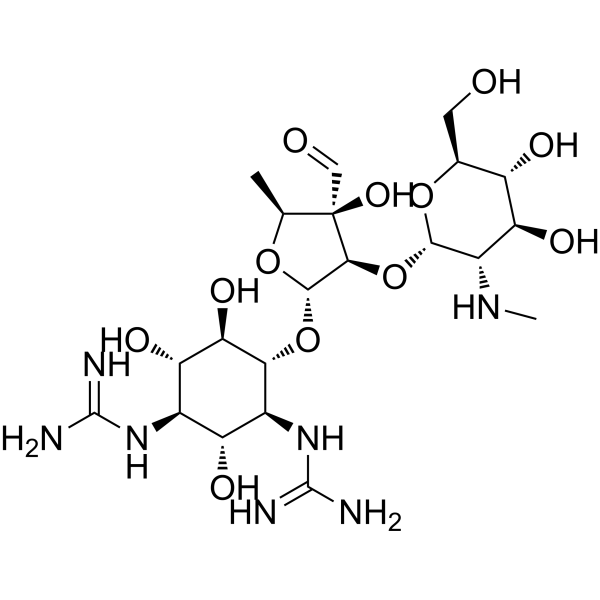
Streptomycin is a amino cyclitol glycoside that consists of streptidine having a disaccharyl moiety attached at the 4-position. The parent of the streptomycin class It has a role as an antimicrobial agent, an antimicrobial drug, an antibacterial drug, a protein synthesis inhibitor, a bacterial metabolite and an antifungal agrochemical. It is an antibiotic antifungal drug, an antibiotic fungicide and a member of streptomycins. It is functionally related to a streptidine. It is a conjugate base of a streptomycin(3+).
Streptomycin, an antibiotic derived from Streptomyces griseus, was the first aminoglycoside to be discovered and used in practice in the 1940s. Selman Waksman and eventually Albert Schatz were recognized with the Nobel Prize in Medicine for their discovery of streptomycin and its antibacterial activity. Although streptomycin was the first antibiotic determined to be effective against mycobacterium tuberculosis, it has fallen out of favor due to resistance and is now primarily used as adjunctive treatment in cases of multi-drug resistant tuberculosis. Streptomycin is an Aminoglycoside Antibacterial and Antimycobacterial. Streptomycin is a broad spectrum aminoglycoside antibiotic typically used for treatment of active tuberculosis, always in combination with other antituberculosis agents. Streptomycin is usually used in combination with agents that are known to be hepatotoxic and the role of streptomycin in liver injury has been difficult to assess, but most information suggests that streptomycin is not hepatotoxic. Streptomycin has been reported in Lyngbya majuscula, Senecio, and other organisms with data available. Streptomycin is an aminoglycoside antibiotic derived from Streptomyces griseus with antibacterial activity. Streptomycin irreversibly binds to the 16S rRNA and S12 protein within the bacterial 30S ribosomal subunit. As a result, this agent interferes with the assembly of initiation complex between mRNA and the bacterial ribosome, thereby inhibiting the initiation of protein synthesis. In addition, streptomycin induces misreading of the mRNA template and causes translational frameshift, thereby results in premature termination. This eventually leads to bacterial cell death. An antibiotic produced by the soil actinomycete Streptomyces griseus. It acts by inhibiting the initiation and elongation processes during protein synthesis. See also: Streptomycin Sulfate (has salt form); Streptomycin pantothenate (is active moiety of); Streptomycin hydrochloride (is active moiety of). Drug Indication Although streptomycin was the first antibiotic available for the treatment of mycobacterium tuberculosis, it is now largely a second line option due to resistance and toxicity. Streptomycin may also be used to treat a variety of other infections caused by susceptible strains of aerobic bacteria where other less toxic agents are ineffective. Examples include: _Yersinia pestis_, _Francisella tularensis_, _Brucella_, _Calymmatobacterium granulomatis_ (donovanosis, granuloma inguinale), _H. ducreyi_ (chancroid), _H. influenzae_ (in respiratory, endocardial, and meningeal infections - concomitantly with another antibacterial agents). _K. pneumoniae_ pneumonia (concomitantly with another antibacterial agent), _E.coli_, _Proteus_, _A.aerogenes_, _K. pneumoniae_, and _Enterococcus faecalis_ in urinary tract infections, _Streptococcus viridans_, _Enterococcus faecalis_ (in endocardial infections - concomitantly with penicillin), and Gram-negative bacillary bacteremia (concomitantly with another antibacterial agent). Mechanism of Action There are 3 key phases of aminoglycoside entry into cells. The first “ionic binding phase” occurs when polycationic aminoglycosides bind electrostatically to negatively charged components of bacterial cell membranes including with lipopolysaccharides and phospholipids within the outer membrane of Gram-negative bacteria and to teichoic acids and phospholipids within the cell membrane of Gram-positive bacteria. This binding results in displacement of divalent cations and increased membrane permeability, allowing for aminoglycoside entry. The second “energy-dependent phase I” of aminoglycoside entry into the cytoplasm relies on the proton-motive force and allows a limited amount of aminoglycoside access to its primary intracellular target - the bacterial 30S ribosome. This ultimately results in the mistranslation of proteins and disruption of the cytoplasmic membrane. Finally, in the “energy-dependent phase II” stage, concentration-dependent bacterial killing is observed. Aminoglycoside rapidly accumulates in the cell due to the damaged cytoplasmic membrane, and protein mistranslation and synthesis inhibition is amplified. Hence, aminoglycosides have both immediate bactericidal effects through membrane disruption and delayed bactericidal effects through impaired protein synthesis; observed experimental data and mathematical modeling support this two-mechanism model. Inhibition of protein synthesis is a key component of aminoglycoside efficacy. Structural and cell biological studies suggest that aminoglycosides bind to the 16S rRNA in helix 44 (h44), near the A site of the 30S ribosomal subunit, altering interactions between h44 and h45. This binding also displaces two important residues, A1492 and A1493, from h44, mimicking normal conformational changes that occur with successful codon-anticodon pairing in the A site. Overall, aminoglycoside binding has several negative effects including inhibition of translation, initiation, elongation, and ribosome recycling. Recent evidence suggests that the latter effect is due to a cryptic second binding site situated in h69 of the 23S rRNA of the 50S ribosomal subunit. Also, by stabilizing a conformation that mimics correct codon-anticodon pairing, aminoglycosides promote error-prone translation. Mistranslated proteins can incorporate into the cell membrane, inducing the damage discussed above. The primary intracellular site of action of the aminoglycosides is the 30 S ribosomal subunit, which consists of 21 proteins and a single 16 S molecule of RNA. at least three of these proteins and perhaps the 16 S ribosomal RNA as well contribute to the streptomycin binding site, and alterations of these molecules markedly affect the binding and subsequent action of streptomycin. For example, a single amino acid substitution of asparagine for lysine at position 42 of one ribosomal protein (S12) prevents binding of the drug; the resultant mutant is totally resistant to streptomycin. Another mutant, in which glutamine is the amino acid at this position, is dependent on streptomycin. During protein synthesis, the ribosome selects aminoacyl-transfer RNAs with anticodons matching the messenger RNA codon present in the A site of the small ribosomal subunit. The aminoglycoside antibiotic streptomycin disrupts decoding by binding close to the site of codon recognition. Here we use X-ray crystallography to define the impact of streptomycin on the decoding site of the Thermus thermophilus 30S ribosomal subunit in complexes with cognate or near-cognate anticodon stem-loop analogues and messenger RNA. Our crystal structures display a significant local distortion of 16S ribosomal RNA induced by streptomycin, including the crucial bases A1492 and A1493 that participate directly in codon recognition. Consistent with kinetic data, we observe that streptomycin stabilizes the near-cognate anticodon stem-loop analogue complex, while destabilizing the cognate anticodon stem-loop analogue complex. These data reveal how streptomycin disrupts the recognition of cognate anticodon stem-loop analogues and yet improves recognition of a near-cognate anticodon stem-loop analogue. The antibiotic streptomycin is widely used in the treatment of microbial infections. The primary mechanism of action is inhibition of translation by binding to the ribosome, ... .Early in the study of this antibiotic, a mysterious streptomycin-induced potassium efflux preceding any decrease in viability was observed; it was speculated that this changed the electrochemical gradient such that streptomycin better accessed the cytoplasm. Here we use a high-throughput screen to search for compounds targeting the mechanosensitive channel of large conductance (MscL) and find dihydrostreptomycin among the 'hits'. Furthermore, we find that MscL is not only necessary for the previously described streptomycin-induced potassium efflux, but also directly increases MscL activity in electrophysiological studies. The data suggest that gating MscL is a novel mode of action of dihydrostreptomycin, and that MscL's large pore may provide a mechanism for cell entry. ... Aminoglycosides are aminocyclitols that kill bacteria by inhibiting protein synthesis as they bind to the 16S rRNA and by disrupting the integrity of bacterial cell membrane. Aminoglycoside resistance mechanisms include: (a) the deactivation of aminoglycosides by N-acetylation, adenylylation or O-phosphorylation, (b) the reduction of the intracellular concentration of aminoglycosides by changes in outer membrane permeability, decreased inner membrane transport, active efflux, and drug trapping, (c) the alteration of the 30S ribosomal subunit target by mutation, and (d) methylation of the aminoglycoside binding site. ... /Aminoglycosides/ |
| 分子式 |
C21H39N7O12
|
|---|---|
| 分子量 |
581.57
|
| 精确质量 |
581.265
|
| CAS号 |
57-92-1
|
| 相关CAS号 |
Streptomycin sulfate;3810-74-0;Penicillin G;61-33-6
|
| PubChem CID |
19649
|
| 外观&性状 |
White to off-white solid powder
|
| 密度 |
2.0±0.1 g/cm3
|
| 沸点 |
872.9±75.0 °C at 760 mmHg
|
| 熔点 |
MW: 1457.383. Powder. MP: aproximately 230 °C /Streptomycin sulfate; 3810-74-0/
|
| 闪点 |
481.7±37.1 °C
|
| 蒸汽压 |
0.0±0.6 mmHg at 25°C
|
| 折射率 |
1.762
|
| LogP |
-2.53
|
| tPSA |
331.43
|
| 氢键供体(HBD)数目 |
12
|
| 氢键受体(HBA)数目 |
15
|
| 可旋转键数目(RBC) |
9
|
| 重原子数目 |
40
|
| 分子复杂度/Complexity |
940
|
| 定义原子立体中心数目 |
15
|
| SMILES |
C[C@H]1[C@@]([C@H]([C@@H](O1)O[C@@H]2[C@H]([C@@H]([C@H]([C@@H]([C@H]2O)O)N=C(N)N)O)N=C(N)N)O[C@H]3[C@H]([C@@H]([C@H]([C@@H](O3)CO)O)O)NC)(C=O)O
|
| InChi Key |
UCSJYZPVAKXKNQ-HZYVHMACSA-N
|
| InChi Code |
InChI=1S/C21H39N7O12/c1-5-21(36,4-30)16(40-17-9(26-2)13(34)10(31)6(3-29)38-17)18(37-5)39-15-8(28-20(24)25)11(32)7(27-19(22)23)12(33)14(15)35/h4-18,26,29,31-36H,3H2,1-2H3,(H4,22,23,27)(H4,24,25,28)/t5-,6-,7+,8-,9-,10-,11+,12-,13-,14+,15+,16-,17-,18-,21+/m0/s1
|
| 化学名 |
2-[(1R,2R,3S,4R,5R,6S)-3-(diaminomethylideneamino)-4-[(2R,3R,4R,5S)-3-[(2S,3S,4S,5R,6S)-4,5-dihydroxy-6-(hydroxymethyl)-3-(methylamino)oxan-2-yl]oxy-4-formyl-4-hydroxy-5-methyloxolan-2-yl]oxy-2,5,6-trihydroxycyclohexyl]guanidine
|
| HS Tariff Code |
2934.99.9001
|
| 存储方式 |
Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month |
| 运输条件 |
Room temperature (This product is stable at ambient temperature for a few days during ordinary shipping and time spent in Customs)
|
| 溶解度 (体外实验) |
H2O : ~125 mg/mL (~214.94 mM)
|
|---|---|
| 溶解度 (体内实验) |
注意: 如下所列的是一些常用的体内动物实验溶解配方,主要用于溶解难溶或不溶于水的产品(水溶度<1 mg/mL)。 建议您先取少量样品进行尝试,如该配方可行,再根据实验需求增加样品量。
注射用配方
注射用配方1: DMSO : Tween 80: Saline = 10 : 5 : 85 (如: 100 μL DMSO → 50 μL Tween 80 → 850 μL Saline)(IP/IV/IM/SC等) *生理盐水/Saline的制备:将0.9g氯化钠/NaCl溶解在100 mL ddH ₂ O中,得到澄清溶液。 注射用配方 2: DMSO : PEG300 :Tween 80 : Saline = 10 : 40 : 5 : 45 (如: 100 μL DMSO → 400 μL PEG300 → 50 μL Tween 80 → 450 μL Saline) 注射用配方 3: DMSO : Corn oil = 10 : 90 (如: 100 μL DMSO → 900 μL Corn oil) 示例: 以注射用配方 3 (DMSO : Corn oil = 10 : 90) 为例说明, 如果要配制 1 mL 2.5 mg/mL的工作液, 您可以取 100 μL 25 mg/mL 澄清的 DMSO 储备液,加到 900 μL Corn oil/玉米油中, 混合均匀。 View More
注射用配方 4: DMSO : 20% SBE-β-CD in Saline = 10 : 90 [如:100 μL DMSO → 900 μL (20% SBE-β-CD in Saline)] 口服配方
口服配方 1: 悬浮于0.5% CMC Na (羧甲基纤维素钠) 口服配方 2: 悬浮于0.5% Carboxymethyl cellulose (羧甲基纤维素) 示例: 以口服配方 1 (悬浮于 0.5% CMC Na)为例说明, 如果要配制 100 mL 2.5 mg/mL 的工作液, 您可以先取0.5g CMC Na并将其溶解于100mL ddH2O中,得到0.5%CMC-Na澄清溶液;然后将250 mg待测化合物加到100 mL前述 0.5%CMC Na溶液中,得到悬浮液。 View More
口服配方 3: 溶解于 PEG400 (聚乙二醇400) 请根据您的实验动物和给药方式选择适当的溶解配方/方案: 1、请先配制澄清的储备液(如:用DMSO配置50 或 100 mg/mL母液(储备液)); 2、取适量母液,按从左到右的顺序依次添加助溶剂,澄清后再加入下一助溶剂。以 下列配方为例说明 (注意此配方只用于说明,并不一定代表此产品 的实际溶解配方): 10% DMSO → 40% PEG300 → 5% Tween-80 → 45% ddH2O (或 saline); 假设最终工作液的体积为 1 mL, 浓度为5 mg/mL: 取 100 μL 50 mg/mL 的澄清 DMSO 储备液加到 400 μL PEG300 中,混合均匀/澄清;向上述体系中加入50 μL Tween-80,混合均匀/澄清;然后继续加入450 μL ddH2O (或 saline)定容至 1 mL; 3、溶剂前显示的百分比是指该溶剂在最终溶液/工作液中的体积所占比例; 4、 如产品在配制过程中出现沉淀/析出,可通过加热(≤50℃)或超声的方式助溶; 5、为保证最佳实验结果,工作液请现配现用! 6、如不确定怎么将母液配置成体内动物实验的工作液,请查看说明书或联系我们; 7、 以上所有助溶剂都可在 Invivochem.cn网站购买。 |
| 制备储备液 | 1 mg | 5 mg | 10 mg | |
| 1 mM | 1.7195 mL | 8.5974 mL | 17.1948 mL | |
| 5 mM | 0.3439 mL | 1.7195 mL | 3.4390 mL | |
| 10 mM | 0.1719 mL | 0.8597 mL | 1.7195 mL |
1、根据实验需要选择合适的溶剂配制储备液 (母液):对于大多数产品,InvivoChem推荐用DMSO配置母液 (比如:5、10、20mM或者10、20、50 mg/mL浓度),个别水溶性高的产品可直接溶于水。产品在DMSO 、水或其他溶剂中的具体溶解度详见上”溶解度 (体外)”部分;
2、如果您找不到您想要的溶解度信息,或者很难将产品溶解在溶液中,请联系我们;
3、建议使用下列计算器进行相关计算(摩尔浓度计算器、稀释计算器、分子量计算器、重组计算器等);
4、母液配好之后,将其分装到常规用量,并储存在-20°C或-80°C,尽量减少反复冻融循环。
计算结果:
工作液浓度: mg/mL;
DMSO母液配制方法: mg 药物溶于 μL DMSO溶液(母液浓度 mg/mL)。如该浓度超过该批次药物DMSO溶解度,请首先与我们联系。
体内配方配制方法:取 μL DMSO母液,加入 μL PEG300,混匀澄清后加入μL Tween 80,混匀澄清后加入 μL ddH2O,混匀澄清。
(1) 请确保溶液澄清之后,再加入下一种溶剂 (助溶剂) 。可利用涡旋、超声或水浴加热等方法助溶;
(2) 一定要按顺序加入溶剂 (助溶剂) 。